Blood Res.
2018 Dec;53(4):314-319. 10.5045/br.2018.53.4.314.
Relationship between liver iron concentration determined by R2-MRI, serum ferritin, and liver enzymes in patients with thalassemia intermedia
- Affiliations
-
- 1Department of Pediatrics, Al-Kindy College of Medicine, University of Baghdad, Baghdad, Iraq.
- 2Department of Obstetrics & Gynecology, College of Medicine, University of Baghdad, Baghdad, Iraq.
- 3Division of Radiology, Department of Surgery, Al-Kindy College of Medicine, University of Baghdad, Baghdad, Iraq.
- 4Department of Endocrinology, Al-Elwiya Pediatric Teaching Hospital, Al-Rusafa Health Directorate, Baghdad, Iraq.
- KMID: 2429306
- DOI: http://doi.org/10.5045/br.2018.53.4.314
Abstract
- BACKGROUND
Iron overload is a risk factor affecting all patients with thalassemia intermedia (TI). We aimed to determine whether there is a relationship of serum ferritin (SF) and alanine aminotransferase (ALT) with liver iron concentration (LIC) determined by R2 magnetic resonance imaging (R2-MRI), to estimate the most relevant degree of iron overload and best time to chelate in patients with TI.
METHODS
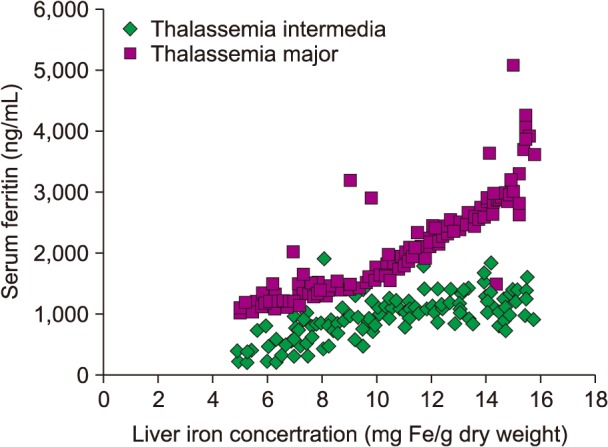
