J Korean Soc Spine Surg.
2018 Dec;25(4):160-168. 10.4184/jkss.2018.25.4.160.
Factors Associated with Conversion from Conservative to Surgical Treatment in Single-Level Lumbar Spinal Stenosis Patients
- Affiliations
-
- 1Department of Orthopedic Surgery, National Police Hospital, Seoul, Korea. osahnyj@nate.com
- KMID: 2430141
- DOI: http://doi.org/10.4184/jkss.2018.25.4.160
Abstract
- STUDY DESIGN: Retrospective study of prospectively-collected data.
OBJECTIVES
To determine the factors associated with conversion from conservative to surgical treatment in single-level lumbar spinal stenosis patients. SUMMARY OF LITERATURE REVIEW: Various reports have presented clinical outcomes after the surgical and nonsurgical treatment of spinal stenosis. However, few reports have investigated factors predicting conversion to surgery during the course of conservative treatment.
MATERIALS AND METHODS
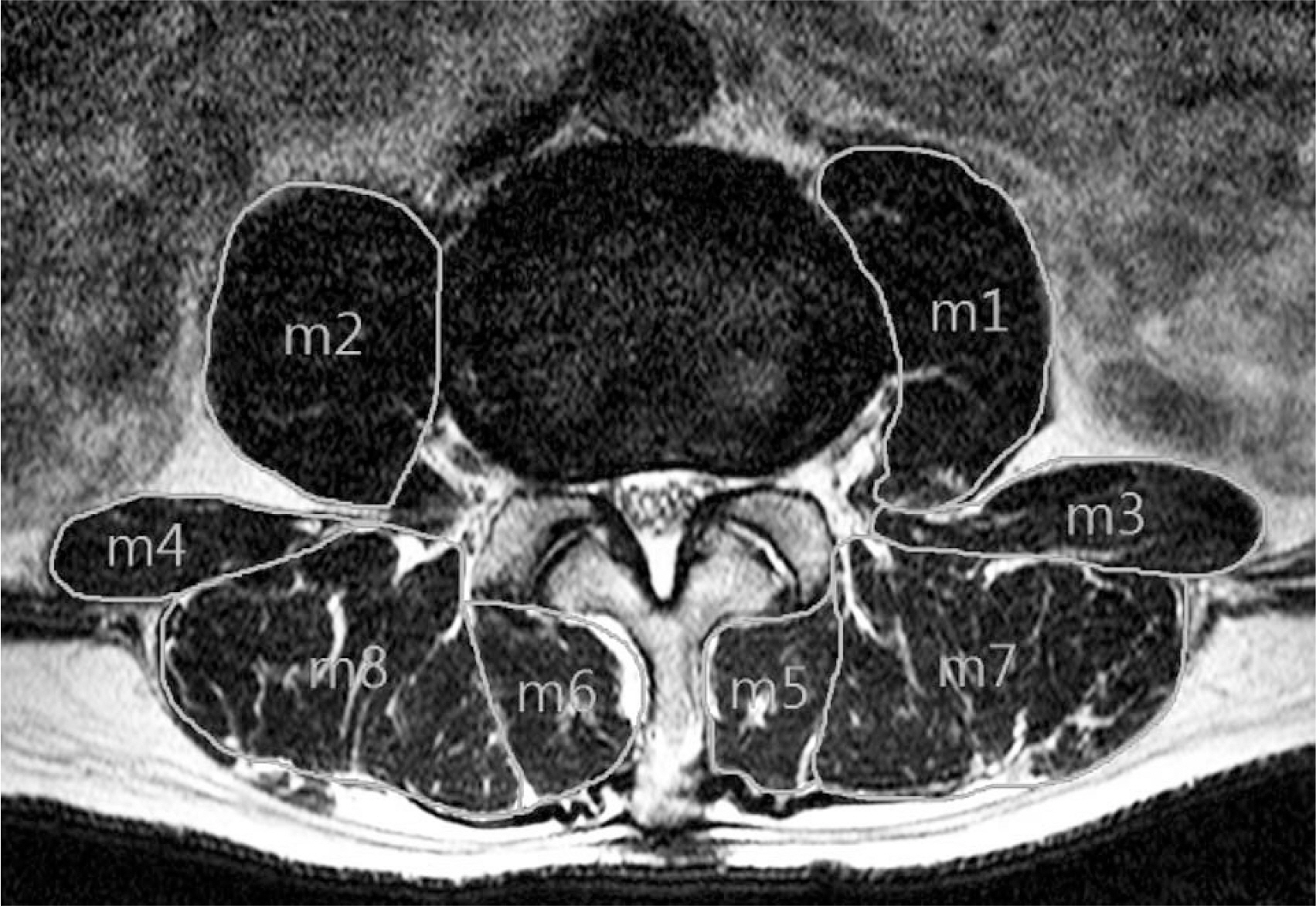
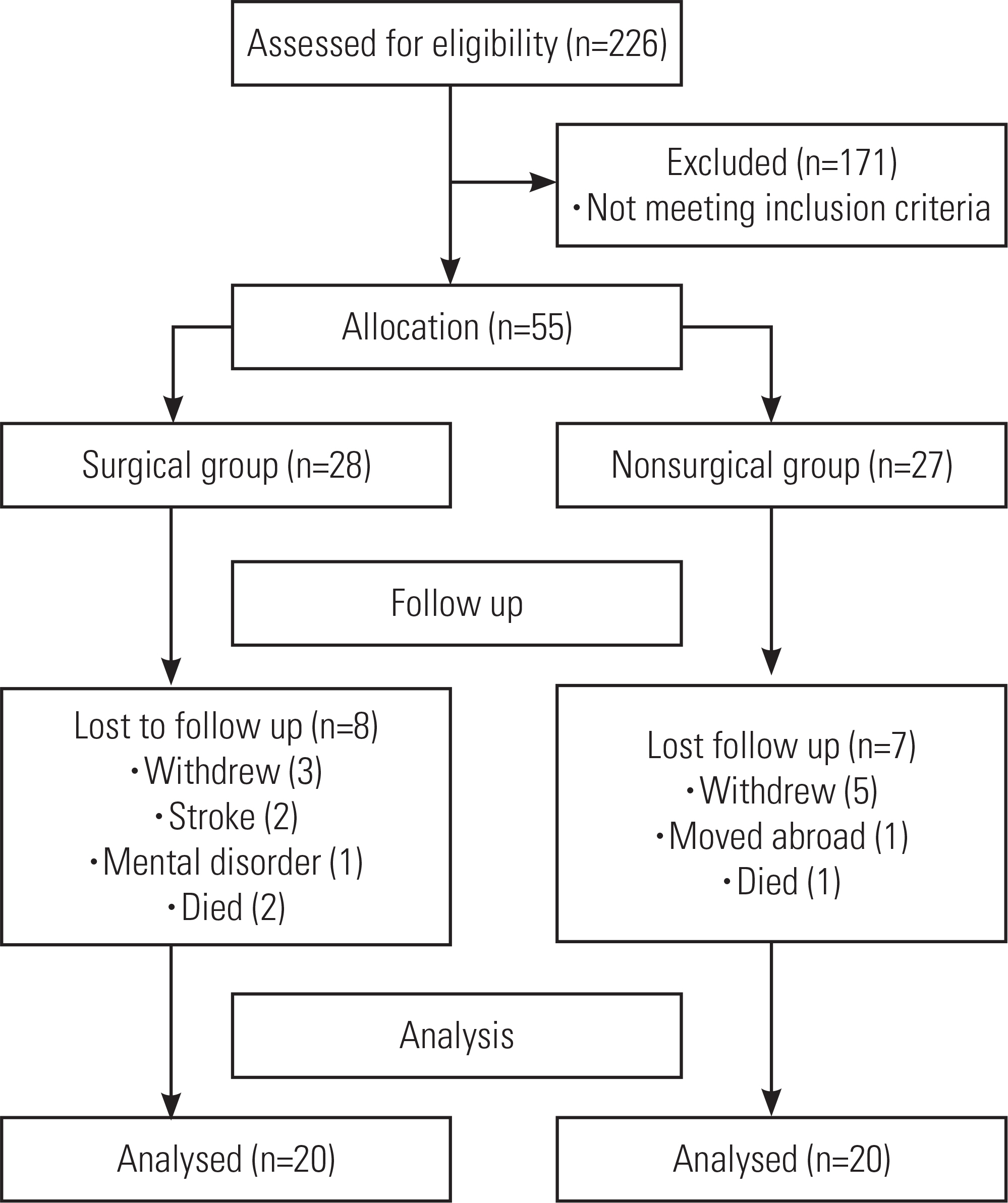
We analyzed 40 patients who visited our hospital from May 2010 to May 2015 and were traceable for at least 3 years after being advised to undergo surgery following 3 months of conservative treatment. Of these patients, 20 underwent surgery and 20 did not. We then investigated the factors associated with conversion to surgical treatment. Clinical assessments were conducted using a questionnaire, and the overall area of the spinal canal and the muscle area within the spinal canal were measured using magnetic resonance imaging.
