Korean J Radiol.
2017 Apr;18(2):361-369. 10.3348/kjr.2017.18.2.361.
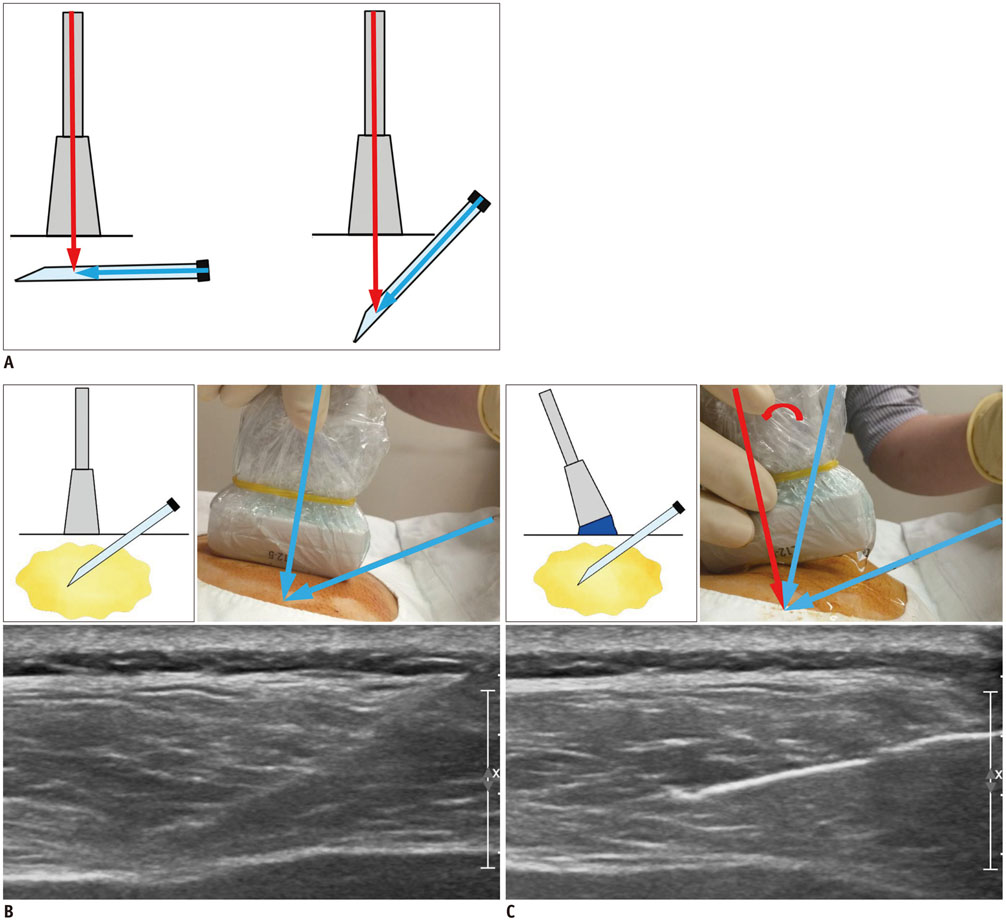
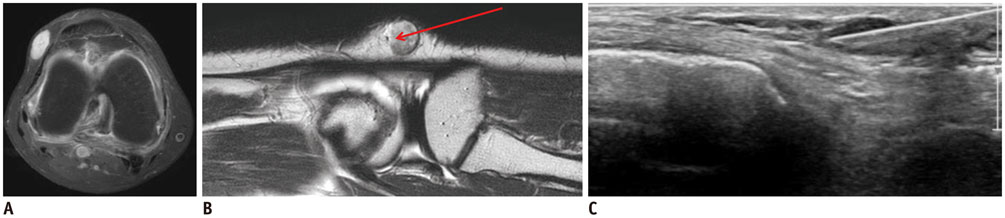
Practical Guidelines for Ultrasound-Guided Core Needle Biopsy of Soft-Tissue Lesions: Transformation from Beginner to Specialist
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul 05505, Korea. chung@amc.seoul.kr
- 2Department of Radiology, Dankook University Hospital, Cheonan 31116, Korea.
- 3Department of Orthopedic Surgery, University of Ulsan College of Medicine, Asan Medical Center, Seoul 05505, Korea.
