Ann Lab Med.
2017 Nov;37(6):511-515. 10.3343/alm.2017.37.6.511.
Comparison of Traditional and Reverse Syphilis Screening Algorithms in Medical Health Checkups
- Affiliations
-
- 1Department of Laboratory Medicine and Health Promotion Research Institute, Korea Association of Health Promotion, Seoul, Korea. cellonah@hanmail.net
- 2MEDIcheck LAB, Korea Association of Health Promotion, Cheongju, Korea.
- 3Institute of Parasitic Diseases, Korea Association of Health Promotion, Seoul, Korea.
- KMID: 2425992
- DOI: http://doi.org/10.3343/alm.2017.37.6.511
Abstract
- BACKGROUND
The syphilis diagnostic algorithms applied in different countries vary significantly depending on the local syphilis epidemiology and other considerations, including the expected workload, the need for automation in the laboratory and budget factors. This study was performed to investigate the efficacy of traditional and reverse syphilis diagnostic algorithms during general health checkups.
METHODS
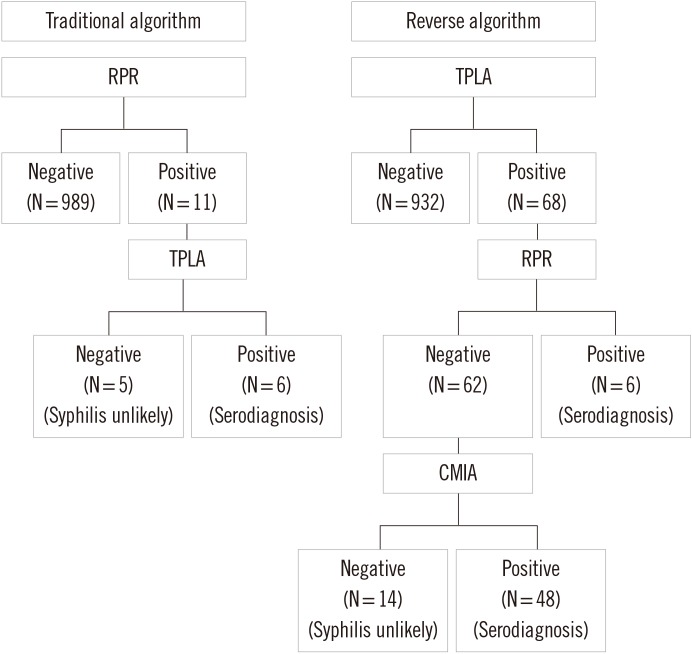
In total, 1,000 blood specimens were obtained from 908 men and 92 women during their regular health checkups. Traditional screening and reverse screening were applied to the same specimens using automatic rapid plasma regain (RPR) and Treponema pallidum latex agglutination (TPLA) tests, respectively. Specimens that were reverse algorithm (TPLA) reactive, were subjected to a second treponemal test performed by using the chemiluminescent microparticle immunoassay (CMIA).
RESULTS
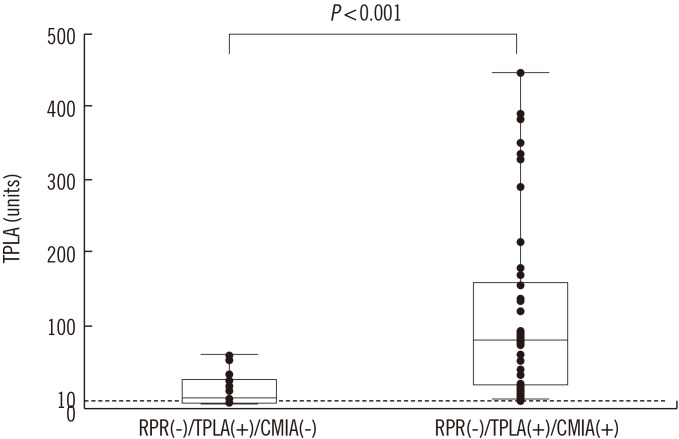
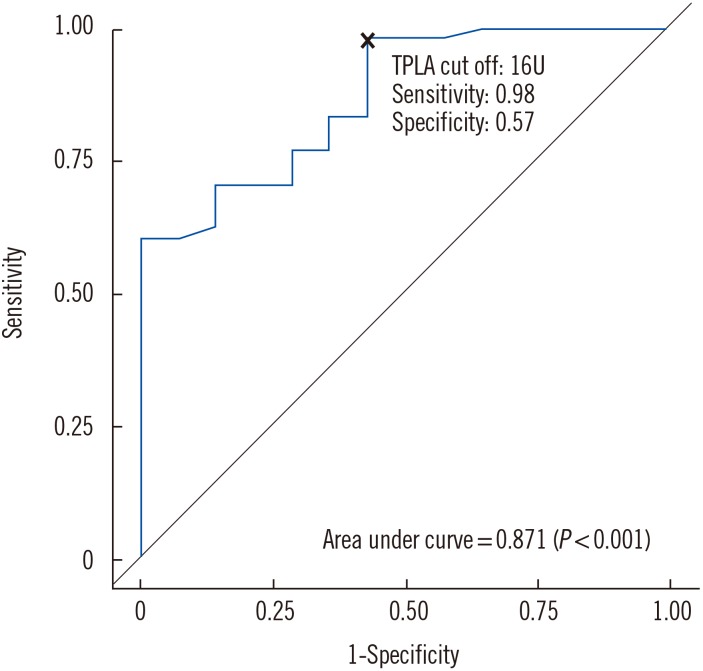
Of the 1,000 specimens tested, 68 (6.8%) were reactive by reverse screening (TPLA) compared with 11 (1.1%) by traditional screening (RPR). The traditional algorithm failed to detect 48 specimens [TPLA(+)/RPR(−)/CMIA(+)]. The median TPLA cutoff index (COI) was higher in CMIA-reactive cases than in CMIA-nonreactive cases (90.5 vs 12.5 U).