RESULTS
The average area of the spinal canal was 81.40±53.61 mm2 in the surgical group, compared to 127.75±82.55 mm2 in the nonsurgical group (p=0.042). The muscle area in the spinal canal was 5.17±1.30 cm2 in the surgical group, whereas it was 6.40±1.56 cm2 in the nonsurgical group (p=0.010). The patients in the surgical group were more likely to have experienced repetitive strain and to have frequently visited health clubs (p=0.047, p=0.037, respectively). However, regular stretching was more common in the nonsurgical group (p=0.028).
CONCLUSIONS
The factors associated with conversion to surgical treatment were a narrow spinal canal, a small muscle area within the spinal canal, visiting health clubs, repetitive sprain, and not stretching. A small muscle area within the spinal canal can be considered as a key factor related to surgical conversion.
MeSH Terms
Figure
Reference
-
1. Katz JN, Harris MB. Clinical practice. Lumbar spinal stenosis. N Engl J Med. 2008 Feb; 358(8):818–25. DOI: 10.1056/NEJMcp0708097.2. Atlas SJ, Keller RB, Wu YA, et al. Long-term Outcomes of Surgical and Nonsurgical Management of Lumbar Spinal stenosis: 8 to 10 Year Results from the Maine Lumbar Spine Study. Spine. 2005 Apr; 30(8):936–43. DOI: 10.1097/01. brs.0000158953.57966.c0.
Article3. Malmivaara A, Slä tis P, Heliö vaara M, et al. Surgical or Nonoperative Treatment for Lumbar Spinal stenosis? A Randomized Controlled Trial. Spine (Phila Pa 1976). 2007 Jan 1; 32(1):1–8. DOI: 10.1097/01.brs.0000251014.81875.6d.4. Matsudaira K, Hara N, Oka H, et al. Predictive Factors for Subjective Improvement in Lumbar Spinal Stenosis Patients with Nonsurgical Treatment: A 3-Year Prospective Cohort Study. PLoS ONE. 2016 Feb; 11(2):e0148584. DOI: 10.1371/journal.pone.0148584.
Article5. Jeon CH, Kim DJ, Kim SK, et al. Validation in the Cross-cultural Adaptation of the Korean Version Of the Oswestry Disability Index. J Korean Med Sci. 2006 Dec; 21(6):1092–7. DOI: 10.3346/jkms.2006.21.6.1092.
Article6. Bolender NF, Schonstrom N, Sepengler D. Role of computed tomography and Myelography in the diagnosis of central spinal stenosis. J Bone Joint Surg Am. 1985 Feb; 67(2):240–6. DOI: 10.2106/00004623-198567020-00009.
Article7. Shim DM, Choi YH, Yang JH, et al. Analysis and measurement of the lumbar spinal canal dimension using magnetic resonance imaging. J Korean Orthop Assoc. 2008; 43(5):588–94. DOI: 10.4055/jkoa.2008.43.5.588.
Article8. WAN Q, LIN C, LI X, et al. MRI assessment of paraspinal muscles in patients with acute and chronic unilateral low back pain. Br J Radiol. 2015 Sep; 88(1053):20140546. DOI: 10.1259/bjr.20140546.
Article9. Porter RW, Wicks M, Ottewell D. Measurement of the spinal canal by diagnostic ultrasound. J Bone Joint Surg Br. 1978 Nov; 60-B(4):481–4. DOI: 10.1302/0301-620x.60b4.711793.
Article10. Ahn YJ, Im SH, Park SH. Short-Term Effects of Selective Nerve Root Block in Spinal Stenosis Patients According to Spinal Canal Dimensions. J Korean Orthop Assoc. 2017 Jun; 24(2):72–9. DOI: 10.4184/jkss.2017.24.2.72.
Article11. Shen W, Punyanitya M, Wang Z, et al. Total body skeletal muscle and adipose tissue volumes: estimation from a single abdominal cross-sectional image. J Appl Physiol (1985). 2004 Dec; 97(6):2333–8. DOI: 10.1152/japplphysi-ol.00744.2004.
