J Korean Orthop Assoc.
2016 Feb;51(1):30-39. 10.4055/jkoa.2016.51.1.30.
Surgical Correction of Adult Spinal Deformity
- Affiliations
-
- 1Department of Orthopaedic Surgery, Kyung Hee University School of Medicine, Seoul, Korea. futurespine@gmail.com
- KMID: 2154346
- DOI: http://doi.org/10.4055/jkoa.2016.51.1.30
Abstract
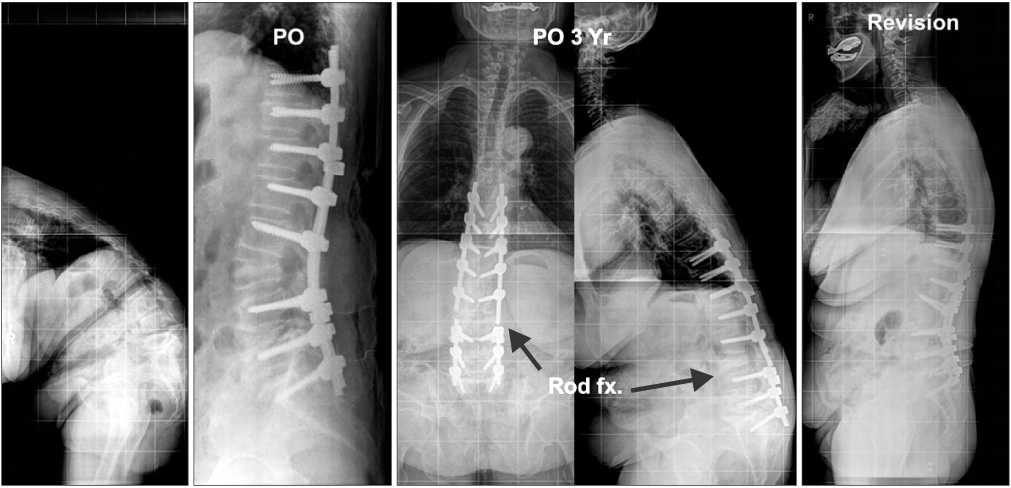
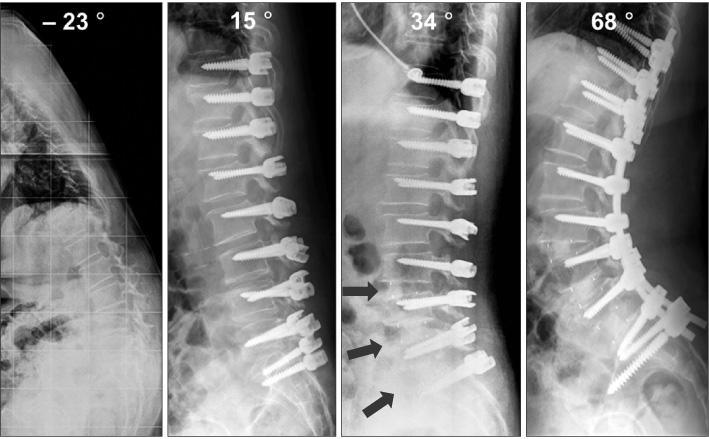
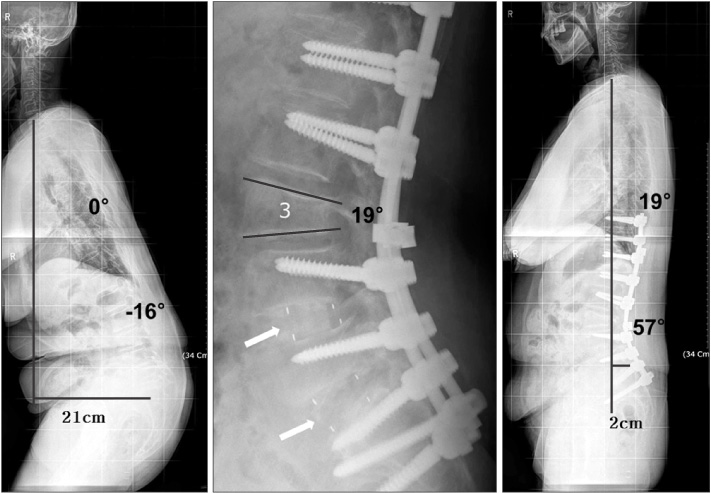
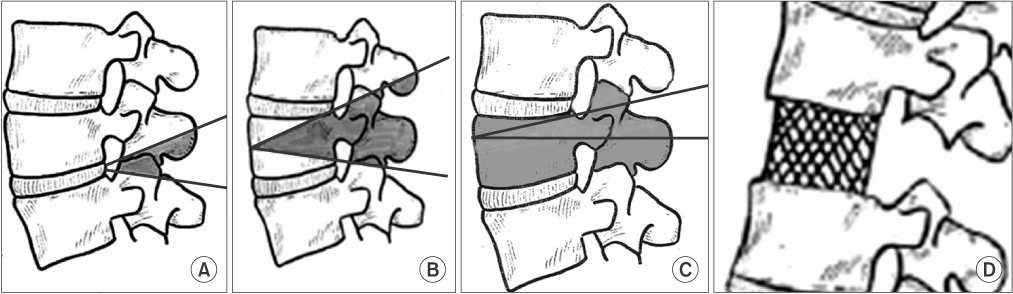
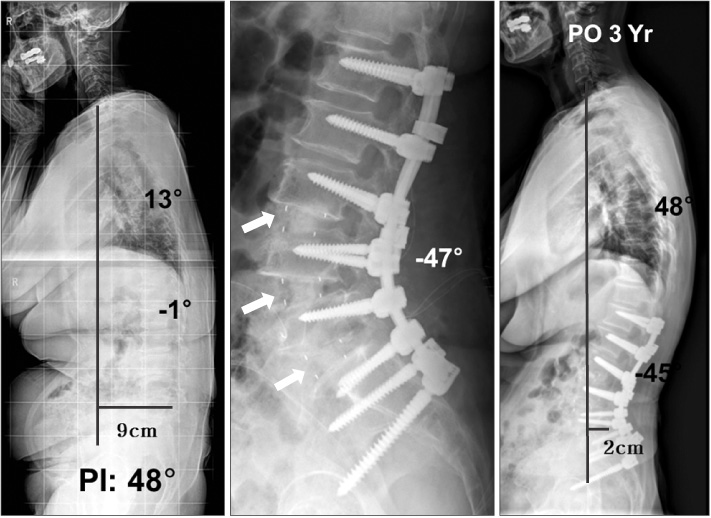
- Surgical correction of adult spinal deformity is a challenge, and is physically and mentally demanding for spinal surgeons. For satisfactory surgical outcomes, proper patient selection is fundamental and preoperative detailed physical examination, intra-operative neuromonitoring, and collaboration with anesthesiology or internal medicine department are critical for prevention of peri-operative complications associated with surgical treatments. A posterior-only or anterior-posterior combined approach can be used. Considering the patients' hemodynamic status or long-time anesthesia, surgeons can decide whether to operate by stage or one stage. Deformity correction can be performed using spinal osteotomy or anterior interbody fusion. Decision regarding correction method depends on the patient's condition and correction degree or level. In this review, the authors try to help in decision making with regard to deformity correction methods for ideal surgical technique, correction angle, fusion length etc. in reference to previous literature.
MeSH Terms
Figure
Reference
-
1. Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976). 2005; 30:2024–2029.
Article2. Auerbach JD, Lenke LG, Bridwell KH, et al. Major complications and comparison between 3-column osteotomy techniques in 105 consecutive spinal deformity procedures. Spine (Phila Pa 1976). 2012; 37:1198–1210.