- KMID: 2427948
- DOI: http://doi.org/10.3348/kjr.2017.18.2.361
Abstract
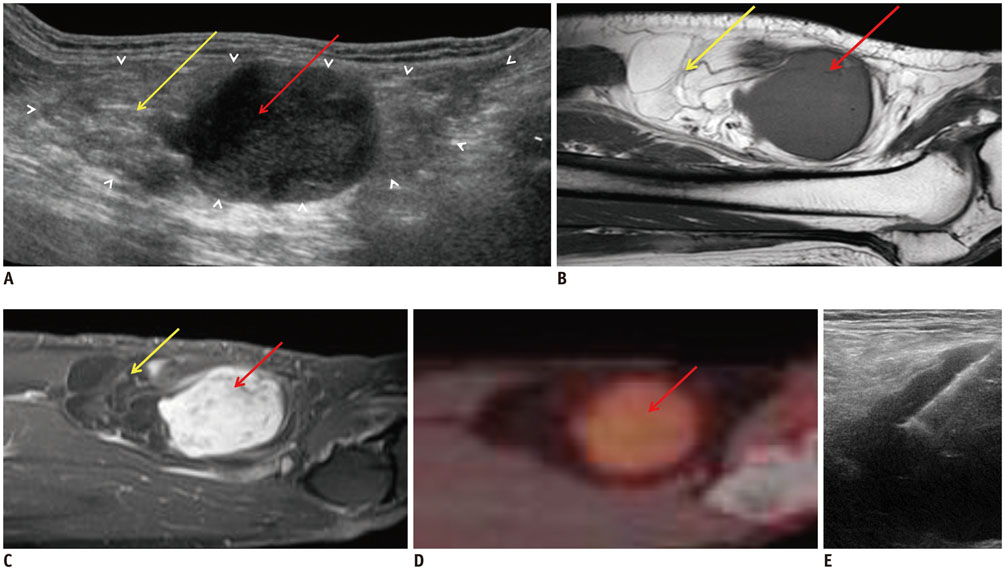
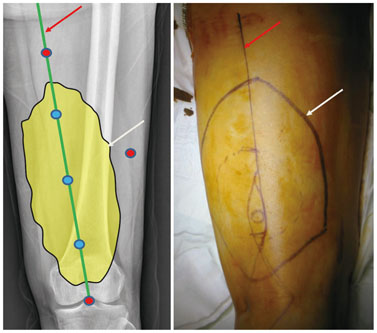
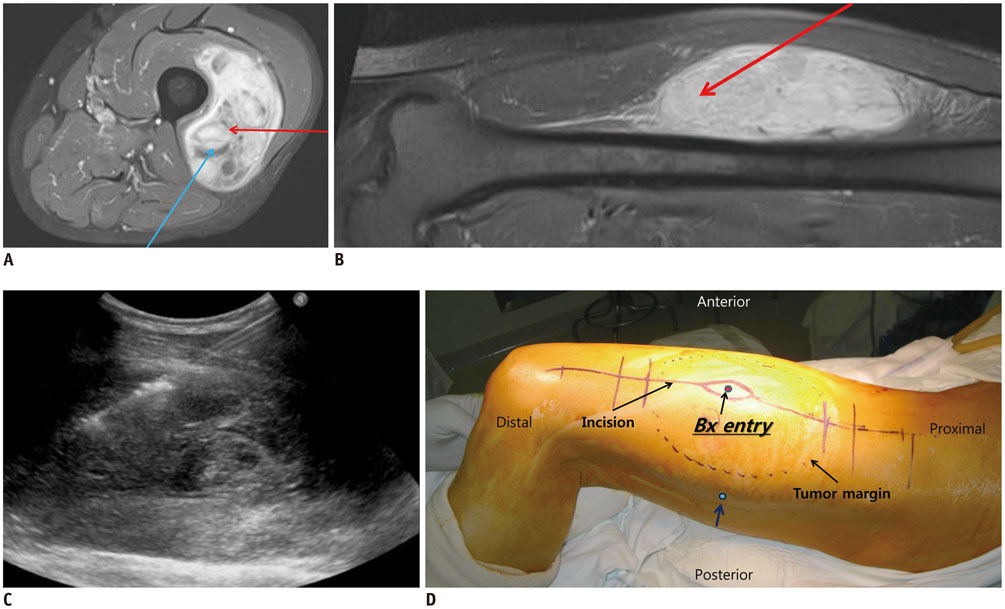
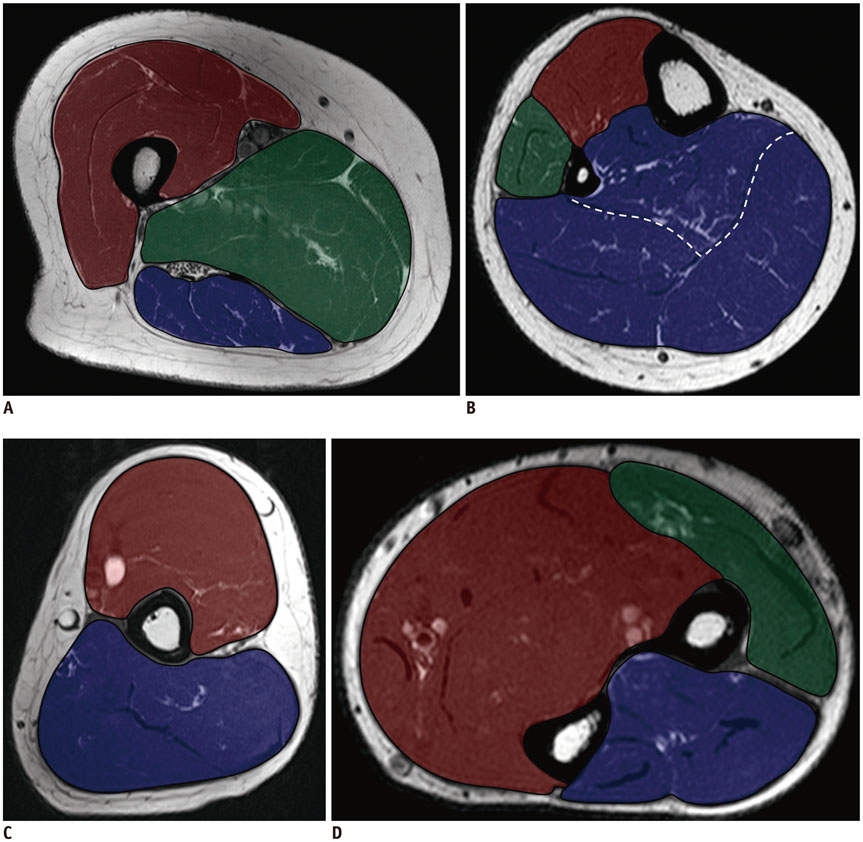
- Ultrasound-guided core needle biopsy (US-CNB) is an important step in the diagnosis of musculoskeletal soft-tissue lesions. To maximize efficacy and minimize the complications of US-CNB, it is critical to collaborate with a multidisciplinary team and to understand the particular considerations of US-CNB for these lesions. The purpose of this article is to provide a systematic review and step-by-step tips for using US-CNB to diagnose musculoskeletal soft-tissue lesions.
MeSH Terms
Figure
Cited by 1 articles
-
Core-Needle Biopsy Does Not Show Superior Diagnostic Performance to Fine-Needle Aspiration for Diagnosing Thyroid Nodules
Ilah Shin, Eun-Kyung Kim, Hee Jung Moon, Jung Hyun Yoon, Vivian Youngjean Park, Si Eun Lee, Hye Sun Lee, Jin Young Kwak
Yonsei Med J. 2020;61(2):161-168. doi: 10.3349/ymj.2020.61.2.161.
Reference
-
1. Kim SY, Chung HW. Small musculoskeletal soft-tissue lesions: US-guided core needle biopsy--comparative study of diagnostic yields according to lesion size. Radiology. 2016; 278:156–163.2. Huang AJ, Kattapuram SV. Musculoskeletal neoplasms: biopsy and intervention. Radiol Clin North Am. 2011; 49:1287–1305. vii3. Balach T, Stacy GS, Haydon RC. The clinical evaluation of soft tissue tumors. Radiol Clin North Am. 2011; 49:1185–1196. vi4. Mavrogenis AF, Angelini A, Errani C, Rimondi E. How should musculoskeletal biopsies be performed? Orthopedics. 