Korean J Radiol.
2017 ;18(4):655-663. 10.3348/kjr.2017.18.4.655.
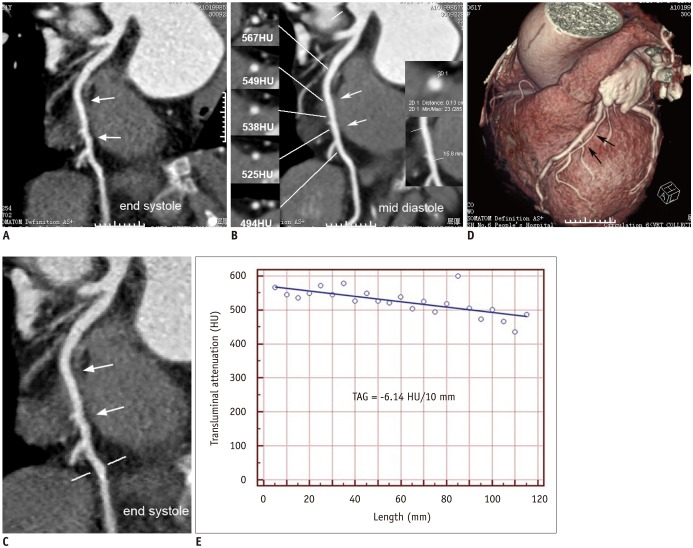
Assessment of Myocardial Bridge by Cardiac CT: Intracoronary Transluminal Attenuation Gradient Derived from Diastolic Phase Predicts Systolic Compression
- Affiliations
-
- 1Institute of Diagnostic and Interventional Radiology, Shanghai Jiao Tong University Affiliated Sixth People's Hospital, Shanghai 200233, China. andrewssmu@msn.com
- 2Department of Pharmaceutical Science, School of Pharmacy, The Second Military Medical University, Shanghai 200433, China.
- 3Department of Scientific Research, TongRen Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai 200050, China.
- KMID: 2427234
- DOI: http://doi.org/10.3348/kjr.2017.18.4.655
Abstract
OBJECTIVE
To study the predictive value of transluminal attenuation gradient (TAG) derived from diastolic phase of coronary computed tomography angiography (CCTA) for identifying systolic compression of myocardial bridge (MB).
MATERIALS AND METHODS
Consecutive patients diagnosed with MB based on CCTA findings and without obstructive coronary artery disease were retrospectively enrolled. In total, 143 patients with 144 MBs were included in the study. Patients were classified into three groups: without systolic compression, with systolic compression < 50%, and with systolic compression ≥ 50%. TAG was defined as the linear regression coefficient between intraluminal attenuation in Hounsfield units (HU) and length from the vessel ostium. Other indices such as the length and depth of the MB were also recorded.
RESULTS
TAG was the lowest in MB patients with systolic compression ≥ 50% (−19.9 ± 8.7 HU/10 mm). Receiver operating characteristic curve analysis was performed to determine the optimal cutoff values for identifying systolic compression ≥ 50%. The result indicated an optimal cutoff value of TAG as −18.8 HU/10 mm (area under curve = 0.778, p < 0.001), which yielded higher sensitivity, specificity, positive predictive value, negative predictive value, and diagnostic accuracy (54.1, 80.5, 72.8, and 75.0%, respectively). In addition, the TAG of MB with diastolic compression was significantly lower than the TAG of MB without diastolic compression (−21.4 ± 4.8 HU/10 mm vs. −12.7 ± 8 HU/10 mm, p < 0.001).
CONCLUSION
TAG was a better predictor of MB with systolic compression ≥ 50%, compared to the length or depth of the MB. The TAG of MB with persistent diastolic compression was significantly lower than the TAG without diastolic compression.