CONCLUSIONS
The reverse screening algorithm could detect the subjects with possible latent syphilis who were not detected by the traditional algorithm. Those individuals could be provided with opportunities for evaluating syphilis during their health checkups. The COI values of the initial TPLA test may be helpful in excluding false-positive TPLA test results in the reverse algorithm.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
The Multi-Institutional Health Screening Records Database of South Korea: Description and Evaluation of Its Characteristics
Yunha Noh, Han Eol Jeong, Hye-Jun Kim, Hanju Ko, Eun-Hee Nah, Ju-Young Shin
Yonsei Med J. 2019;60(12):1216-1222. doi: 10.3349/ymj.2019.60.12.1216.
Reference
-
1. Greenblatt RM, Lukehart SA, Plummer FA, Quinn TC, Critchlow CW, Ashley RL, et al. Genital ulceration as a risk factor for human immunodeficiency virus infection. AIDS. 1988; 2:47–50. PMID: 3128996.2. Mehta SD, Ghanem KG, Rompalo AM, Erbelding EJ. HIV seroconversion among public sexually transmitted disease clinic patients: analysis of risks to facilitate early identification. J Acquir Immune Defic Syndr. 2006; 42:116–122. PMID: 16763500.3. Morshed MG. Recent trends in the serologic diagnosis of syphilis. Clin Vaccine Immunol. 2015; 22:137–147. PMID: 25428245.4. Müller I, Brade V, Hagedorn HJ, Straube E, Schörner C, Frosch M, et al. Is serological testing a reliable tool in laboratory diagnosis of syphilis? Meta-analysis of eight external quality control surveys performed by the German infection serology proficiency testing program. J Clin Microbiol. 2006; 44:1335–1341. PMID: 16597859.5. Workowski KA, Berman S. Centers for Disease Control and Prevention (CDC). Sexually transmitted diseases treatment guidelines, 2010. MMWR Recomm Rep. 2010; 59:1–110.6. Loeffelholz MJ. It is time to use treponema-specific antibody screening tests for diagnosis of syphilis. J Clin Microbiol. 2012; 50:2–6. PMID: 22090405.7. Tong ML, Lin LR, Liu LL, Zhang HL, Huang SJ, Chen YY, et al. Analysis of 3 algorithms for syphilis serodiagnosis and implications for clinical management. Clin Infect Dis. 2014; 58:1116–1124. PMID: 24550376.8. Park IU, Chow JM, Bolan G, Stanley M, Shieh J, Schapiro JM. Screening for syphilis with the treponemal immunoassay: analysis of discordant serology results and implications for clinical management. J Infect Dis. 2011; 204:1297–1304. PMID: 21930610.9. Binnicker MJ, Jespersen DJ, Rollins LO. Direct comparison of the traditional and reverse syphilis screening algorithms in a population with a low prevalence of syphilis. J Clin Microbiol. 2012; 50:148–150. PMID: 22090407.10. Owusu-Edusei K Jr, Peterman TA, Ballard RC. Serologic testing for syphilis in the United States: a cost-effectiveness analysis of two screening algorithms. Sex Transm Dis. 2011; 38:1–7. PMID: 20739911.11. Park BG, Yoon JG, Rim JH, Lee A, Kim HS. Comparison of six automated Treponema-Specific antibody assays. J Clin Microbiol. 2016; 54:163–167. PMID: 26560543.12. Centers for Disease Control and Prevention (CDC). Discordant results from reverse sequence syphilis screening-five laboratories, United States, 2006-2010. MMWR Morb Mortal Wkly Rep. 2011; 60:133–137. PMID: 21307823.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Automated Treponemal and Nontreponemal Test Algorithms as First-Line Syphilis Screening Assays
- Comparative Performance of the Reverse Algorithm Using Architect Syphilis TP Versus the Traditional Algorithm Using Rapid Plasma Reagin in Florida's Public Health Testing Population
- Comparison of Auto RPR Plus and Auto TPIM Plus with Mediace RPR and Abbott Syphilis TP for Serologic Diagnosis of Syphilis
- Recent Trends in Clinical Observation of Syphilis and Consideration for Laboratory Tests
- Acquired Secondary Syphilis in Early Childhood