Korean J Ophthalmol.
2018 Dec;32(6):438-444. 10.3341/kjo.2018.0044.
Combination Surgery of Silicone Tube Intubation and Conjunctival Resection in Patients with Epiphora
- Affiliations
-
- 1Department of Ophthalmology, Dong-A University College of Medicine, Busan, Korea. hbahn@dau.ac.kr
- KMID: 2427957
- DOI: http://doi.org/10.3341/kjo.2018.0044
Abstract
- PURPOSE
To compare the success rates of performing only silicone tube intubation versus carrying out both conjunctival resection and silicone tube intubation.
METHODS
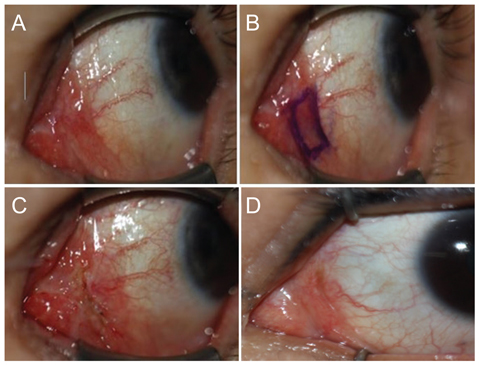
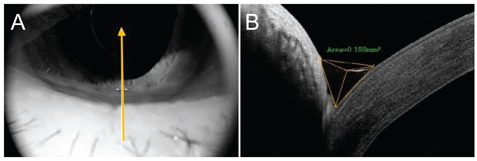
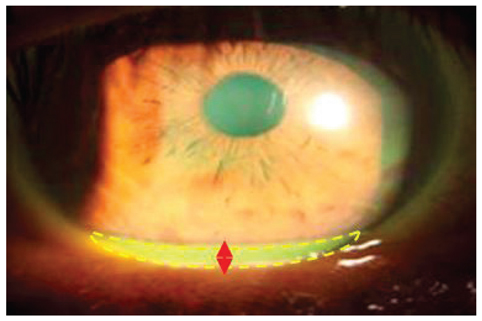
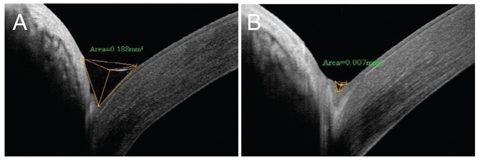
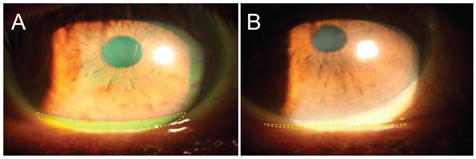
The subjects of this study involved 62 patients (96 eyes) between October 2015 and May 2017 who were diagnosed as having punctal stricture or nasolacrimal duct stenosis. Out of 96 eyes, 47 underwent only silicone tube intubation, and 49 underwent both silicone tube intubation and conjunctival resection. Three parameters were measured at 1, 3, and 6 months after the surgery: the area of the tear meniscus using RTVue-100 anterior segment optical coherence tomography, the height of the tear meniscus using a slit lamp microscope, and the subjective satisfaction of patients as a result of improved sympotms like epiphora. The surgery was considered successful when the patients' experienced the resolution of symptoms and reduction of the area and height of the tear meniscus.
RESULTS
The area of the tear meniscus, height of the tear meniscus, and subjective satisfaction of patients was superior in the group that underwent both silicone tube intubation and conjunctival resection compared silicone tube intubation only. Based on these results, the success rate of the surgery was 68.9% in the group that underwent only silicone tube intubation and 78.7% in the group that underwent both silicone tube intubation and conjunctival resection.
CONCLUSIONS
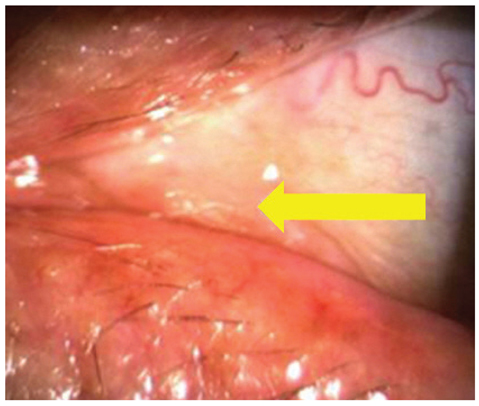
The resection of relaxed plica semilunares seems to increase the success rate of silicone tube intubation through the reduction of the area and height of the tear meniscus. Therefore, after determining the degree of conjunctivochalasis, if it was found to be severe, a combination with conjunctival resection was expected to increase the success rate of the surgery.
Keyword
MeSH Terms
Figure
Reference
-
1. Oum JS, Park JW, Choi YK, et al. Result of partial nasolacrimal duct obstruction after silicone tube intubation. J Korean Ophthalmol Soc. 2004; 45:1777–1782.2. Keith CG. Intubation of the lacrimal passages. Am J Ophthalmol. 1968; 65:70–74.
Article3. Beigi B, O'Keefe M. Results of Crawford tube intubation in children. Acta Ophthalmol (Copenh). 1993; 71:405–407.
Article4. Jung JJ, Jang SY, Jang JW, In JH. Comparison results of silicone tube intubation according to syringing and dacryocystography. J Korean Ophthalmol Soc. 2014; 55:1584–1588.