In this cross-sectional study, 119 patients with TI (mean age years) were randomly selected and compared with 120 patients who had a diagnosis of thalassemia major (TM). Correlations of LIC, as determined by R2-MRI, with SF and ALT levels, were assessed in all participants. A P-value < 0.05 was considered statistically significant.
RESULTS
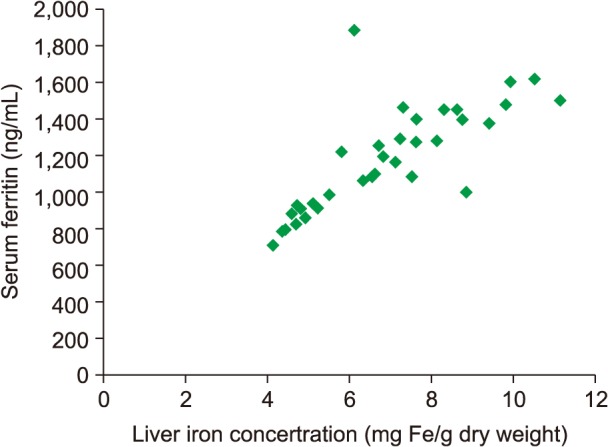
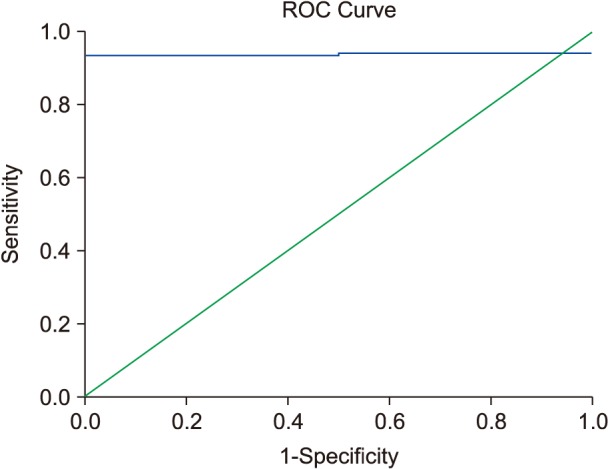
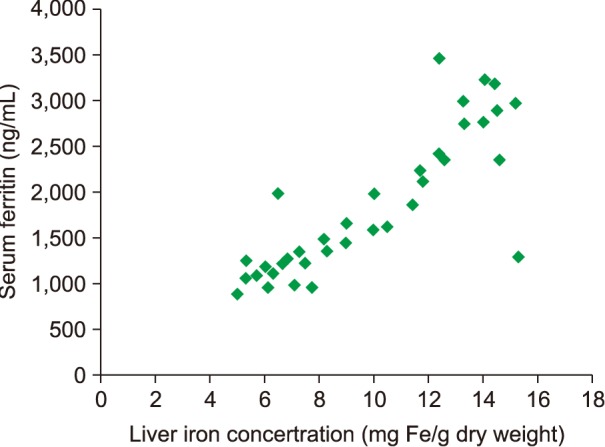
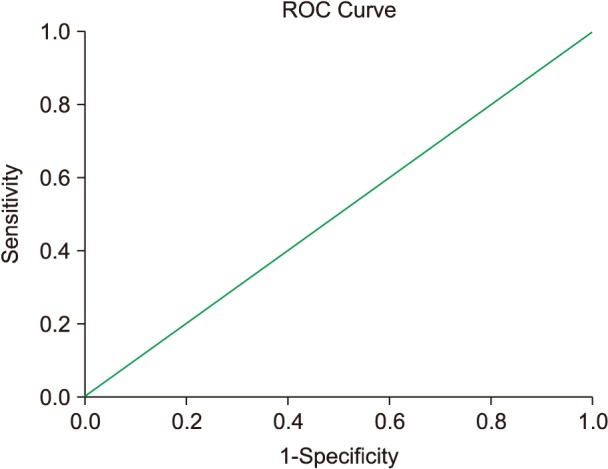
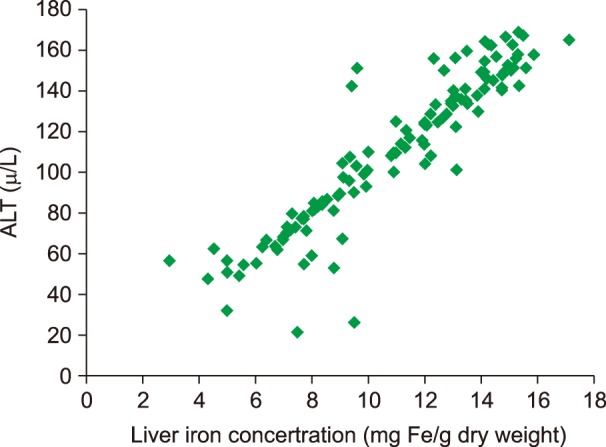
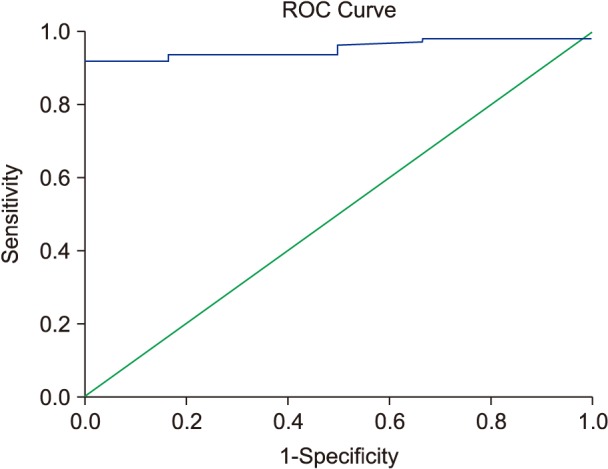
SF and LIC levels were lower in patients with TI than in those with TM; only ferritin values were significant. We found a statistically significant relationship between SF and LIC, with cut-off estimates of SF in patients with TI who had splenectomy and those who entered puberty spontaneously (916 and 940 ng/mL, respectively) with LIC >5 mg Fe/g dry weight (P < 0.0001). A significant relationship was also found for patients with TI who had elevated ALT level (63.5 U/L), of 3.15 times the upper normal laboratory limit, using a cut-off for LIC ≥5 mg Fe/g dry weight.
