Obstet Gynecol Sci.
2018 Sep;61(5):605-614. 10.5468/ogs.2018.61.5.605.
Interrelationships among endometriosis-related pain symptoms and their effects on health-related quality of life: a sectional observational study
- Affiliations
-
- 1Departments of Gynecology and Anesthesia, Fernandes Figueira National Institute for Women, Children and Youth Health (IFF), Oswaldo Cruz Foundation, Rio de Janeiro, Brazil. marlon@iff.fiocruz.br, marlon.iff@gmail.com
- 2Crispi Institute of Minimally Invasive Surgery, Rio de Janeiro, Brazil.
- 3Department of Urology, Lagoa Federal Hospital, Rio de Janeiro, Brazil.
- 4Department of Urology, Pedro Ernesto University Hospital, Rio de Janeiro State University, Rio de Janeiro, Brazil.
- KMID: 2426026
- DOI: http://doi.org/10.5468/ogs.2018.61.5.605
Abstract
OBJECTIVE
To assess the correlation between different pain symptoms and different domains of women's health-related quality of life (HRQoL).
METHODS
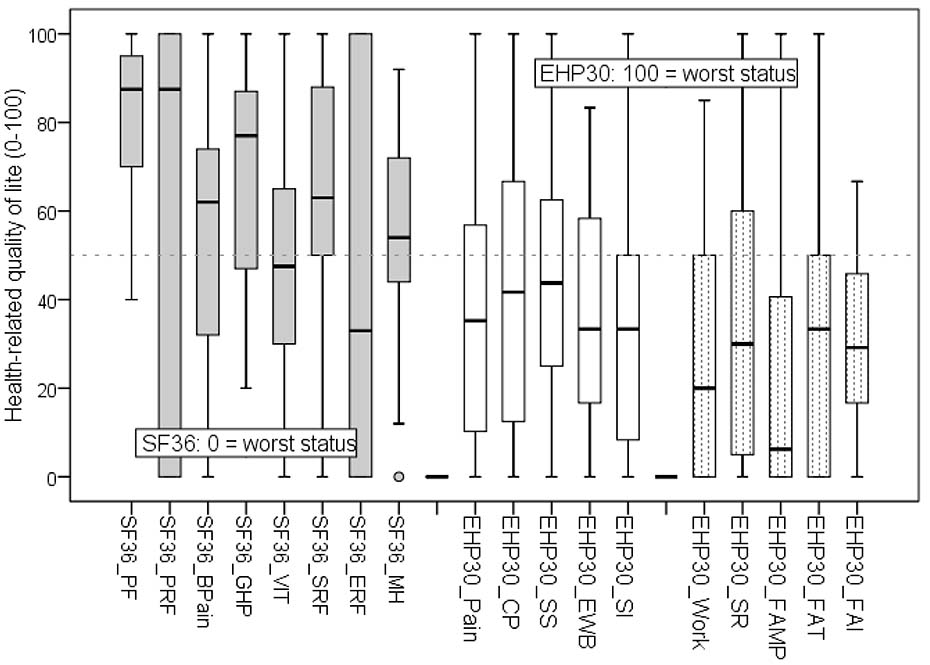
Seventy-seven women with deep infiltrating endometriosis were successively enrolled between June 2011 and August 2013 while being prepared to undergo laparoscopy due to pain and/or infertility. We quantified the intensities of dysmenorrhea, deep dyspareunia, chronic pelvic pain, and dyschezia (menstrual and non-menstrual) using a 11-point visual analog scale (VAS: 0-10) and the validated full versions of the Short Form 36 (SF36) and Endometriosis Health Profile (EHP30) questionnaires to assess HRQoL. The pain symptoms were considered simultaneously in a hierarchical agglomerative clustering method (exploratory multivariate approach) and the associations among scores were tested by bivariate correlation.
RESULTS
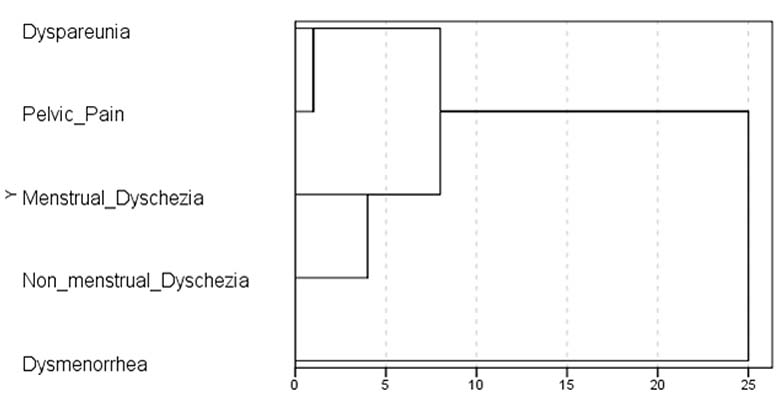
Dysmenorrhea showed the lowest similarity on to the multivariate cluster analysis and no statistically significant correlation with the other pain symptoms: deep dyspareunia (P=0.244), chronic pelvic pain (P=0.108), menstrual dyschezia (P=0.238), and non-menstrual dyschezia (P=0.380). Dysmenorrhea and chronic pelvic pain were the main symptoms correlated with all domains of the SF36 and the EHP30 (core instrument) questionnaires (P < 0.05).