Article5. Park JJ, Shin DS, Hong SP, Lee KW. Effects of double silicone tube intubation for nasolacrimal duct obstruction in adults. J Korean Ophthalmol Soc. 2005; 46:1951–1956.6. Lee DH, Choi HY, Ahn JH. Comparison of results and complications between 0.64 mm and 0.94 mm silicone tube intubation in adults. J Korean Ophthalmol Soc. 2016; 57:1193–1198.
Article7. Lee KS, Byun YJ. Dacryocystorhinostomy with intraoperative mitomycin C. J Korean Ophthalmol Soc. 1998; 39:1909–1914.8. Kim YT, Chung WS. The effect of mitomycin C in endonasal dacryocystorhinostomy. J Korean Ophthalmol Soc. 2002; 43:728–732.9. Lee JM, Lee YJ, Kim JH. The effect of mitomycin C concentration in endonasal dacryocystorhinostomy. J Korean Ophthalmol Soc. 2004; 45:1609–1614.10. Song BY, Kim JD, Kim S. Silicone intubation and postoperative mitomycin application for partial nasolacrimal duct obstruction in adults. J Korean Ophthalmol Soc. 2005; 46:16–21.11. Kim DS, Lee YJ. Efficacy of silicone nasolacrimal intubation with mitomycin C treatmentfor treatment of incomplete nasolacrimal duct obstruction. J Korean Ophthalmol Soc. 2006; 47:181–185.12. Lim CS, Martin F, Beckenham T, Cumming RG. Nasolacrimal duct obstruction in children: outcome of intubation. J AAPOS. 2004; 8:466–472.
Article13. Kaufman LM, Guay-Bhatia LA. Monocanalicular intubation with Monoka tubes for the treatment of congenital nasolacrimal duct obstruction. Ophthalmology. 1998; 105:336–341.
Article14. Engel JM, Hichie-Schmidt C, Khammar A, et al. Monocanalicular silastic intubation for the initial correction of congenital nasolacrimal duct obstruction. J AAPOS. 2007; 11:183–186.
Article15. Oh SH, Park JY, Yim HB, Lee NY. Treatment of epiphora in patients with conjunctivochalasis using conjunctival fixation to the sclera. J Korean Ophthalmol Soc. 2012; 53:1063–1067.
Article16. Dartt DA. The conjunctiva: structure and function. In : Duane TD, Tasman W, Jaeger EA, editors. Duane's foundations of clinical ophthalmology. Philadelphia: Lippincott, Williams & Wilkins;2012. p. 11.17. Watanabe A, Yokoi N, Kinoshita S, et al. Clinicopathologic study of conjunctivochalasis. Cornea. 2004; 23:294–298.
Article18. Francis IC, Chan DG, Kim P, et al. Case-controlled clinical and histopathological study of conjunctivochalasis. Br J Ophthalmol. 2005; 89:302–305.
Article19. Meller D, Li DQ, Tseng SC. Regulation of collagenase, stromelysin, and gelatinase B in human conjunctival and conjunctivochalasis fibroblasts by interleukin-1beta and tumor necrosis factor-alpha. Invest Ophthalmol Vis Sci. 2000; 41:2922–2929.20. Erdogan-Poyraz C, Mocan MC, Bozkurt B, et al. Elevated tear interleukin-6 and interleukin-8 levels in patients with conjunctivochalasis. Cornea. 2009; 28:189–193.
Article21. Ellis S. Structure and function of the lymphatic system: an overview. Br J Community Nurs. 2006; 11:S4–S6.
Article22. Skandalakis JE, Skandalakis LJ, Skandalakis PN. Anatomy of the lymphatics. Surg Oncol Clin N Am. 2007; 16:1–16.
Article23. Kim JT, Kim JH, Kim JC. Visualization of subconjunctival lymphatics and its significance. J Korean Ophthalmol Soc. 2008; 49:1215–1219.
Article24. Bae JB, Park WC. Histopathologic characteristics of conjunctivochalasis. J Korean Ophthalmol Soc. 2013; 54:1165–1174.
Article25. Wang J, Aquavella J, Palakuru J, Chung S. Repeated measurements of dynamic tear distribution on the ocular surface after instillation of artificial tears. Invest Ophthalmol Vis Sci. 2006; 47:3325–3329.
Article26. Zhou S, Li Y, Lu AT, et al. Reproducibility of tear meniscus measurement by Fourier-domain optical coherence tomography: a pilot study. Ophthalmic Surg Lasers Imaging. 2009; 40:442–447.
Article27. Kim JS, Bae JB, Seo JW, Park WC. Changes in area of conjunctiva and tear meniscus measured using anterior segment optical coherence tomography after conjunctivochalasis surgery. J Korean Ophthalmol Soc. 2015; 56:509–514.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Comparison of Punctoplasty and Silicone Tube Intubation in Patients with Punctal Obstruction
- Silicone Tube Intubation in Acquired Nasolacrimal Duct Obstruction
- Silicone Intubation for Treatment of Punctal Stenosis
- Factors Affecting the Long-term Outcome of Silicone Tube Intubation in Patients With Nasolacrimal Duct Obstruction
- Treatment of Congenital Nasolacrimal Duct Obstruction Using Silicone Intubation Set