CONCLUSION
We determined the cut-off values for ALT and SF indicating the best time to start iron chelation therapy in patients with TI, and found significant correlations among iron overload, SF, and ALT.
Keyword
MeSH Terms
Figure
Reference
-
1. Ben Salah N, Bou-Fakhredin R, Mellouli F, Taher AT. Revisiting beta thalassemia intermedia: past, present, and future prospects. Hematology. 2017; 22:607–616. PMID: 28589785.
Article2. Rivella S. β-thalassemias: paradigmatic diseases for scientific discoveries and development of innovative therapies. Haematologica. 2015; 100:418–430. PMID: 25828088.
Article3. Parrow NL, Gardenghi S, Ramos P, et al. Decreased hepcidin expression in murine β-thalassemia is associated with suppression of Bmp/Smad signaling. Blood. 2012; 119:3187–3189. PMID: 22461476.
Article4. Rivella S. The role of ineffective erythropoiesis in non- transfusion-dependent thalassemia. Blood Rev. 2012; 26(Suppl 1):S12–S15. PMID: 22631035.5. Marsella M, Ammirabile M, Di Matola T, et al. Is there a difference in phenotype between males and females with nontransfusion-dependent thalassemia? A cross-sectional evaluation. Hematology. 2018; 23:522–525. PMID: 29303050.
Article6. Casu C, Aghajan M, Oikonomidou PR, Guo S, Monia BP, Rivella S. Combination of Tmprss6- ASO and the iron chelator deferiprone improves erythropoiesis and reduces iron overload in a mouse model of beta-thalassemia intermedia. Haematologica. 2016; 101:e8–e11. PMID: 26405152.
Article7. Fischer R, Harmatz PR. Non-invasive assessment of tissue iron overload. Hematology Am Soc Hematol Educ Program. 2009; 1:215–221.
Article8. Olivieri NF, Brittenham GM. Iron-chelating therapy and the treatment of thalassemia. Blood. 1997; 89:739–761. PMID: 9028304.
Article9. Porter JB, Elalfy M, Taher A, et al. Limitations of serum ferritin to predict liver iron concentration responses to deferasirox therapy in patients with transfusion-dependent thalassaemia. Eur J Haematol. 2017; 98:280–288. PMID: 27859648.
Article10. Olivieri NF, Brittenham GM, Matsui D, et al. Iron-chelation therapy with oral deferiprone in patients with thalassemia major. N Engl J Med. 1995; 332:918–922. PMID: 7877649.
Article11. Wood JC. Magnetic resonance imaging measurement of iron overload. Curr Opin Hematol. 2007; 14:183–190. PMID: 17414205.
Article12. Tanner JM. Growth at adolescence: with a general consideration of the effects of hereditary and environmental factors upon growth and maturation from birth to maturity. 2nd ed. Oxford, UK: Blackwell;1962.13. Zachmann M, Prader A, Kind HP, Häfliger H, Budliger H. Testicular volume during adolescence. Cross-sectional and longitudinal studies. Helv Paediatr Acta. 1974; 29:61–72. PMID: 4838166.14. Shalitin S, Carmi D, Weintrob N, et al. Serum ferritin level as a predictor of impaired growth and puberty in thalassemia major patients. Eur J Haematol. 2005; 74:93–100. PMID: 15654898.
