Anesth Pain Med.
2019 Jan;14(1):54-62. 10.17085/apm.2019.14.1.54.
Safety of blood mixture transfusion by rapid infusion device in liver transplantation recipients
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. lucid80@gmail.com
- KMID: 2434200
- DOI: http://doi.org/10.17085/apm.2019.14.1.54
Abstract
- BACKGROUND
Information on biochemical changes following rapid transfusion of blood mixtures in liver transplantation patients is limited.
METHODS
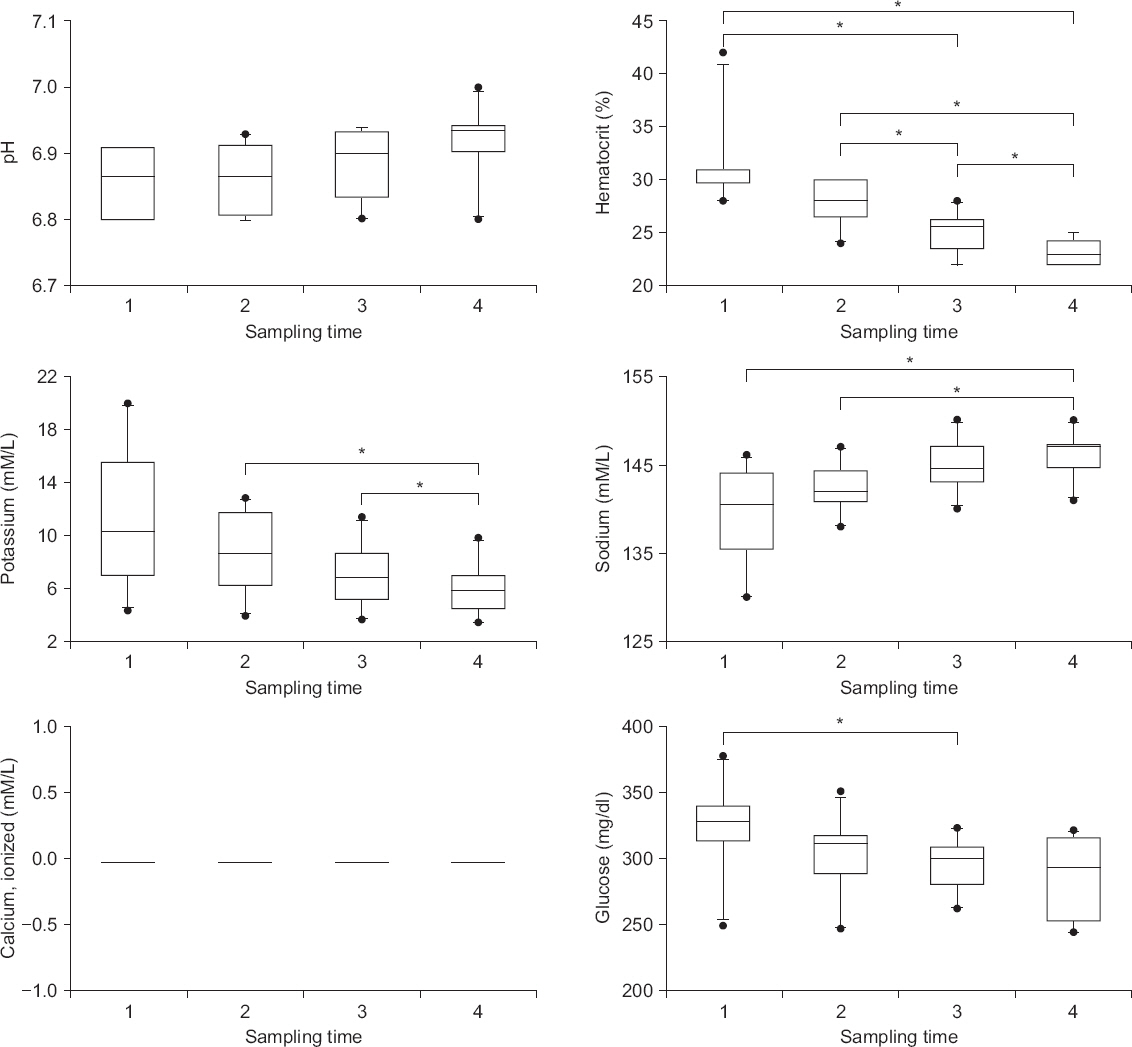
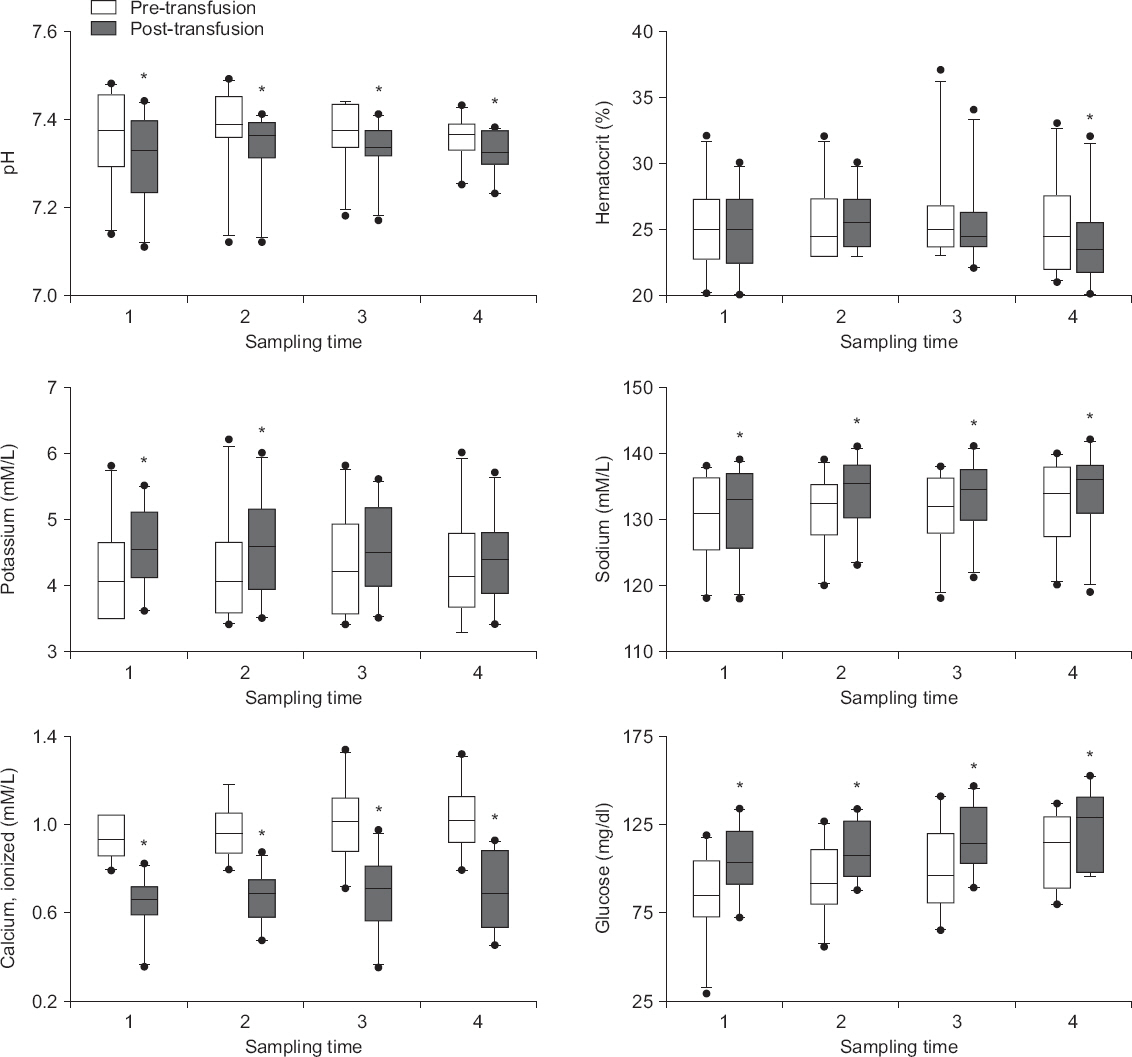
A blood mixture composed of red blood cells, fresh frozen plasma, and 0.9% saline was prepared in a ratio of 1 unit:1 unit:250 ml. During massive hemorrhage, 300 ml of the blood mixture was repeatedly transfused. A blood mixture sample as well as pre- and post-transfusion arterial blood samples were collected at the first, third, fifth, and seventh bolus transfusions. Changes in pH, hematocrit, electrolytes, and glucose were measured with a point-of-care analyzer. The biochemical changes were described, and the factors driving the changes were sought through linear mixed effects analysis.
RESULTS
A total of 120 blood samples from 10 recipients were examined. Potassium and sodium levels became normalized during preservation. Biochemical changes in the blood mixture were significantly related to the duration of blood bank storage and reservoir preservation (average R2 = 0.41). Acute acidosis and hypocalcemia requiring immediate correction occurred with each transfusion. Both the pre-transfusion value of the patient and the blood mixture value were significant predictors of post-transfusion changes in the body (average R2 = 0.87); however, the former was more crucial.
CONCLUSIONS
Rapid infusion of blood mixture is relatively safe because favorable biochemical changes occur during storage in the reservoir, and the composition of the blood mixture has little effect on the body during rapid transfusion in liver recipients. However, acute hypocalcemia and acidosis requiring immediate correction occurred frequently due to limited citrate metabolism in the liver recipients.