2014; 37:585–588.5. Toomayan GA, Robertson F, Major NM. Lower extremity compartmental anatomy: clinical relevance to radiologists. Skeletal Radiol. 2005; 34:307–313.6. Toomayan GA, Robertson F, Major NM, Brigman BE. Upper extremity compartmental anatomy: clinical relevance to radiologists. Skeletal Radiol. 2006; 35:195–201.7. Sridharan R, Yunos SM, Aziz S, Hussain RI, Alhabshi SM, Suria Hayati MP, et al. Comparison on the use of semi-automated and automated core biopsy needle in ultrasound guided breast biopsy. Med J Malaysia. 2015; 70:326–333.8. Wu JS, Goldsmith JD, Horwich PJ, Shetty SK, Hochman MG. Bone and soft-tissue lesions: what factors affect diagnostic yield of image-guided core-needle biopsy? Radiology. 2008; 248:962–970.9. Song HS, Kim DY, Yoon KS. Intervention using ultrasonography. J Korean Orthop Assoc. 2013; 48:342–349.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Ultrasound-Fine Needle Aspiration versus Core Biopsy for the Diagnosis of Subepithelial Tumors
- Usefulness of Ultrasound-Guided Automated Core Biopsy of Nonpalpable Breast Lesions
- Fine-Needle Biopsy: Should This Be the First Choice in Endoscopic Ultrasound-Guided Tissue Acquisition?
- Breast Lesions with Discordant Results on Ultrasound-guided Core Needle Biopsy
- Clinical Application of Ultrasound-guided Core Needle Biopsy of the Breast