Article15. Fung EB, Harmatz PR, Lee PD, et al. Increased prevalence of iron-overload associated endocrinopathy in thalassaemia versus sickle-cell disease. Br J Haematol. 2006; 135:574–582. PMID: 17054676.
Article16. Al-Momen H. Iron chelation therapy in sickle cell/beta thalassemia syndrome, a 2 years' extension study. KCMJ. 2017; 13:76–81.
Article17. Fung EB, Harmatz P, Milet M, et al. Morbidity and mortality in chronically transfused subjects with thalassemia and sickle cell disease: a report from the multi-center study of iron overload. Am J Hematol. 2007; 82:255–265. PMID: 17094096.
Article18. Taher A, El Rassi F, Isma'eel H, Koussa S, Inati A, Cappellini MD. Correlation of liver iron concentration determined by R2 magnetic resonance imaging with serum ferritin in patients with thalassemia intermedia. Haematologica. 2008; 93:1584–1586. PMID: 18728025.
Article19. Pakbaz Z, Fischer R, Fung E, Nielsen P, Harmatz P, Vichinsky E. Serum ferritin underestimates liver iron concentration in transfusion independent thalassemia patients as compared to regularly transfused thalassemia and sickle cell patients. Pediatr Blood Cancer. 2007; 49:329–332. PMID: 17554789.
Article20. Fiorelli G, Fargion S, Piperno A, Battafarano N, Cappellini MD. Iron metabolism in thalassemia intermedia. Haematologica. 1990; 75:89–95. PMID: 2086386.21. Origa R, Galanello R, Ganz T, et al. Liver iron concentrations and urinary hepcidin in beta-thalassemia. Haematologica. 2007; 92:583–588. PMID: 17488680.22. Asadov C, Alimirzoeva Z, Mammadova T, Aliyeva G, Gafarova S, Mammadov J. β-thalassemia intermedia: a comprehensive overview and novel approaches. Int J Hematol. 2018; 108:5–21. PMID: 29380178.
Article23. El Rassi F, Cappellini MD, Inati A, Taher A. Beta-thalassemia intermedia: an overview. Pediatr Ann. 2008; 37:322–328. PMID: 18543543.
Article24. De Sanctis V. Growth and puberty and its management in thalassaemia. Horm Res. 2002; 58:72–79. PMID: 12373018.
Article25. Taher A, Isma'eel H, Cappellini MD. Thalassemia intermedia: revisited. Blood Cells Mol Dis. 2006; 37:12–20. PMID: 16737833.
Article26. Ameli M, Besharati S, Nemati K, Zamani F. Relationship between elevated liver enzyme with iron overload and viral hepatitis in thalassemia major patients in Northern Iran. Saudi Med J. 2008; 29:1611–1615. PMID: 18998011.27. Majd Z, Haghpanah S, Ajami GH, et al. Serum ferritin levels correlation with heart and liver MRI and LIC in patients with transfusion-dependent thalassemia. Iran Red Crescent Med J. 2015; 17:e24959. PMID: 26023341.
Article28. Musallam KM, Cappellini MD, Taher AT. Evaluation of the 5mg/g liver iron concentration threshold and its association with morbidity in patients with β-thalassemia intermedia. Blood Cells Mol Dis. 2013; 51:35–38. PMID: 23425967.
Article29. Taher AT, Porter JB, Viprakasit V, et al. Defining serum ferritin thresholds to predict clinically relevant liver iron concentrations for guiding deferasirox therapy when MRI is unavailable in patients with non-transfusion-dependent thalassaemia. Br J Haematol. 2015; 168:284–290. PMID: 25212456.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Incidenc of Iron Deficiency Anemia and Changes in Serum Feffitin Level in Various Childhood Diseases
- Body iron, serum ferritin, and nonalcoholic fatty liver disease
- A Study of Serum Ferritin Levels in Patients with Acute Infectious Hepatitis
- Optimal method for early detection of cardiac disorders in thalassemia major patients: magnetic resonance imaging or echocardiography?
- Effects of Chronic Aluminum Administration on Blood and Liver Iron-Related Parameters in Mice