J Korean Ophthalmol Soc.
2010 May;51(5):769-773.
Central Toxic Keratopathy After LASEK
- Affiliations
-
- 1Department of Ophthalmology, KyungHee University Medical Center, Seoul, Korea. khjinmd@khmc.or.kr
Abstract
- PURPOSE
We report a case of transient corneal opacity and hyperopia after LASEK surgery.
CASE SUMMARY
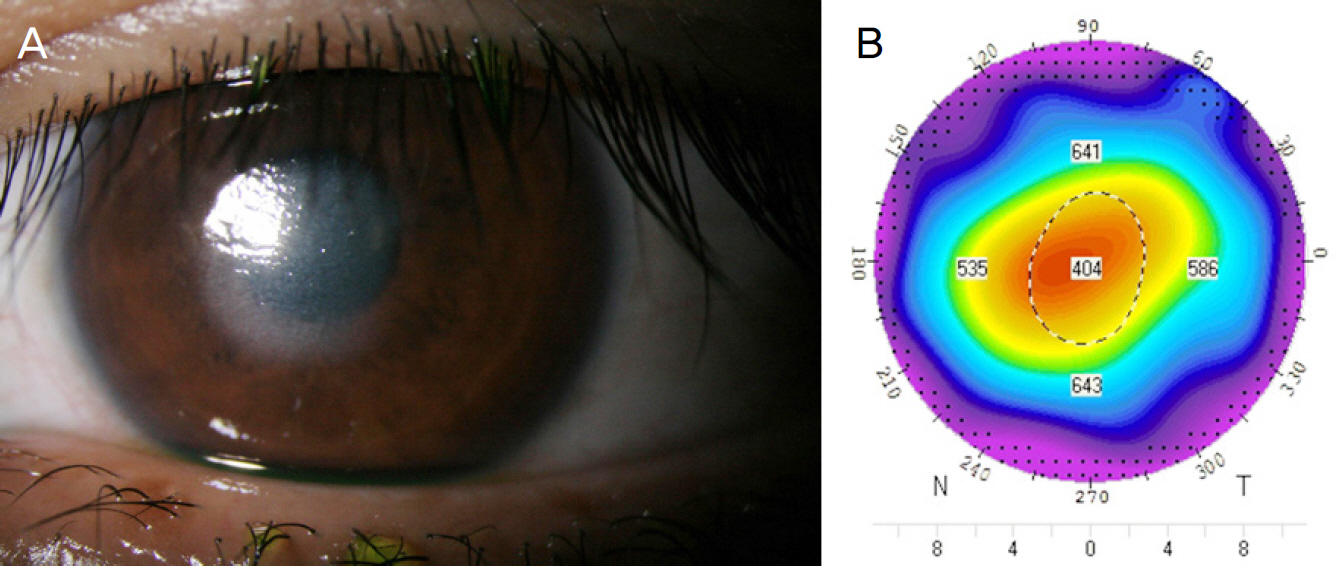
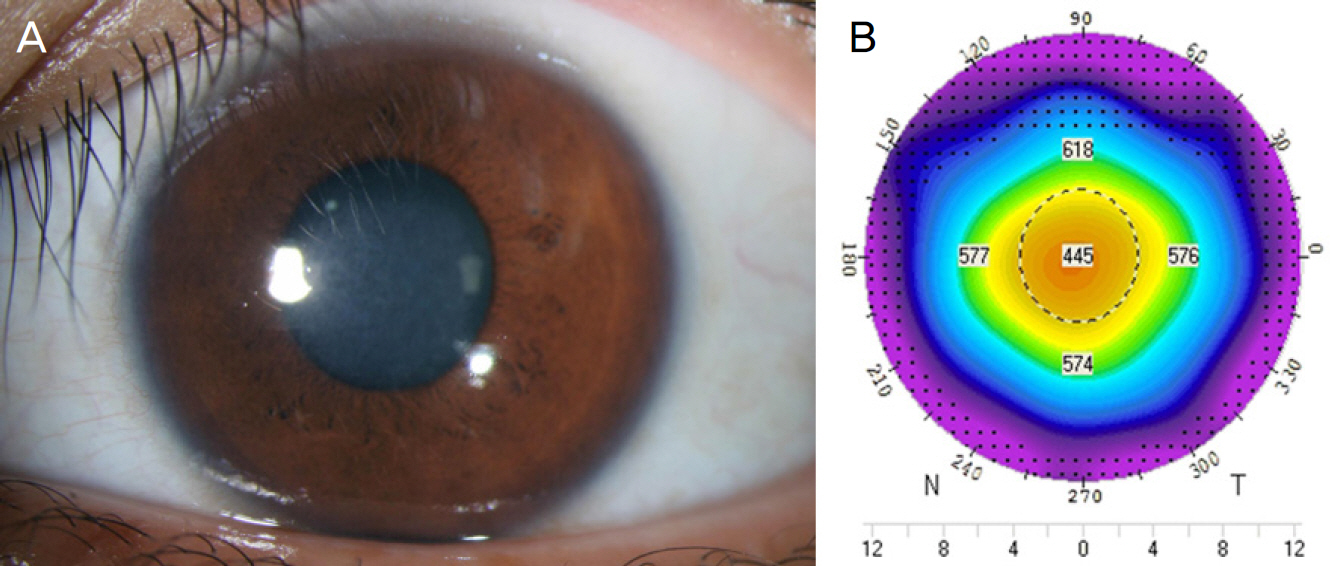
A 21-year-old female visited our clinic complaining of decreased visual acuity in the left eye. The patient had undergone LASEK surgeryten days previously. Before LASEK surgery, the central corneal thickness of the left eye was 540 micrometer, and the refractive error was -2.00 Dsph=-0.75 Dcyl x80A with an estimated ablation depth of 52.2 micrometer. At the time of visit (on the tenth day after surgery), the best corrected visual acuity (BCVA) was 0.07, the central corneal thickness was 404 micrometer, and the refractive error was +1.00D=+1.25D x90. Slit-lamp biomicroscopy showed round central corneal haziness, but there were no signs of inflammation. At the third weeks after surgery, the central corneal thickness was 401 micrometer and the refractive error was +11.25D=-4.00D x145. Slit-lamp biomicroscopy showed sustained round central corneal haze. Twenty-two weeks after surgery, the central corneal thickness was 445 micrometer and the refractive error was -0.75D=-1.25D x180. The corneal opacity had disappeared.
