Anesth Pain Med.
2019 Jan;14(1):48-53. 10.17085/apm.2019.14.1.48.
Successful case of veno-venous extracorporeal membrane oxygenation in an abdominal trauma patient: A case report
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea. jy67925@naver.com
- KMID: 2434199
- DOI: http://doi.org/10.17085/apm.2019.14.1.48
Abstract
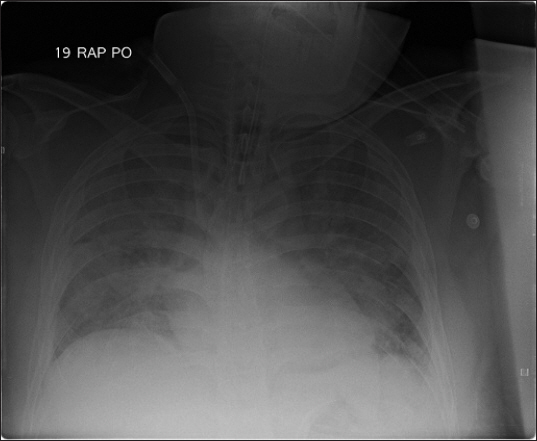
- A 37-year-old male visited the hospital with multiple trauma after traffic accident. Fractures of ribs, left femur, and right humerus and spleen rupture with hemoperitoneum were founded on image studies. He was moved to operation room and general anesthesia was performed for splenectomy. During the operation, excessive high peak inspiratory pressure was observed. After abdominal closure, hypoxia, hypercapnia, and respiratory acidosis were worsened. Veno-venous extracorporeal membrane oxygenation (ECMO) was initiated after the operation. Status of the patient were improved after the application of ECMO. The patient was discharged without significant complication. Despite of several limitations in applying ECMO to patients with abdominal compartment syndrome (ACS) and multiple trauma, severe pulmonary dysfunction in ACS patients may be rescued without open abdomen treatment.
Keyword
MeSH Terms
Figure
Reference
-
1. Lam MC, Yang PT, Skippen PW, Kissoon N, Skarsgard ED. Abdominal compartment syndrome complicating paediatric extracorporeal life support: diagnostic and therapeutic challenges. Anaesth Intensive Care. 2008; 36:726–31. DOI: 10.1177/0310057X0803600517. PMID: 18853595.2. Augustin P, Lasocki S, Dufour G, Rode J, Karsenti A, Al-Attar N, et al. Abdominal compartment syndrome due to extracorporeal membrane oxygenation in adults. Ann Thorac Surg. 2010; 90:e40–1. DOI: 10.1016/j.athoracsur.2010.06.039. PMID: 20732475.3. Malbrain ML, De Laet IE, De Waele JJ, Kirkpatrick AW. Intra-abdominal hypertension: definitions, monitoring, interpretation and management. Best Pract Res Clin Anaesthesiol. 2013; 27:249–70. DOI: 10.1016/j.bpa.2013.06.009. PMID: 24012236.4. Strang SG, Van Lieshout EM, Verhoeven RA, Van Waes OJ, Verhofstad MH. Recognition and management of intra-abdominal hypertension and abdominal compartment syndrome;a survey among Dutch surgeons. Eur J Trauma Emerg Surg. 2017; 43:85–98. DOI: 10.1007/s00068-016-0637-x. PMID: 26902655. PMCID: PMC5306333.5. Hatch QM, Osterhout LM, Podbielski J, Kozar RA, Wade CE, Holcomb JB, et al. Impact of closure at the first take back: complication burden and potential overutilization of damage control laparotomy. J Trauma. 