Article3. Lee CS, Chung SS, Shin SK, Park SJ, Lee HI, Kang KC. Differences in post-operative functional disability and patient satisfaction between patients with long (three levels or more) and short (less than three) lumbar fusions. J Bone Joint Surg Br. 2011; 93:1400–1404.
Article4. Gill JB, Levin A, Burd T, Longley M. Corrective osteotomies in spine surgery. J Bone Joint Surg Am. 2008; 90:2509–2520.
Article5. Kim KT, Lee SH, Suk KS, Lee JH, Jeong BO. Outcome of pedicle subtraction osteotomies for fixed sagittal imbalance of multiple etiologies: a retrospective review of 140 patients. Spine (Phila Pa 1976). 2012; 37:1667–1675.6. Hu SS, Berven SH. Preparing the adult deformity patient for spinal surgery. Spine (Phila Pa 1976). 2006; 31:S126–S131.
Article7. Pateder DB, Kebaish KM, Cascio BM, Neubaeur P, Matusz DM, Kostuik JP. Posterior only versus combined anterior and posterior approaches to lumbar scoliosis in adults: a radiographic analysis. Spine (Phila Pa 1976). 2007; 32:1551–1554.8. Crandall DG, Revella J. Transforaminal lumbar interbody fusion versus anterior lumbar interbody fusion as an adjunct to posterior instrumented correction of degenerative lumbar scoliosis: three year clinical and radiographic outcomes. Spine (Phila Pa 1976). 2009; 34:2126–2133.9. O'neill KR, Lenke LG, Bridwell KH, et al. Clinical and radiographic outcomes after 3-column osteotomies with 5-year follow-up. Spine (Phila Pa 1976). 2014; 39:424–432.10. Cho SK, Bridwell KH, Lenke LG, et al. Major complications in revision adult deformity surgery: risk factors and clinical outcomes with 2- to 7-year follow-up. Spine (Phila Pa 1976). 2012; 37:489–500.11. Shufflebarger HL, Grimm JO, Bui V, Thomson JD. Anterior and posterior spinal fusion. Staged versus same-day surgery. Spine (Phila Pa 1976). 1991; 16:930–933.