CONCLUSIONS
In case of transient corneal opacity, stromal loss and hyperopic change after LASEK surgery, central toxic keratopathy should be considered.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Melki SA, Azar DT. LASIK Complications: etiology, management, and prevention. Surv Ophthalmol. 2001; 46:95–116.2. Sachdev N, McGhee CN, Craig JP, et al. Epithelial defect, diffuse abdominal keratitis, and epithelial ingrowth following post-LASIK abdominal toxicity. J Cataract Refract Surg. 2002; 28:1463–6.3. Lim GC, Lin HC, Shen SC, Lin KK. Toxic keratopathy-related corneal dehydration after laser in situ keratomileusis. J Cataract Refract Surg. 2005; 31:1656–8.
Article4. Mah FS, Romanowski EG, Dhaliwal DK, et al. Role of topical abdominal on the pathogenesis of diffuse lamellar keratitis in abdominal in vivo studies. J Cataract Refract Surg. 2006; 32:264–8.5. Linebarger EJ, Hardten DR, Lindstrom RL. Diffuse lamellar keratitis: Diagnosis and management. J Cataract Refract Surg. 2000; 26:1072–7.
Article6. Gil-Cazorla R, Teus MA, de Benito-Llopis L, Fuentes I. Incidence of diffuse lamellar keratitis after laser in situ keratomileusis associated with the IntraLase 15 kHz femtosecond laser and Moria M2 microkeratome. J Cataract Refract Surg. 2008; 34:28–31.
Article7. Villarrubia A, Palacín E, Gómez del Río M, Martínez P. Description, etiology, and prevention of an outbreak of diffuse lamellar keratitis abdominal LASIK. J Refract Surg. 2007; 23:482–6.8. Shen YC, Wang CY, Fong SC, et al. Diffuse lamellar keratitis induced by toxic chemicals after laser in situ keratomileusis. J Cataract Refract Surg. 2006; 32:1146–50.
Article9. Brouzas D, Droutsas D, Charakidas A, et al. Severe toxic effect of Methylene blue 1% on iris epithelium and corneal endothelium. Cornea. 2006; 25:470–1.
Article10. Fraenkel GE, Cohen PR, Sutton GL, et al. Central focal interface opacity after laser in situ keratomileusis. J Refract Surg. 1998; 14:571–6.
Article11. Parolini B, Marcon G, Panozzo GA. Central necrotic lamellar abdominal after laser in situ keratomileusis. J Refract Surg. 2001; 17:110–2.12. Sonmez B, Maloney RK. Central Toxic Keratopathy: Description of a syndrome in laser refractive surgery. Am J Ophthalmol. 2007; 143:420–7.
Article13. Fantes FE, Hanna KD, Waring Go 3rd, et al. Wound healing after abdominal laser keratomileusis (photorefractive keratectomy) in monkeys. Arch Ophthalmol. 1990; 108:665–75.14. Smith RJ, Maloney RK. Diffuse lamellar keratitis. A new syndrome in lamellar refractive surgery. Ophthalmology. 1998; 105:1721–6.
Article15. Moon SW, Kim YH, Lee SC, et al. Bilateral peripheral infiltrative abdominal after LASIK. Korean J Ophthalmol. 2007; 21:172–4.16. Choi J, Wee WR, Lee JH, Kim MK. High intraocular pressure-induced delayed diffuse lamellar keratitis after laser in situ abdominal(LASIK). J Korean Ophthalmol Soc. 2006; 47:1678–85.17. Ku M, Shyn KH. 2006 survey for KSCRS members – Current trends in refractive surgery in Korea. J Korean Ophthalmol Soc. 2009; 50:182–8.18. Kim SJ, Lee MH, Kim EH, Lee JS. Corneal opacity caused by LASEK with improper high-concentrated Mitomycin-C. J Korean Ophthalmol Soc. 2008; 49:1525–31.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum: Central Toxic Keratopathy after LASEK [J Korean Ophthalmol Soc 2010;51(5):769-773, DOI:10.3341/jkos.2010.51.5.769]
- Central Toxic Keratopathy after Femtosecond Laser in-situ Keratomileusis
- Influence of Central Corneal Thickness Change on Intraocular Pressure Measurement after LASIK and LASEK
- Long-term Outcome of Combined Laser-assisted Subepithelial Keratomileusis and Accelerated Corneal Crosslinking for Myopia
- Changes in the Cornea and Anterior Chamber After LASEK: Pentacam Findings