Article12. Baumgartner RN, Koehler KM, Gallagher D, et al. Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol. 1998 Apr; 147(8):755–63. DOI: 10.1093/oxfordjournals.aje.a009520.
Article13. D'hooge R, Cagnie B, Crombez G, et al. Increased intra-muscular fatty infiltration without differences in lumbar muscle cross-sectional area during remission of unilateral recurrent low back pain. Man Ther. 2012 Dec; 17(6):584–8. DOI: 10.1016/j.math.2012.06.007.14. Lee JC, Cha JG, Kim Y, et al. Quantitative analysis of back muscle degeneration in the patients with the degenerative lumbar flat back using a digital image analysis. Comparison with the normal controls. Spine. 2008 Feb; 33(3):318–25. DOI: 10.1097/BRS.0b013e318162458f.15. Knutsson B. Comparative value of electromyographic, myelography, and clinical neurological examination in the diagnosis of lumbar root compression syndrome. Arch Orthop Scand Suppl. 1961; 49:1–135. DOI: 10.3109/ort.1961.32.suppl-49.01.16. Johnson EW, Melvin J. Value of electromyography in lumbar radiculopathy. Arch Phys Med Rehabil. 1971 Jun; 52(6):239–43. DOI: 10.3109/ort.1961.32.suppl-49.01.17. Hides JA, Stokes MJ, Saide M, et al. Evidence of lumbar multifidus muscle wasting ipsilateral to symptoms in patients with acute/subacute low back pain. Spine (Phila Pa 1976). 1994 Jan; 19(2):165–72. DOI: 10.1097/00007632-199401001-00009.
Article18. Hodges PW, Holm AK, Hansson T, et al. Rapid atrophy of the lumbar multifidus follows experimental disc or nerve root injury. Spine (Phila Pa 1976). 2006 Dec; 31(25):2926–33. DOI: 10.1097/01.brs.0000248453.51165.0b.
Article19. MacDonald DA, Lorimer Moseley G, Hodges PW. The lumbar multifidus. Dose the evidence support clinical be-liefs? Man Ther. 2006 Nov; 11(4):254–63. DOI: 10.1016/j.math.2006.02.004.20. Roy SH, De Luca CJ, Casavant DA. Lumbar muscle fa-tigue and chronic lower back pain. Spine (Phila Pa 1976). 1989 Sep; 14(9):992–1001. DOI: 10.1097/00007632-198909000-00014.
Article21. Twomey L, Taylor J. Exercise and spinal manipulation in the treatment of low back pain. Spine. Spine (Phila Pa 1976). 1995 Mar; 20(5):615–9. DOI: 10.1097/00007632-199503010-00021.22. Hides JA, Stanton WR, McMahon S, et al. Effect of stabi-lization training on multifidus muscle cross-sectional area among young elite cricketers with low back pain. J Orthop Phys Ther. 2008 Mar; 38(3):101–8. DOI: 10.2519/jospt.2008.2658.
Article23. Mannion AF, Taimela S, Muntener M, et al. Active therapy for chronic low back pain. part 1. Effects on back muscle activation, fatigability, and strength. Spine (Phila Pa 1976). 2001 Apr; 26(8):897–908. DOI: 10.1097/00007632-200104150-00013.24. Callaghan JP, Gunning JL, McGill SM. The relationship between lumbar spine load and muscle activity during extensor exercises. Phys Ther. 1998 Jan; 78(1):8–18. DOI: 10.1093/ptj/78.1.8.
Article25. Elliott JM, Jull G, Noteboom JT, et al. Fatty infiltration in the cervical extensor muscles in persistent whiplash-associated disorders. a magnetic resonance imaging analysis. Spine (Phila Pa 1976). 2006 Oct; 31(22):E847–55. DOI: 10.1097/01.brs.0000240841.07050.34.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors Associated with the Effect of Conservative Treatment in Surgically Indicated Single-Level Lumbar Spinal Stenosis Patient
- Current Status of Biportal Endoscopic Decompression for Lumbar Central Stenosis
- Diagnostic Significance of Myelo-Enhanced Computerized Tomography(MECT) in Spinal Stenosis
- A Case of Coexisting Cervical and Lumbar Spinal Stenosis
- Single Incision Tubular Decompression to Treat Multi-level Lumbar Spinal Stenosis: A Retrospective Review