CONCLUSION
Dysmenorrhea and chronic pelvic pain were independent factors associated with HRQoL.
Keyword
MeSH Terms
Figure
Reference
-
1. Eriksen HL, Gunnersen KF, Sørensen JA, Munk T, Nielsen T, Knudsen UB. Psychological aspects of endometriosis: differences between patients with or without pain on four psychological variables. Eur J Obstet Gynecol Reprod Biol. 2008; 139:100–105.
Article2. Facchin F, Barbara G, Saita E, Mosconi P, Roberto A, Fedele L, et al. Impact of endometriosis on quality of life and mental health: pelvic pain makes the difference. J Psychosom Obstet Gynaecol. 2015; 36:135–141.
Article3. Laganà AS, Condemi I, Retto G, Muscatello MR, Bruno A, Zoccali RA, et al. Analysis of psychopathological comorbidity behind the common symptoms and signs of endometriosis. Eur J Obstet Gynecol Reprod Biol. 2015; 194:30–33.
Article4. Warren JW, Clauw DJ, Wesselmann U, Howard FM, Gallicchio L, Morozov V. Functional somatic syndromes as risk factors for hysterectomy in early bladder pain syndrome/interstitial cystitis. J Psychosom Res. 2014; 77:363–367.
Article5. Cornillie FJ, Oosterlynck D, Lauweryns JM, Koninckx PR. Deeply infiltrating pelvic endometriosis: histology and clinical significance. Fertil Steril. 1990; 53:978–983.
Article6. Vercellini P. Introduction: Management of endometriosis: moving toward a problem-oriented and patient-centered approach. Fertil Steril. 2015; 104:761–763.7. Ferrero S, Alessandri F, Racca A, Leone Roberti Maggiore U. Treatment of pain associated with deep endometriosis: alternatives and evidence. Fertil Steril. 2015; 104:771–792.
Article8. Porto BT, Ribeiro HS, Galvão MA, Sekula VG, Aldrigui JM, Ribeiro PA. Histological classification and quality of life in women with endometriosis. Rev Bras Ginecol Obstet. 2015; 37:87–93.9. de Freitas Fonseca M, Sessa FV, de Carvalho Aragao L, de Resende JA. Junior, Crispi CP. The association between dyspareunia and dysmenorrhea in women with deep endometriosis: a pre-planned observational study. Ann Public Health Res. 2015; 2:1018.10. Evangelista A, Dantas T, Zendron C, Soares T, Vaz G, Oliveira MA. Sexual function in patients with deep infiltrating endometriosis. J Sex Med. 2014; 11:140–145.
Article11. Fauconnier A, Chapron C, Dubuisson JB, Vieira M, Dousset B, Bréart G. Relation between pain symptoms and the anatomic location of deep infiltrating endometriosis. Fertil Steril. 2002; 78:719–726.
Article12. Fauconnier A, Staraci S, Huchon C, Roman H, Panel P, Descamps P. Comparison of patient- and physician-based descriptions of symptoms of endometriosis: a qualitative study. Hum Reprod. 2013; 28:2686–2694.
Article13. Lukic A, Di Properzio M, De Carlo S, Nobili F, Schimberni M, Bianchi P, et al. Quality of sex life in endometriosis patients with deep dyspareunia before and after laparoscopic treatment. Arch Gynecol Obstet. 2016; 293:583–590.
Article14. Nnoaham KE, Hummelshoj L, Webster P, d'Hooghe T, de Cicco Nardone F, de Cicco Nardone C, et al. Impact of endometriosis on quality of life and work productivity: a multicenter study across ten countries. Fertil Steril. 2011; 96:366–373.e8.
Article15. Minson FP, Abrão MS, Sardá Júnior J, Kraychete DC, Podgaec S, Assis FD. Importance of quality of life assessment in patients with endometriosis. Rev Bras Ginecol Obstet. 2012; 34:11–15.16. Medeiros LR, Rosa MI, Silva BR, Reis ME, Simon CS, Dondossola ER, et al. Accuracy of magnetic resonance in deeply infiltrating endometriosis: a systematic review and meta-analysis. Arch Gynecol Obstet. 2015; 291:611–621.
Article17. Gerlinger C, Schumacher U, Faustmann T, Colligs A, Schmitz H, Seitz C. Defining a minimal clinically important difference for endometriosis-associated pelvic pain measured on a visual analog scale: analyses of two placebo-controlled, randomized trials. Health Qual Life Outcomes. 2010; 8:138.
Article18. Bourdel N, Alves J, Pickering G, Ramilo I, Roman H, Canis M. Systematic review of endometriosis pain assessment: how to choose a scale? Hum Reprod Update. 2015; 21:136–152.
