Arch Hand Microsurg.
2018 Dec;23(4):239-247. 10.12790/ahm.2018.23.4.239.
Reduction Loss after Extension Block Kirschner Wire Fixation for Treatment of Bony Mallet Finger
- Affiliations
-
- 1Department of Orthopedic Surgery, Soonchunhyang University Bucheon Hospital, Bucheon, Korea.
- 2Department of Orthopedic Surgery, Soonchunhyang University Seoul Hospital, Seoul, Korea.
- 3Department of Orthopedic Surgery, Soonchunhyang University Cheonan Hospital, Cheonan, Korea.
- 4Department of Orthopedic Surgery, Seogwipo Medical Center, Seogwipo, Korea. haruki0@naver.com
- KMID: 2427389
- DOI: http://doi.org/10.12790/ahm.2018.23.4.239
Abstract
- PURPOSE
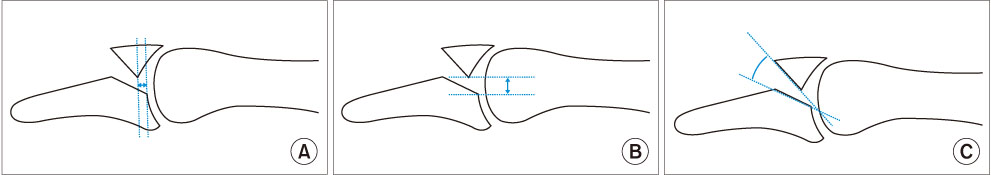
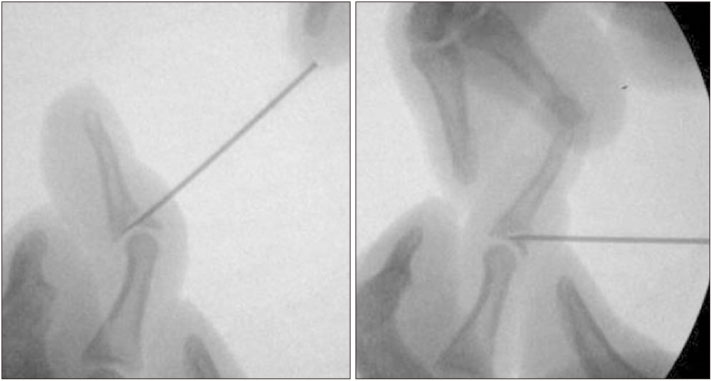
We investigated occurrence of reduction loss after extension block (EB) Kirschner wire fixation or additional interfragmentary fixation (AIF) and clinical results including extension lag of the distal interphalangeal joint for treating bony mallet finger.
METHODS
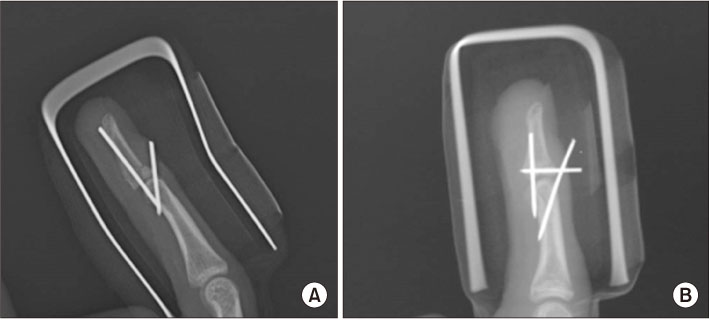
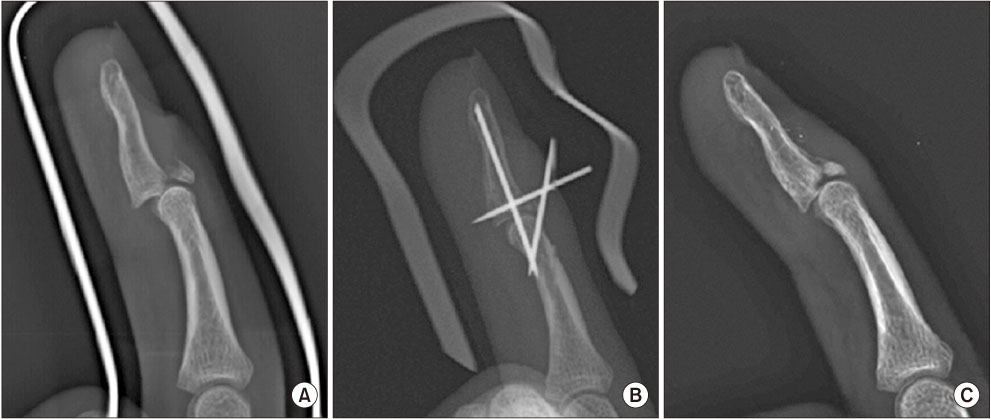
Forty-six patients were included with a mean follow-up of 28 months (range, 12-54 months). Twenty-seven patients were treated with EB K-wire fixation (Group A) while 19 patients were treated with AIF (Group B). We checked radiologic factors, such as amount of articular involvement, volar subluxation, mallet fragment angle, reduction loss, range of motion including extension lag, and functional outcomes using Crawford's criteria.