2011; 71:1503–11. DOI: 10.1097/TA.0b013e31823cd78d. PMID: 22182860.6. Popivanov G, Kjossev K, Mutafchiyski V. The open abdomen - still a challenge for the surgeons. Which is the best technique for temporary abdominal closure?. A focus on negative pressure wound therapy. G Chir. 2017; 38:267–72. DOI: 10.11138/gchir/2017.38.6.267. PMID: 29442056. PMCID: PMC5885786.7. Huang Y, Li Y. Open abdomen in trauma patients: a double-edged sword. Mil Med Res. 2016; 3:10. DOI: 10.1186/s40779-016-0079-0. PMID: 27042329. PMCID: PMC4818399.8. Delius R, Anderson H 3rd, Schumacher R, Shapiro M, Otsu T, Toft K, et al. Venovenous compares favorably with venoarterial access for extracorporeal membrane oxygenation in neonatal respiratory failure. J Thorac Cardiovasc Surg. 1993; 106:329–38. PMID: 8341073.9. Oshima K, Kunimoto F, Hinohara H, Ohkawa M, Mita N, Tajima Y, et al. Extracorporeal membrane oxygenation for respiratory failure: comparison of venovenous versus venoarterial bypass. Surg Today. 2010; 40:216–22. DOI: 10.1007/s00595-008-4040-z. PMID: 20180073.10. Papademetriou MD, Tachtsidis I, Banaji M, Elliott MJ, Hoskote A, Elwell CE. Optical topography to measure variations in regional cerebral oxygenation in an infant supported on veno-arterial extra-corporeal membrane oxygenation. Adv Exp Med Biol. 2012; 737:71–6. DOI: 10.1007/978-1-4614-1566-4_11. PMID: 22259084. PMCID: PMC4038014.11. Gutsche JT, Mikkelsen ME, McCarthy FH, Miano TA, Vernick WJ, Ramakrishna H, et al. Veno-venous extracorporeal life support in hemodynamically unstable patients with ARDS. Anesth Analg. 2017; 124:846–8. DOI: 10.1213/ANE.0000000000001646. PMID: 27749338. PMCID: PMC5313331.12. Kon ZN, Bittle GJ, Pasrija C, Pham SM, Mazzeffi MA, Herr DL, et al. Venovenous versus venoarterial extracorporeal membrane oxygenation for adult patients with acute respiratory distress syndrome requiring precannulation hemodynamic support: a review of the ELSO registry. Ann Thorac Surg. 2017; 104:645–9. DOI: 10.1016/j.athoracsur.2016.11.006. PMID: 28190548.13. Cordell-Smith JA, Roberts N, Peek GJ, Firmin RK. Traumatic lung injury treated by extracorporeal membrane oxygenation (ECMO). Injury. 2006; 37:29–32. DOI: 10.1016/j.injury.2005.03.027. PMID: 16243331.14. Lisagor P, Cohen D, McDonnell B, Lawlor D, Moore C. Irreversible shock revisited: mechanical support of the cardiovascular system: a case report and review. J Trauma. 1997; 42:1182–6. DOI: 10.1097/00005373-199706000-00037. PMID: 9210566.15. Larsson M, Forsman P, Hedenqvist P, Östlund A, Hultman J, Wikman A, et al. Extracorporeal membrane oxygenation improves coagulopathy in an experimental traumatic hemorrhagic model. Eur J Trauma Emerg Surg. 2017; 43:701–9. DOI: 10.1007/s00068-016-0730-1. PMID: 27815579. PMCID: PMC5629226.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Extracorporeal Membrane Oxygenation for Complicated Scrub Typhus
- Whole Lung Lavage in Pulmonary Alveolar Proteinosis associated with Lung Cancer Using Extracorporeal Membrane Oxygenation (ECMO)
- Venovenous and Venoarterial Extracorporeal Membrane Oxygenation for Repeated Life Threatening Hemoptysis: A case report
- Application of Veno-venoarterial Extracorporeal Membrane Oxygenation in Multitrauma Patient with ARDS: A case report
- Iatrogenic Iliac Vein Injury Following Extracorporeal Membrane Oxygenation Cannulation in a Patient with May-Thurner Syndrome: A Case Report and Literature Review