Keyword
MeSH Terms
-
Adult
Aged
Aged, 80 and over
Area Under Curve
Blood Pressure/physiology
Coronary Angiography
Female
Humans
Image Processing, Computer-Assisted
Linear Models
Male
Middle Aged
Myocardial Bridging/diagnosis/*diagnostic imaging
ROC Curve
Retrospective Studies
Sensitivity and Specificity
Severity of Illness Index
*Tomography, X-Ray Computed
Young Adult
Figure
Cited by 1 articles
-
Age of Data in Contemporary Research Articles Published in Representative General Radiology Journals
Ji Hun Kang, Dong Hwan Kim, Seong Ho Park, Jung Hwan Baek
Korean J Radiol. 2018;19(6):1172-1178. doi: 10.3348/kjr.2018.19.6.1172.
Reference
-
1. Möhlenkamp S, Hort W, Ge J, Erbel R. Update on myocardial bridging. Circulation. 2002; 106:2616–2622. PMID: 12427660.
Article2. Akdemir R, Gunduz H, Emiroglu Y, Uyan C. Myocardial bridging as a cause of acute myocardial infarction: a case report. BMC Cardiovasc Disord. 2002; 2:15. PMID: 12243650.
Article3. Kim SS, Jeong MH, Kim HK, Kim MC, Cho KH, Lee MG, et al. Long-term clinical course of patients with isolated myocardial bridge. Circ J. 2010; 74:538–543. PMID: 20103971.
Article4. Gowda RM, Khan IA, Ansari AW, Cohen RA. Acute ST segment elevation myocardial infarction from myocardial bridging of left anterior descending coronary artery. Int J Cardiol. 2003; 90:117–118. PMID: 12821227.
Article5. Nakanishi R, Rajani R, Ishikawa Y, Ishii T, Berman DS. Myocardial bridging on coronary CTA: an innocent bystander or a culprit in myocardial infarction? J Cardiovasc Comput Tomogr. 2012; 6:3–13. PMID: 22264630.
Article6. Gawor R, Kuśmierek J, Płachcińska A, Bieńkiewicz M, Drożdż J, Piotrowski G, et al. Myocardial perfusion GSPECT imaging in patients with myocardial bridging. J Nucl Cardiol. 2011; 18:1059–1065. PMID: 21822768.
Article7. Lee YS, Moon DH, Shin JW, Park SW, Park SJ, Lee HK. Dipyridamole TI-201 SPECT imaging in patients with myocardial bridging. Clin Nucl Med. 1999; 24:759–764. PMID: 10512101.8. Hwang JH, Ko SM, Roh HG, Song MG, Shin JK, Chee HK, et al. Myocardial bridging of the left anterior descending coronary artery: depiction rate and morphologic features by dual-source CT coronary angiography. Korean J Radiol. 2010; 11:514–521. PMID: 20808694.
Article9. Hirai N, Horiguchi J, Fujioka C, Kiguchi M, Yamamoto H, Matsuura N, et al. Prospective versus retrospective ECG-gated 64-detector coronary CT angiography: assessment of image quality, stenosis, and radiation dose. Radiology. 2008; 248:424–430. PMID: 18574140.
Article10. Leschka S, Koepfli P, Husmann L, Plass A, Vachenauer R, Gaemperli O, et al. Myocardial bridging: depiction rate and morphology at CT coronary angiography--comparison with conventional coronary angiography. Radiology. 2008; 246:754–762. PMID: 18223120.
Article11. Machida H, Tanaka I, Fukui R, Shen Y, Ishikawa T, Tate E, et al. Current and novel imaging techniques in coronary CT. Radiographics. 2015; 35:991–1010. PMID: 26046942.
Article12. Bourassa MG, Butnaru A, Lespérance J, Tardif JC. Symptomatic myocardial bridges: overview of ischemic mechanisms and current diagnostic and treatment strategies. J Am Coll Cardiol. 2003; 41:351–359. PMID: 12575960.
Article13. Steigner ML, Mitsouras D, Whitmore AG, Otero HJ, Wang C, Buckley O, et al. Iodinated contrast opacification gradients in normal coronary arteries imaged with prospectively ECG-gated single heart beat 320-detector row computed tomography. Circ Cardiovasc Imaging. 2010; 3:179–186. PMID: 20044512.
Article14. Choi JH, Min JK, Labounty TM, Lin FY, Mendoza DD, Shin DH, et al. Intracoronary transluminal attenuation gradient in coronary CT angiography for determining coronary artery stenosis. JACC Cardiovasc Imaging. 2011; 4:1149–1157. PMID: 22093264.