MeSH Terms
Figure
Reference
-
1. Yost CS, Niemann CU. Anesthesia for abdominal organ transplantation. Miller's anesthesia. 7th ed. Miller RD, editor. Philadelphia: Churchill Livingstone;2009. p. 2155–84.2. Pinsky MR, Grenuik A, Gordon RD, Starzl TE. Intensive care of liver transplant patients. Critical Care. Civetta J, Kirby R, Taylor R, editors. Philadelphia: JB Lippincott Company;1987.3. Kramer L, Bauer E, Joukhadar C, Strobl W, Gendo A, Madl C, et al. Citrate pharmacokinetics and metabolism in cirrhotic and noncirrhotic critically ill patients. Crit Care Med. 2003; 31:2450–5. DOI: 10.1097/01.CCM.0000084871.76568.E6. PMID: 14530750.4. Chung HS, Cho SJ, Park CS. Effects of liver function on ionized hypocalcaemia following rapid blood transfusion. J Int Med Res. 2012; 40:572–82. DOI: 10.1177/147323001204000219. PMID: 22613418.5. Hillyer CD, Tiegerman KO, Berkman EM. Evaluation of the red cell storage lesion after irradiation in filtered packed red cell units. Transfusion. 1991; 31:497–9. DOI: 10.1046/j.1537-2995.1991.31691306244.x. PMID: 1853441.6. Abbasoglu O, Goldstein RM, Vodapally MS, Jennings LW, Levy MF, Husberg BS, et al. Liver transplantation in hyponatremic patients with emphasis on central pontine myelinolysis. Clin Transplant. 1998; 12:263–9. PMID: 9642521.7. Cronbaugh R, Ploessl J, Sutton R, Martin M. Evaluation of a rapid infusion system. J Extra Corpor Technol. 1994; 26:200–4. PMID: 10150685.8. Nakagawa S, Schielzeth H. A general and simple method for obtaining R2 from generalized linear mixed-effects models. Methods Ecol Evol. 2013; 4:133–42. DOI: 10.1111/j.2041-210x.2012.00261.x.9. Moore GL, Peck CC, Sohmer PR, Zuck TF. Some properties of blood stored in anticoagulant CPDA-1 solution. A brief summary. Transfusion. 1981; 21:135–7. DOI: 10.1046/j.1537-2995.1981.21281178147.x. PMID: 7222197.10. Smith HM, Farrow SJ, Ackerman JD, Stubbs JR, Sprung J. Cardiac arrests associated with hyperkalemia during red blood cell transfusion: a case series. Anesth Analg. 2008; 106:1062–9. DOI: 10.1213/ane.0b013e318164f03d. PMID: 18349174.11. Xia VW, Ghobrial RM, Du B, Chen T, Hu KQ, Hiatt JR, et al. Predictors of hyperkalemia in the prereperfusion, early postreperfusion, and late postreperfusion periods during adult liver transplantation. Anesth Analg. 2007; 105:780–5. DOI: 10.1213/01.ane.0000271914.54261.17. PMID: 17717240.12. Morgan JP, Perreault CL, Morgan KG. The cellular basis of contraction and relaxation in cardiac and vascular smooth muscle. Am Heart J. 1991; 121:961–8. DOI: 10.1016/0002-8703(91)90227-9.13. Ewalenko P, Deloof T, Peeters J. Composition of fresh frozen plasma. Crit Care Med. 1986; 14:145–6. DOI: 10.1097/00003246-198602000-00015. PMID: 3943320.14. Atchison SR, Rettke SR, Fromme GA, Janossy TA, Kunkel SE, Williamson KR, et al. Plasma glucose concentrations during liver transplantation. Mayo Clin Proc. 1989; 64:241–5. DOI: 10.1016/S0025-6196(12)65679-1.15. Cheng KW, Chen CL, Cheng YF, Tseng CC, Wang CH, Chen YS, et al. Dextrose in the banked blood products does not seem to affect the blood glucose levels in patients undergoing liver transplantation. World J Gastroenterol. 2005; 11:2789–91. DOI: 10.3748/wjg.v11.i18.2789. PMID: 15884124. PMCID: PMC4305918.16. Miller A, Green M, Robinson D. Simple rule for calculating normal erythrocyte sedimentation rate. Br Med J (Clin Res Ed). 1983; 286:266. DOI: 10.1136/bmj.286.6361.266.17. Wetteland P, Røger M, Solberg HE, Iversen OH. Population-based erythrocyte sedimentation rates in 3910 subjectively healthy Norwegian adults. A statistical study based on men and women from the Oslo area. J Intern Med. 1996; 240:125–31. DOI: 10.1046/j.1365-2796.1996.30295851000.x. PMID: 8862121.18. Miller RD. Transfusion therapy. Miller's anesthesia. 7th ed. Miller RD, editor. Philadelphia: Churchill Livingstone;2009. p. 1739–93.19. Buchholz DH, Borgia JF, Ward M, Miripol JE, Simpson JM. Comparison of Adsol and CPDA-1 blood preservatives during simulated massive resuscitation after hemorrhage in swine. Transfusion. 1999; 39:998–1004. DOI: 10.1046/j.1537-2995.1999.39090998.x. PMID: 10533827.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Transfusion status in liver and kidney transplantation recipients: results from nationwide claims database
- Assessment of patient safety and the efficiency of facility utilization following simplified ultra-rapid intravenous infusion of hepatitis B immunoglobulin in a high-volume liver transplantation center
- Experience in Establishing Department of Transfusion Management
- Liver Failure Has Higher IgG ABO Blood Group Isoagglutinin Titer than Kidney Failure
- Unexpected Massive Bleeding during Liver Transplantation in Patients with Budd-Chiari Syndrome: A case report