Ann Hepatobiliary Pancreat Surg.
2018 Nov;22(4):350-358. 10.14701/ahbps.2018.22.4.350.
Comparison analysis of left-side versus right-side resection in bismuth type III hilar cholangiocarcinoma
- Affiliations
-
- 1Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. dw7722.choi@samsung.com
- 2Department of Surgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- KMID: 2427366
- DOI: http://doi.org/10.14701/ahbps.2018.22.4.350
Abstract
- BACKGROUNDS/AIMS
Several studies report worse prognosis after left-side compared to right-side liver resection in patients with perihilar cholangiocarcinoma. In this study, we compared outcomes of left-side and right-side resections for Bismuth type III hilar cholangiocarcinoma and analyzed factors affecting survival.
METHODS
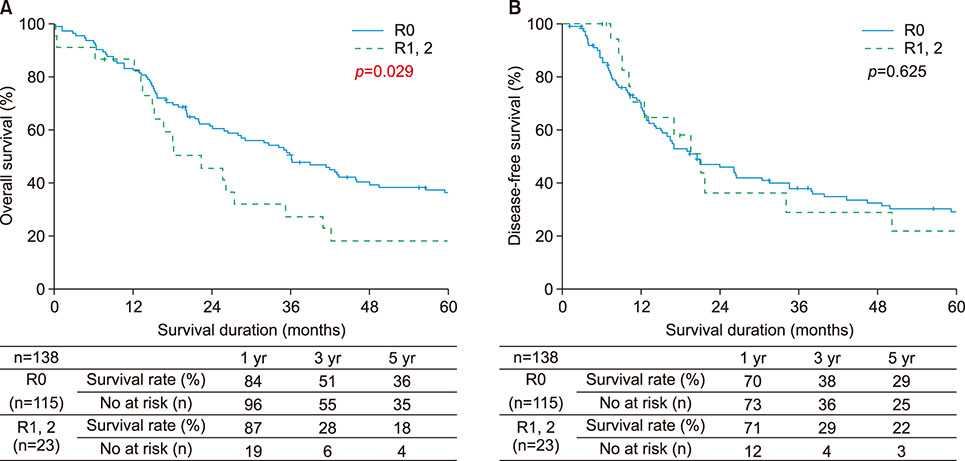
From May 1995 to December 2012, 179 patients underwent surgery at Samsung Medical Center for type III hilar cholangiocarcinoma. Among these patients, 138 received hepatectomies for adenocarcinoma with curative intent: 103 had right-side resections (IIIa group) and 35 had left-side resections (IIIb group). Perioperative demographics, morbidity, mortality, and overall and disease-free survival rates were compared between the groups.
RESULTS
BMI was higher in the IIIa group (24±2.6 kg/m² versus 22.7±2.8 kg/m²; p=0.012). Preoperative portal vein embolization was done in 23.3% of patients in the IIIa group and none in the IIIb group. R0 rate was 82.5% in the IIIa group and 85.7% in the IIIb group (p=0.796) and 3a complications by Clavien-Dindo classification were significantly different between groups (10.7% for IIIa versus 23.3% for IIIb; p=0.002). The 5-year overall survival rate was 33% in the IIIa group and 35% in the IIIb group (p=0.983). The 5-year disease-free survival rate was 28% in the IIIa group and 29% in the IIIb group (p=0.706). Advanced T-stages 3 and 4 and LN metastasis were independent prognostic factors for survival and recurrence by multivariate analysis.
CONCLUSIONS
No significant differences were seen in outcomes by lesion side in patients receiving curative surgery for Bismuth type III hilar cholangiocarcinoma.
MeSH Terms
Figure
Cited by 1 articles
-
Comparison study for surgical outcomes of right versus left side hemihepatectomy to treat hilar cholangiocellular carcinoma
Seung Soo Hong, Dai Hoon Han, Gi Hong Choi, Jin Sub Choi
Ann Surg Treat Res. 2020;98(1):15-22. doi: 10.4174/astr.2020.98.1.15.
Reference
-
1. Soares KC, Kamel I, Cosgrove DP, Herman JM, Pawlik TM. Hilar cholangiocarcinoma: diagnosis, treatment options, and management. Hepatobiliary Surg Nutr. 2014; 3:18–34.2. Klatskin G. Adenocarcinoma of the hepatic duct at its bifurcation within the porta hepatis. An unusual tumor with distinctive clinical and pathological features. Am J Med. 1965; 38:241–256.3. Bismuth H, Corlette MB. Intrahepatic cholangioenteric anastomosis in carcinoma of the hilus of the liver. Surg Gynecol Obstet. 1975; 140:170–178.4. Tompkins RK, Thomas D, Wile A, Longmire WP Jr. Prognostic factors in bile duct carcinoma: analysis of 96 cases. Ann Surg. 1981; 194:447–457.5. Blumgart LH, Hadjis NS, Benjamin IS, Beazley R. Surgical approaches to cholangiocarcinoma at confluence of hepatic ducts. Lancet. 1984; 1:66–70.
