Hip Pelvis.
2018 Dec;30(4):276-281. 10.5371/hp.2018.30.4.276.
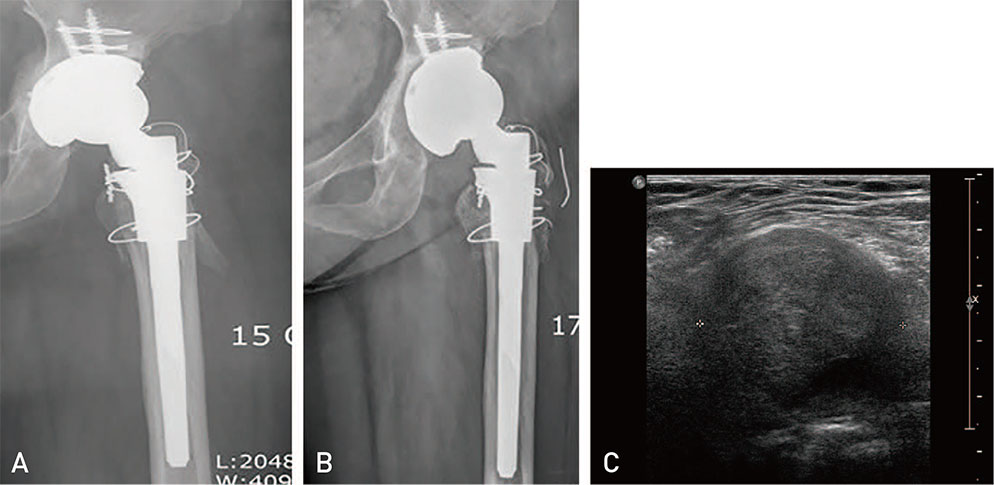
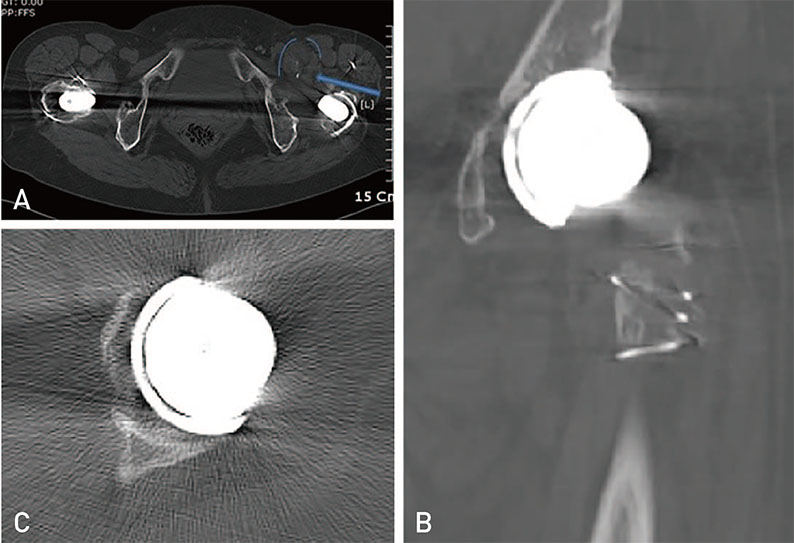
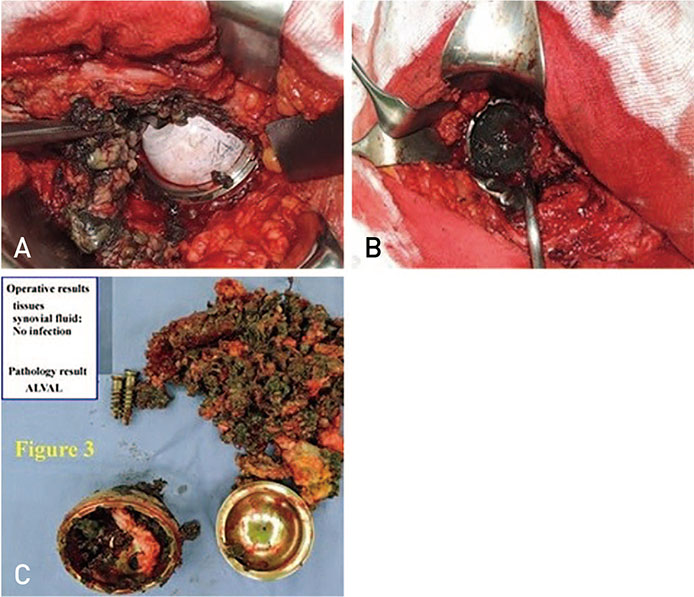
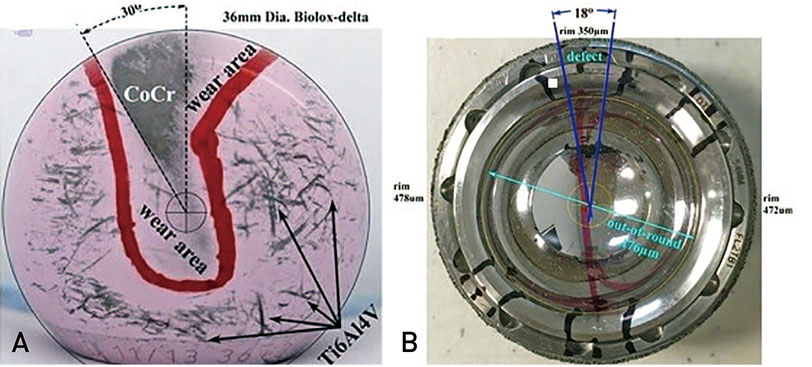
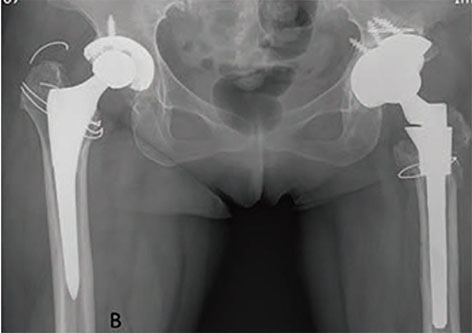
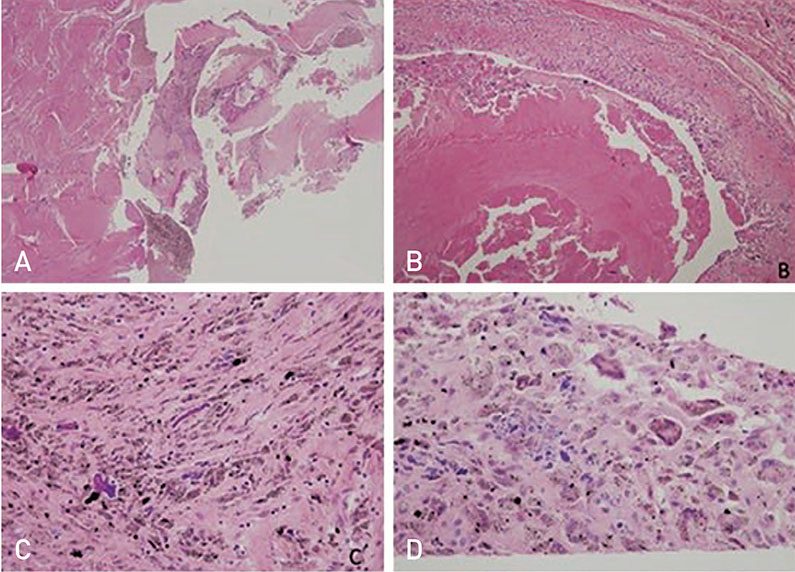
Pseudotumor and Subsequent Implant Loosening as a Complication of Revision Total Hip Arthroplasty with Ceramic-on-Metal Bearing: A Case Report
- Affiliations
-
- 1Department of Arthroplasty, Korea University Guro Hospital, Seoul, Korea.
- 2Donaldson Arthritis Research Foundation, Colton, CA, USA.
- 3Department of Orthopaedics, Korea University Guro Hospital, Seoul, Korea. heavystone75@gmail.com
- KMID: 2427932
- DOI: http://doi.org/10.5371/hp.2018.30.4.276
Abstract
- Pseudotumors are not uncommon complications after total hip arthroplasty (THA) and may occur due to differences in bearing surfaces of the head and the liner ranging from soft to hard articulation. The most common causes of pseudotumors are foreign-body reaction, hypersensitivity and wear debris. The spectrum of pseudotumor presentation following THA varies greatly-from completely asymptomatic to clear implant failure. We report a case of pseudo-tumor formation with acetabular cup aseptic loosening after revision ceramic-on-metal hip arthroplasty. The patient described herein underwent pseudotumor excision and re-revision complex arthroplasty using a trabecular metal shell and buttress with ceramic-on-polyethylene THA. Surgeons should be aware of the possibility of a pseudotumor when dealing with revisions to help prevent rapid progression of cup loosening and implant failure, and should intervene early to avoid complex arthroplasty procedures.
