J Breast Cancer.
2010 Sep;13(3):305-310.
Secondary Partial Mastectomy with Contralateral Sentinel Lymph Node Biopsy for Ipsilateral Breast Cancer Recurrence after Conservative Surgery: Report of 2 Cases
- Affiliations
-
- 1Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 2Department of Surgery, Yeungnam University College of Medicine, Daegu, Korea. crystallee@medical.yu.ac.kr
Abstract
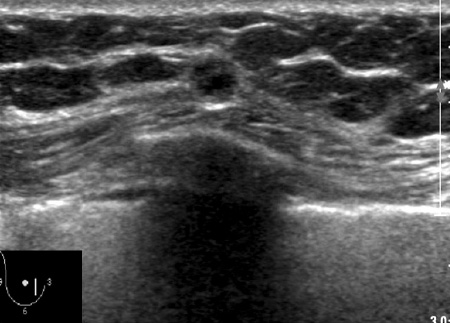
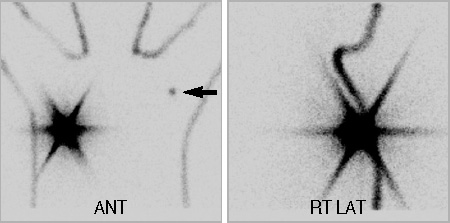
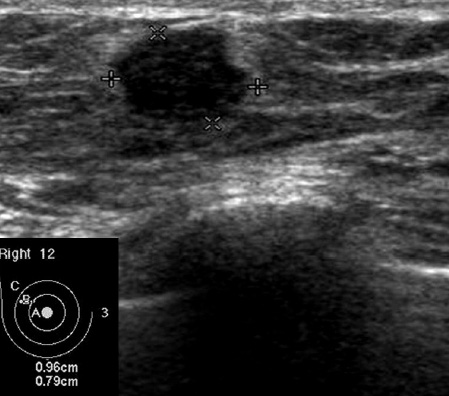
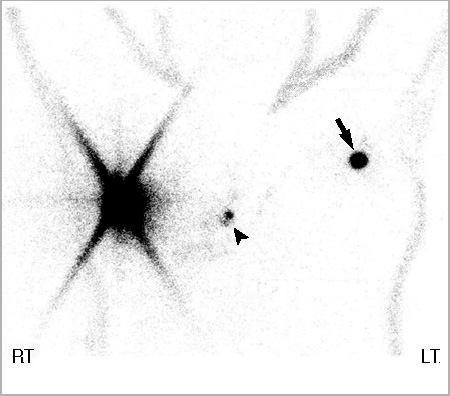
- Mastectomy has been known to be the best strategy for treating in patients with ipsilateral breast cancer recurrence (IBCR) after conservative surgery. For the cases with a small recurrent cancer which is found in the majority of cases on the regular check-up, the patients' desire for breast conserving surgery is increasing. Some recent studies have reported patients with IBCR might receive a second partial mastectomy, when a good local control can be predicted. It is not obvious that sentinel lymph node biopsy (SLNB) in the treated breast is feasible because the previous axillary dissection and/or irradiation may affected the pattern of lymphatic flow. Because of its high accuracy, SLNB may be safely performed for the patients with IBCR in the treated breast. Interestingly, there are reports that SLNB in this condition has revealed that the sentinel lymph node(s) can be found in the opposite side. We reported two cases in which contralateral SLNB were performed during the secondary partial mastectomy for the IBCR after breast conserving surgery.
Keyword
MeSH Terms
Figure
Reference
-
1. Kennedy MJ, Abeloff MD. Management of locally recurrent breast cancer. Cancer. 1993. 71:2395–2409.
Article2. Bethke KP. Breast conservation: predictors and treatment of local recurrence. Semin Surg Oncol. 1996. 12:332–338.
Article3. Gentilini O, Botteri E, Rotmensz N, Santillo B, Peradze N, Saihum RC, et al. When can a second conservative approach be considered for ipsilateral breast tumour recurrence? Ann Oncol. 2007. 18:468–472.
Article4. Kurtz JM, Jacquemier J, Amalric R, Brandone H, Ayme Y, Hans D, et al. Is breast conservation after local recurrence feasible? Eur J Cancer. 1991. 27:240–244.
Article5. Salvadori B, Marubini E, Miceli R, Conti AR, Cusumano F, Andreola S, et al. Reoperation for locally recurrent breast cancer in patients previously treated with conservative surgery. Br J Surg. 1999. 86:84–87.
Article6. Taback B, Nguyen P, Hansen N, Edwards GK, Conway K, Giuliano AE. Sentinel lymph node biopsy for local recurrence of breast cancer after breast-conserving therapy. Ann Surg Oncol. 2006. 13:1099–1104.
Article7. Luini A, Galimberti V, Gatti G, Arnone P, Vento AR, Trifirò G, et al. The sentinel node biopsy after previous breast surgery: preliminary results on 543 patients treated at the European Institute of Oncology. Breast Cancer Res Treat. 2005. 89:159–163.
Article8. Port ER, Fey J, Gemignani ML, Heerdt AS, Montgomery LL, Petrek JA, et al. Reoperative sentinel lymph node biopsy: a new option for patients with primary or locally recurrent breast carcinoma. J Am Coll Surg. 2002. 195:167–172.9. Sood A, Youssef IM, Heiba SI, El-Zeftawy H, Axelrod D, Seigel B, et al. Alternative lymphatic pathway after previous axillary node dissection in recurrent/primary breast cancer. Clin Nucl Med. 2004. 29:698–702.
Article10. Koizumi M, Koyama M, Tada K, Nishimura S, Miyagi Y, Makita M, et al. The feasibility of sentinel node biopsy in the previously treated breast. Eur J Surg Oncol. 2008. 34:365–368.
Article11. Veronesi U, Banfi A, Del Vecchio M, Saccozzi R, Clemente C, Greco M, et al. Comparison of Halsted mastectomy with quadrantectomy, axillary dissection, and radiotherapy in early breast cancer: long-term results. Eur J Cancer Clin Oncol. 1986. 22:1085–1089.
Article12. Veronesi U, Cascinelli N, Mariani L, Greco M, Saccozzi R, Luini A, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 2002. 347:1227–1232.
Article13. Fisher B, Anderson S, Fisher ER, Redmond C, Wickerham DL, Wolmark N, et al. Significance of ipsilateral breast tumour recurrence after lumpectomy. Lancet. 1991. 338:327–331.
Article14. Haffty BG, Reiss M, Beinfield M, Fischer D, Ward B, McKhann C. Ipsilateral breast tumor recurrence as a predictor of distant disease: implications for systemic therapy at the time of local relapse. J Clin Oncol. 1996. 14:52–57.
Article15. Komoike Y, Motomura K, Inaji H, Kasugai T, Koyama H. Repeat lumpectomy for patients with ipsilateral breast tumor recurrence after breast-conserving surgery. Preliminary results. Oncology. 2003. 64:1–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intramammary sentinel lymph node with capsular extravasation in breast cancer
- The Number of Removed Lymph Nodes for an Acceptable False Negative Rate in Sentinel Lymph Node Biopsy for Breast Cancer
- Short Term Follow-up Data in Breast Cancer Patients with Sentinel Lymph Node Biopsy Alone
- Surgical Treatment of Breast Cancer
- Validation and Controversy of Sentinel Node Biopsy for Breast Cancer