Article6. Nakeeb A, Pitt HA, Sohn TA, Coleman J, Abrams RA, Piantadosi S, et al. Cholangiocarcinoma. A spectrum of intrahepatic, perihilar, and distal tumors. Ann Surg. 1996; 224:463–473.7. Seyama Y, Makuuchi M. Current surgical treatment for bile duct cancer. World J Gastroenterol. 2007; 13:1505–1515.
Article8. D'Angelica MI, Jarnagin WR, Blumgart LH. Resectable hilar cholangiocarcinoma: surgical treatment and long-term outcome. Surg Today. 2004; 34:885–890.9. Aljiffry M, Walsh MJ, Molinari M. Advances in diagnosis, treatment and palliation of cholangiocarcinoma: 1990–2009. World J Gastroenterol. 2009; 15:4240–4262.
Article10. Otto G. Diagnostic and surgical approaches in hilar cholangiocarcinoma. Int J Colorectal Dis. 2007; 22:101–108.
Article11. Valero V 3rd, Cosgrove D, Herman JM, Pawlik TM. Management of perihilar cholangiocarcinoma in the era of multimodal therapy. Expert Rev Gastroenterol Hepatol. 2012; 6:481–495.
Article12. Ratti F, Cipriani F, Piozzi G, Catena M, Paganelli M, Aldrighetti L. Comparative analysis of left- versus right-sided resection in klatskin tumor surgery: can lesion side be considered a prognostic factor? J Gastrointest Surg. 2015; 19:1324–1333.
Article13. Seyama Y, Kubota K, Sano K, Noie T, Takayama T, Kosuge T, et al. Long-term outcome of extended hemihepatectomy for hilar bile duct cancer with no mortality and high survival rate. Ann Surg. 2003; 238:73–83.
Article14. Kawasaki S, Imamura H, Kobayashi A, Noike T, Miwa S, Miyagawa S. Results of surgical resection for patients with hilar bile duct cancer: application of extended hepatectomy after biliary drainage and hemihepatic portal vein embolization. Ann Surg. 2003; 238:84–92.15. Ikeyama T, Nagino M, Oda K, Ebata T, Nishio H, Nimura Y. Surgical approach to bismuth Type I and II hilar cholangiocarcinomas: audit of 54 consecutive cases. Ann Surg. 2007; 246:1052–1057.16. Nagino M, Ebata T, Yokoyama Y, Igami T, Sugawara G, Takahashi Y, et al. Evolution of surgical treatment for perihilar cholangiocarcinoma: a single-center 34-year review of 574 consecutive resections. Ann Surg. 2013; 258:129–140.17. Konstadoulakis MM, Roayaie S, Gomatos IP, Labow D, Fiel MI, Miller CM, et al. Aggressive surgical resection for hilar cholangiocarcinoma: is it justified? Audit of a single center's experience. Am J Surg. 2008; 196:160–169.
Article18. Hirose T, Igami T, Ebata T, Yokoyama Y, Sugawara G, Mizuno T, et al. Surgical and radiological studies on the length of the hepatic ducts. World J Surg. 2015; 39:2983–2989.
Article19. Natsume S, Ebata T, Yokoyama Y, Igami T, Sugawara G, Shimoyama Y, et al. Clinical significance of left trisectionectomy for perihilar cholangiocarcinoma: an appraisal and comparison with left hepatectomy. Ann Surg. 2012; 255:754–762.20. Hosokawa I, Shimizu H, Yoshidome H, Ohtsuka M, Kato A, Yoshitomi H, et al. Surgical strategy for hilar cholangiocarcinoma of the left-side predominance: current role of left trisectionectomy. Ann Surg. 2014; 259:1178–1185.21. Shimizu H, Kimura F, Yoshidome H, Ohtsuka M, Kato A, Yoshitomi H, et al. Aggressive surgical resection for hilar cholangiocarcinoma of the left-side predominance: radicality and safety of left-sided hepatectomy. Ann Surg. 2010; 251:281–286.22. Launois B, Campion JP, Brissot P, Gosselin M. Carcinoma of the hepatic hilus. Surgical management and the case for resection. Ann Surg. 1979; 190:151–157.