MeSH Terms
Figure
Cited by 1 articles
-
Total Hip Arthroplasty: Past, Present, and Future. What Has Been Achieved?
Won Yong Shon, Beyoung-Yun Park, Rajsankar N R, Phil Sun Park, Jung Taek Im, Ho Hyun Yun
Hip Pelvis. 2019;31(4):179-189. doi: 10.5371/hp.2019.31.4.179.
Reference
-
1. Daniel J, Holland J, Quigley L, Sprague S, Bhandari M. Pseudotumors associated with total hip arthroplasty. J Bone Joint Surg Am. 2012; 94:86–93.
Article2. Griffiths HJ, Burke J, Bonfiglio TA. Granulomatous pseudotumors in total joint replacement. Skeletal Radiol. 1987; 16:146–152.
Article3. Pandit H, Glyn-Jones S, McLardy-Smith P, et al. Pseudotumours associated with metal-on-metal hip resurfacings. J Bone Joint Surg Br. 2008; 90:847–851.
Article4. Madan S, Jowett RL, Goodwin MI. Recurrent intrapelvic cyst complicating metal-on-metal cemented total hip arthroplasty. Arch Orthop Trauma Surg. 2000; 120:508–510.
Article5. Campbell P, Shimmin A, Walter L, Solomon M. Metal sensitivity as a cause of groin pain in metal-on-metal hip resurfacing. J Arthroplasty. 2008; 23:1080–1085.
Article6. Kwon YM, Ostlere SJ, McLardy-Smith P, Athanasou NA, Gill HS, Murray DW. “Asymptomatic” pseudotumors after metal-on-metal hip resurfacing arthroplasty: prevalence and metal ion study. J Arthroplasty. 2011; 26:511–518.
Article7. Williams S, Schepers A, Isaac G, et al. The 2007 Otto Aufranc Award. Ceramic-on-metal hip arthroplasties: a comparative in vitro and in vivo study. Clin Orthop Relat Res. 2007; 465:23–32.8. Isaac GH, Brockett C, Breckon A, et al. Ceramic-on-metal bearings in total hip replacement: whole blood metal ion levels and analysis of retrieved components. J Bone Joint Surg Br. 2009; 91:1134–1141.9. Reinders J, Sonntag R, Heisel C, Reiner T, Vot L, Kretzer JP. Wear performance of ceramic-on-metal hip bearings. PLoS One. 2013; 8:e73252.
Article10. Hsu AR, Gross CE, Levine BR. Pseudotumor from modular neck corrosion after ceramic-on-polyethylene total hip arthroplasty. Am J Orthop (Belle Mead NJ). 2012; 41:422–426.11. Mont MA, Schmalzried TP. Modern metal-on-metal hip resurfacing: important observations from the first ten years. J Bone Joint Surg Am. 2008; 90:Suppl 3. 3–11.
Article12. Harper GD, Bull T, Cobb AG, Bentley G. Failure of the Ring polyethylene uncemented acetabular cup. J Bone Joint Surg Br. 1995; 77:557–561.
Article13. Williams S, Isaac G, Porter N, Fisher J, Older J. Long-term radiographic assessment of cemented polyethylene acetabular cups. Clin Orthop Relat Res. 2008; 466:366–372.
Article14. Deshmukh AJ, Rathod PA, Rodgers WH, Rodriguez JA. Early failure of a ceramic-on-metal total hip arthroplasty: a case report. JBJS Case Connect. 2012; 2:e25.15. Carli A, Reuven A, Zukor DJ, Antoniou J. Adverse soft-tissue reactions around non-metal-on-metal total hip arthroplasty - a systematic review of the literature. Bull NYU Hosp Jt Dis. 2011; 69:Suppl 1. S47–S51.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Revision Total Hip Arthroplasty after Ceramic Bearing Fractures in Patients Under 60-years Old; Mid-term Results
- Failure of a Metal Femoral Head after Revision Total Hip Arthroplasty for a Ceramic Liner Fracture
- Cementless Revision Total Hip Arthroplasty with Ceramic Articulation
- Cementless Total Hip Arthroplasty Involving Trochanteric Osteotomy without Subtrochanteric Shortening for High Hip Dislocation
- Total Hip Arthroplasty using a Ceramic on Ceramic Bearing Surfaces