RESULTS
Reduction loss occurred in eight patients (17%). Differences in mean extension lag, age, preoperative volar subluxation and mallet fragment angle between patients with reduction loss and those with reduction maintaining were significant. However, there were no significant differences in gender, hand dominance, amount of articular involvement, AIF, or further flexion between reduction loss and reduction maintaining. As for patterns of displacement, there was a significant relationship between gap or step-off and extension lag. Using Crawford's evaluation criteria, functional outcomes were excellent in 31, good in 10, fair in 3, and poor in 2 patients.
CONCLUSION
Reduction loss should be careful in older age, smaller mallet fragment angle and preoperative volar subluxation.
Figure
Reference
-
1. Tetik C, Gudemez E. Modification of the extension block kirschner wire technique for mallet fractures. Clin Orthop Relat Res. 2002; (404):284–290.
Article2. Pegoli L, Toh S, Arai K, Fukuda A, Nishikawa S, Vallejo IG. The Ishiguro extension block technique for the treatment of mallet finger fracture: indications and clinical results. J Hand Surg Br. 2003; 28:15–17.3. Lee YH, Kim JY, Chung MS, Baek GH, Gong HS, Lee SK. Two extension block kirschner wire technique for mallet finger fractures. J Bone Joint Surg Br. 2009; 91:1478–1481.
Article4. Jörgsholm P, Björkman A, Emmeluth C, Björkman-Burtscher IM. Extension block pinning of mallet fractures. Scand J Plast Reconstr Surg Hand Surg. 2010; 44:54–58.
Article5. Hofmeister EP, Mazurek MT, Shin AY, Bishop AT. Extension block pinning for large mallet fractures. J Hand Surg Am. 2003; 28:453–459.
Article6. Bendre AA, Hartigan BJ, Kalainov DM. Mallet finger. J Am Acad Orthop Surg. 2005; 13:336–344.
Article7. Ishiguro T, Itoh Y, Yabe Y, Hashizume N. Extension block with kirschner wire for fracture dislocation of the distal interphalangeal joint. Tech Hand Up Extrem Surg. 1997; 1:95–102.
Article8. Theivendran K, Mahon A, Rajaratnam V. A novel hook plate fixation technique for the treatment of mallet fractures. Ann Plast Surg. 2007; 58:112–115.
Article9. Lucchina S, Badia A, Dornean V, Fusetti C. Unstable mallet fractures: a comparison between three different techniques in a multicenter study. Chin J Traumatol. 2010; 13:195–200.10. Schweitzer TP, Rayan GM. The terminal tendon of the digital extensor mechanism: part II, kinematic study. J Hand Surg Am. 2004; 29:903–908.
Article11. Hahn SB, Park KH, Choi YR, Kang HJ, Lee JK. Prognostic factors of the extension block technique for the bony mallet finger. J Korean Orthop Assoc. 2010; 45:127–132.
Article12. Crawford GP. The molded polythene splint for mallet finger deformities. J Hand Surg Am. 1984; 9:231–237.
Article13. Wehbé MA, Schneider LH. Mallet fractures. J Bone Joint Surg Am. 1984; 66:658–669.
Article14. Husain SN, Dietz JF, Kalainov DM, Lautenschlager EP. A biomechanical study of distal interphalangeal joint subluxation after mallet fracture injury. J Hand Surg Am. 2008; 33:26–30.
Article15. Pike J, Mulpuri K, Metzger M, Ng G, Wells N, Goetz T. Blinded, prospective, randomized clinical trial comparing volar, dorsal, and custom thermoplastic splinting in treatment of acute mallet finger. J Hand Surg Am. 2010; 35:580–588.
Article16. Segmueller HE. Mallet finger injuries. J Hand Surg Am. 2010; 35:693. author reply 693-4.
Article17. Kim JY, Lee SH. Factors related to distal interphalangeal joint extension loss after extension block pinning of mallet finger fractures. J Hand Surg Am. 2016; 41:414–419.
Article18. Chung DW, Lee JH. Anatomic reduction of mallet fractures using extension block and additional intrafocal pinning techniques. Clin Orthop Surg. 2012; 4:72–76.
Article19. Shin SH, Lee YS, Kang JW, Kang W, Chung YG. Tips under the skin: a simple modification of extension block pinning for mallet fractures. Orthopedics. 2018; 41:e299–e302.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Modified Extension Block Technique Using Conjoined Kirschner Wires for Bony Mallet Fingers
- Closed Reduction and Percutaneous K-Wire Fixation of Bony Mallet Finger Using an 18 Gauge Needle
- Evaluation of Fragment Reduction Feasibility When Treating Bony Mallet Finger Using Extension Block K-Wire Technique
- Treatment of Bony Mallet Finger: Closed Reduction Using Extension Block K-wire
- Osteoarthritis after Extension Block Technique for the Bony Mallet Finger