Article23. Bengmark S, Ekberg H, Evander A, Klofver-Stahl B, Tranberg KG. Major liver resection for hilar cholangiocarcinoma. Ann Surg. 1988; 207:120–125.
Article24. Boerma EJ. Research into the results of resection of hilar bile duct cancer. Surgery. 1990; 108:572–580.25. Launois B, Terblanche J, Lakehal M, Catheline JM, Bardaxoglou E, Landen S, et al. Proximal bile duct cancer: high resectability rate and 5-year survival. Ann Surg. 1999; 230:266–275.
Article26. Sugiura Y, Nakamura S, Iida S, Hosoda Y, Ikeuchi S, Mori S, et al. Extensive resection of the bile ducts combined with liver resection for cancer of the main hepatic duct junction: a cooperative study of the Keio Bile Duct Cancer Study Group. Surgery. 1994; 115:445–451.27. Pichlmayr R, Weimann A, Klempnauer J, Oldhafer KJ, Maschek H, Tusch G, et al. Surgical treatment in proximal bile duct cancer. A single-center experience. Ann Surg. 1996; 224:628–638.28. Klempnauer J, Ridder GJ, von Wasielewski R, Werner M, Weimann A, Pichlmayr R. Resectional surgery of hilar cholangiocarcinoma: a multivariate analysis of prognostic factors. J Clin Oncol. 1997; 15:947–954.
Article29. Nagino M, Nimura Y, Kamiya J, Kanai M, Uesaka K, Hayakawa N, et al. Segmental liver resections for hilar cholangiocarcinoma. Hepatogastroenterology. 1998; 45:7–13.30. Neuhaus P, Jonas S, Bechstein WO, Lohmann R, Radke C, Kling N, et al. Extended resections for hilar cholangiocarcinoma. Ann Surg. 1999; 230:808–818.
Article31. Miyazaki M, Ito H, Nakagawa K, Ambiru S, Shimizu H, Okaya T, et al. Parenchyma-preserving hepatectomy in the surgical treatment of hilar cholangiocarcinoma. J Am Coll Surg. 1999; 189:575–583.
Article32. Kosuge T, Yamamoto J, Shimada K, Yamasaki S, Makuuchi M. Improved surgical results for hilar cholangiocarcinoma with procedures including major hepatic resection. Ann Surg. 1999; 230:663–671.
Article33. Jarnagin WR, Fong Y, DeMatteo RP, Gonen M, Burke EC, Bodniewicz BS J, et al. Staging, resectability, and outcome in 225 patients with hilar cholangiocarcinoma. Ann Surg. 2001; 234:507–517.
Article34. Paik KY, Choi DW, Chung JC, Kang KT, Kim SB. Improved survival following right trisectionectomy with caudate lobectomy without operative mortality: surgical treatment for hilar cholangiocarcinoma. J Gastrointest Surg. 2008; 12:1268–1274.
Article35. Gazzaniga GM, Ciferri E, Bagarolo C, Filauro M, Bondanza G, Fazio S, et al. Primitive hepatic hilum neoplasm. J Surg Oncol Suppl. 1993; 3:140–146.36. Tsao JI, Nimura Y, Kamiya J, Hayakawa N, Kondo S, Nagino M, et al. Management of hilar cholangiocarcinoma: comparison of an American and a Japanese experience. Ann Surg. 2000; 232:166–174.37. Fortner JG, Vitelli CE, Maclean BJ. Proximal extrahepatic bile duct tumors. Analysis of a series of 52 consecutive patients treated over a period of 13 years. Arch Surg. 1989; 124:1275–1279.38. Bismuth H, Nakache R, Diamond T. Management strategies in resection for hilar cholangiocarcinoma. Ann Surg. 1992; 215:31–38.
Article39. Lygidakis NJ, van der, Houthoff HJ. Surgical approaches to the management of primary biliary cholangiocarcinoma of the porta hepatis: the decision-making dilemma. Hepatogastroenterology. 1988; 35:261–267.40. Lee SG, Song GW, Hwang S, Ha TY, Moon DB, Jung DH, et al. Surgical treatment of hilar cholangiocarcinoma in the new era: the Asan experience. J Hepatobiliary Pancreat Sci. 2010; 17:476–489.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Preliminary Study on the Usefullness of a Zilver Stent for Bilateral Stenting in Patients withAdvanced Hilar Cholangiocarcinoma
- Role of resection for Bismuth type IV hilar cholangiocarcinoma and analysis of determining factors for curative resection
- TNM Staging of Hilar Cholangiocarcinoma
- Endoscopic Staging of Hilar Cholangiocarcinoma
- Bilateral Metallic Stenting in Malignant Hilar Obstruction