Article19. Stull DE, Wasiak R, Kreif N, Raluy M, Colligs A, Seitz C, et al. Validation of the SF-36 in patients with endometriosis. Qual Life Res. 2014; 23:103–117.
Article20. Mengarda CV, Passos EP, Picon P, Costa AF, Picon PD. Validation of Brazilian Portuguese version of quality of life questionnaire for women with endometriosis (Endometriosis Health Profile Questionnaire--EHP-30). Rev Bras Ginecol Obstet. 2008; 30:384–392.
Article21. Fonseca MF, De Souza Hacon S, Grandjean P, Choi AL, Bastos WR. Iron status as a covariate in methylmercury-associated neurotoxicity risk. Chemosphere. 2014; 100:89–96.
Article22. Campbell F, Collett BJ. Chronic pelvic pain. Br J Anaesth. 1994; 73:571–573.
Article23. De Graaff AA, Van Lankveld J, Smits LJ, Van Beek JJ, Dunselman GA. Dyspareunia and depressive symptoms are associated with impaired sexual functioning in women with endometriosis, whereas sexual functioning in their male partners is not affected. Hum Reprod. 2016; 31:2577–2586.
Article24. Vercellini P, Somigliana E, Buggio L, Barbara G, Frattaruolo MP, Fedele L. “I can't get no satisfaction”: deep dyspareunia and sexual functioning in women with rectovaginal endometriosis. Fertil Steril. 2012; 98:1503–1511.e1.25. Setälä M, Härkki P, Matomäki J, Mäkinen J, Kössi J. Sexual functioning, quality of life and pelvic pain 12 months after endometriosis surgery including vaginal resection. Acta Obstet Gynecol Scand. 2012; 91:692–698.26. de Resende JA Júnior, Cavalini LT, Crispi CP, de Freitas Fonseca M. Risk of urinary retention after nerve-sparing surgery for deep infiltrating endometriosis: a systematic review and meta-analysis. Neurourol Urodyn. 2017; 36:57–61.
Article27. Oliveira MA, Pereira TR, Gilbert A, Tulandi T, de Oliveira HC, De Wilde RL. Bowel complications in endometriosis surgery. Best Pract Res Clin Obstet Gynaecol. 2016; 35:51–62.
Article28. Myles PS, Troedel S, Boquest M, Reeves M. The pain visual analog scale: is it linear or nonlinear? Anesth Analg. 1999; 89:1517–1520.
Article29. Barbara G, Facchin F, Meschia M, Berlanda N, Frattaruolo MP, Vercellin IP. When love hurts. A systematic review on the effects of surgical and pharmacological treatments for endometriosis on female sexual functioning. Acta Obstet Gynecol Scand. 2017; 96:668–687.
Article30. Dubernard G, Rouzier R, David-Montefiore E, Bazot M, Darai E. Use of the SF-36 questionnaire to predict quality-of-life improvement after laparoscopic colorectal resection for endometriosis. Hum Reprod. 2008; 23:846–851.
Article31. Vercellini P, Frattaruolo MP, Somigliana E, Jones GL, Consonni D, Alberico D, et al. Surgical versus low-dose progestin treatment for endometriosis-associated severe deep dyspareunia II: effect on sexual functioning, psychological status and health-related quality of life. Hum Reprod. 2013; 28:1221–1230.
Article32. Touboul C, Ballester M, Dubernard G, Zilberman S, Thomin A, Daraï E. Long-term symptoms, quality of life, and fertility after colorectal resection for endometriosis: extended analysis of a randomized controlled trial comparing laparoscopically assisted to open surgery. Surg Endosc. 2015; 29:1879–1887.
Article33. De Graaff AA, D'Hooghe TM, Dunselman GA, Dirksen CD, Hummelshoj L. The significant effect of endometriosis on physical, mental and social wellbeing: results from an international cross-sectional survey. Hum Reprod. 2013; 28:2677–2685.
Article34. Barbara G, Facchin F, Buggio L, Somigliana E, Berlanda N, Kustermann A, et al. What is known and unknown about the association between endometriosis and sexual functioning: a systematic review of the literature. Reprod Sci. 2017; 24:1566–1576.
Article35. Rogers PA, Adamson GD, Al-Jefout M, Becker CM, D'Hooghe TM, Dunselman GA, et al. Research priorities for endometriosis. Reprod Sci. 2017; 24:202–226.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Frailty on Health-related Quality of Life of Rural Community-dwelling Elderly: Mediating and Moderating Effects of Fall-Related Efficacy and Social Support
- Correlations among Total Symptom Distress, Uncertainty and Quality of Life among Women With Endometriosis
- Relationship between Low Back Pain and Health-Related Quality of Life among Some Elderly
- Mediating Effect of Physical Activity in the Relationship between Depressive Symptoms and Health-related Quality of Life in Patients with Coronary Artery Disease: The 2016 Nationwide Community Health Survey in Korea
- The Effects of Related Factors on Health-related Quality of Life for the Frail Elderly