Article15. Kim PJ, Hur G, Kim SY, Namgung J, Hong SW, Kim YH, et al. Frequency of myocardial bridges and dynamic compression of epicardial coronary arteries: a comparison between computed tomography and invasive coronary angiography. Circulation. 2009; 119:1408–1416. PMID: 19255347.16. Kramer JR, Kitazume H, Proudfit WL, Sones FM Jr. Clinical significance of isolated coronary bridges: benign and frequent condition involving the left anterior descending artery. Am Heart J. 1982; 103:283–288. PMID: 7055058.
Article17. Schwarz ER, Gupta R, Haager PK, vom Dahl J, Klues HG, Minartz J, et al. Myocardial bridging in absence of coronary artery disease: proposal of a new classification based on clinical-angiographic data and long-term follow-up. Cardiology. 2009; 112:13–21. PMID: 18577881.
Article18. Ishikawa Y, Akasaka Y, Suzuki K, Fujiwara M, Ogawa T, Yamazaki K, et al. Anatomic properties of myocardial bridge predisposing to myocardial infarction. Circulation. 2009; 120:376–383. PMID: 19620504.
Article19. Kim YJ, Yong HS, Kim SM, Kim JA, Yang DH, Hong YJ, et al. Korean guidelines for the appropriate use of cardiac CT. Korean J Radiol. 2015; 16:251–285. PMID: 25741189.
Article20. Hwang D, Lee JM, Koo BK. Physiologic assessment of coronary artery disease: focus on fractional flow reserve. Korean J Radiol. 2016; 17:307–320. PMID: 27134520.
Article21. Corban MT, Hung OY, Eshtehardi P, Rasoul-Arzrumly E, McDaniel M, Mekonnen G, et al. Myocardial bridging: contemporary understanding of pathophysiology with implications for diagnostic and therapeutic strategies. J Am Coll Cardiol. 2014; 63:2346–2355. PMID: 24583304.22. Herrmann J, Higano ST, Lenon RJ, Rihal CS, Lerman A. Myocardial bridging is associated with alteration in coronary vasoreactivity. Eur Heart J. 2004; 25:2134–2142. PMID: 15571829.
Article23. Soran O, Pamir G, Erol C, Kocakavak C, Sabah I. The incidence and significance of myocardial bridge in a prospectively defined population of patients undergoing coronary angiography for chest pain. Tokai J Exp Clin Med. 2000; 25:57–60. PMID: 11127508.24. Uusitalo V, Saraste A, Pietilä M, Kajander S, Bax JJ, Knuuti J. The functional effects of intramural course of coronary arteries and its relation to coronary atherosclerosis. JACC Cardiovasc Imaging. 2015; 8:697–704. PMID: 25981503.
Article25. Sun Z, Ng KH. Prospective versus retrospective ECG-gated multislice CT coronary angiography: a systematic review of radiation dose and diagnostic accuracy. Eur J Radiol. 2012; 81:e94–e100. PMID: 21316887.
Article26. Ko BS, Cameron JD, Leung M, Meredith IT, Leong DP, Antonis PR, et al. Combined CT coronary angiography and stress myocardial perfusion imaging for hemodynamically significant stenoses in patients with suspected coronary artery disease: a comparison with fractional flow reserve. JACC Cardiovasc Imaging. 2012; 5:1097–1111. PMID: 23153909.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Attenuation Drop of Intra-Mural Coronary Segment Observed at Diastolic Phase of Coronary CT Angiography Predicts Significant Systolic Compression of Myocardial Bridge
- Coronary Flow Velocity Pattern in Patients with Myocardial Bridging of Coronary Artery
- CT Fractional Flow Reserve for the Diagnosis of Myocardial Bridging-Related Ischemia: A Study Using Dynamic CT Myocardial Perfusion Imaging as a Reference Standard
- Myocardial Infarction in a Patient with Myocardial Bridge and Pheochromocytoma: A case report
- Current Roles and Future Applications of Cardiac CT: Risk Stratification of Coronary Artery Disease