Article12. Rhee JM, Bridwell KH, Lenke LG, et al. Staged posterior surgery for severe adult spinal deformity. Spine (Phila Pa 1976). 2003; 28:2116–2121.
Article13. Tsirikos AI, Chang WN, Dabney KW, Miller F. Comparison of one-stage versus two-stage anteroposterior spinal fusion in pediatric patients with cerebral palsy and neuromuscular scoliosis. Spine (Phila Pa 1976). 2003; 28:1300–1305.
Article14. Dorward IG, Lenke LG, Bridwell KH, et al. Transforaminal versus anterior lumbar interbody fusion in long deformity constructs: a matched cohort analysis. Spine (Phila Pa 1976). 2013; 38:E755–E762.15. Hsieh PC, Koski TR, O'Shaughnessy BA, et al. Anterior lumbar interbody fusion in comparison with transforaminal lumbar interbody fusion: implications for the restoration of foraminal height, local disc angle, lumbar lordosis, and sagittal balance. J Neurosurg Spine. 2007; 7:379–386.
Article16. Schwab F, Blondel B, Chay E, et al. The comprehensive anatomical spinal osteotomy classification. Neurosurgery. 2014; 74:112–120. discussion 120
Article17. Geck MJ, Macagno A, Ponte A, Shufflebarger HL. The Ponte procedure: posterior only treatment of Scheuermann's kyphosis using segmental posterior shortening and pedicle screw instrumentation. J Spinal Disord Tech. 2007; 20:586–593.18. Lehmer SM, Keppler L, Biscup RS, Enker P, Miller SD, Steffee AD. Posterior transvertebral osteotomy for adult thoracolumbar kyphosis. Spine (Phila Pa 1976). 1994; 19:2060–2067.
Article19. Kim KT, Park DH, Lee SH, Suk KS, Lee JH, Park KJ. Partial pedicle subtraction osteotomy as an alternative option for spinal sagittal deformity correction. Spine (Phila Pa 1976). 2013; 38:1238–1243.
Article20. Chang KW, Tu MY, Huang HH, Chen HC, Chen YY, Lin CC. Posterior correction and fixation without anterior fusion for pseudoarthrosis with kyphotic deformity in ankylosing spondylitis. Spine (Phila Pa 1976). 2006; 31:E408–E413.
Article21. Ploumis A, Simpson AK, Cha TD, Herzog JP, Wood KB. Coronal spinal balance in adult spine deformity patients with long spinal fusions: a minimum 2- to 5-year follow-up study. J Spinal Disord Tech. 2015; 28:341–347.22. Lee SH, Kim KT, Suk KS, Lee JH, Seo EM, Huh DS. Sagittal decompensation after corrective osteotomy for lumbar degenerative kyphosis: classification and risk factors. Spine (Phila Pa 1976). 2011; 36:E538–E544.23. Schwab F, Patel A, Ungar B, Farcy JP, Lafage V. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976). 2010; 35:2224–2231.24. Suk KS, Kim KT, Lee SH, Kim JM. Significance of chin-brow vertical angle in correction of kyphotic deformity of ankylosing spondylitis patients. Spine (Phila Pa 1976). 2003; 28:2001–2005.
Article25. Gertzbein SD, Harris MB. Wedge osteotomy for the correction of post-traumatic kyphosis. A new technique and a report of three cases. Spine (Phila Pa 1976). 1992; 17:374–379.26. Ondra SL, Marzouk S, Koski T, Silva F, Salehi S. Mathematical calculation of pedicle subtraction osteotomy size to allow precision correction of fixed sagittal deformity. Spine (Phila Pa 1976). 2006; 31:E973–E979.
Article27. Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G. An analysis of sagittal spinal alignment following long adult lumbar instrumentation and fusion to L5 or S1: can we predict ideal lumbar lordosis? Spine (Phila Pa 1976). 2006; 31:2343–2352.
Article28. Rothenfluh DA, Mueller DA, Rothenfluh E, Min K. Pelvic incidence-lumbar lordosis mismatch predisposes to adjacent segment disease after lumbar spinal fusion. Eur Spine J. 2015; 24:1251–1258.
Article29. Lau D, Clark AJ, Scheer JK, et al. Proximal junctional kyphosis and failure after spinal deformity surgery: a systematic review of the literature as a background to classification development. Spine (Phila Pa 1976). 2014; 39:2093–2102.30. Chang DG, Ha KY, Kim YH, Lee EW. Spinopelvic alignment by different surgical methods in the treatment of degenerative sagittal imbalance of the lumbar spine. J Spinal Disord Tech. 2014; 12. 30. Published online. DOI: 10.1097/BSD.0000000000000239.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ankylosing Spondylitis: Prevention And Surgical Correction Of Deformity
- Etiology, diagnosis, and treatment of iatrogenic spinal deformity
- Cervical Spine Deformity Correction Techniques
- Diagnosis and treatment of adult spinal deformity
- Surgical Management of Recurrent Plexiform Neurofibroma in a Pediatric Patient with Severe Cervical Kyphotic Deformity: A Case Report