J Korean Ophthalmol Soc.
2010 May;51(5):642-650.
Clinical Research on Surgical Treatment for Double-Head Pterygium
- Affiliations
-
- 1Cheil Eye Hospital, Daegu, Korea. eyepark9@dreamwiz.com
Abstract
- PURPOSE
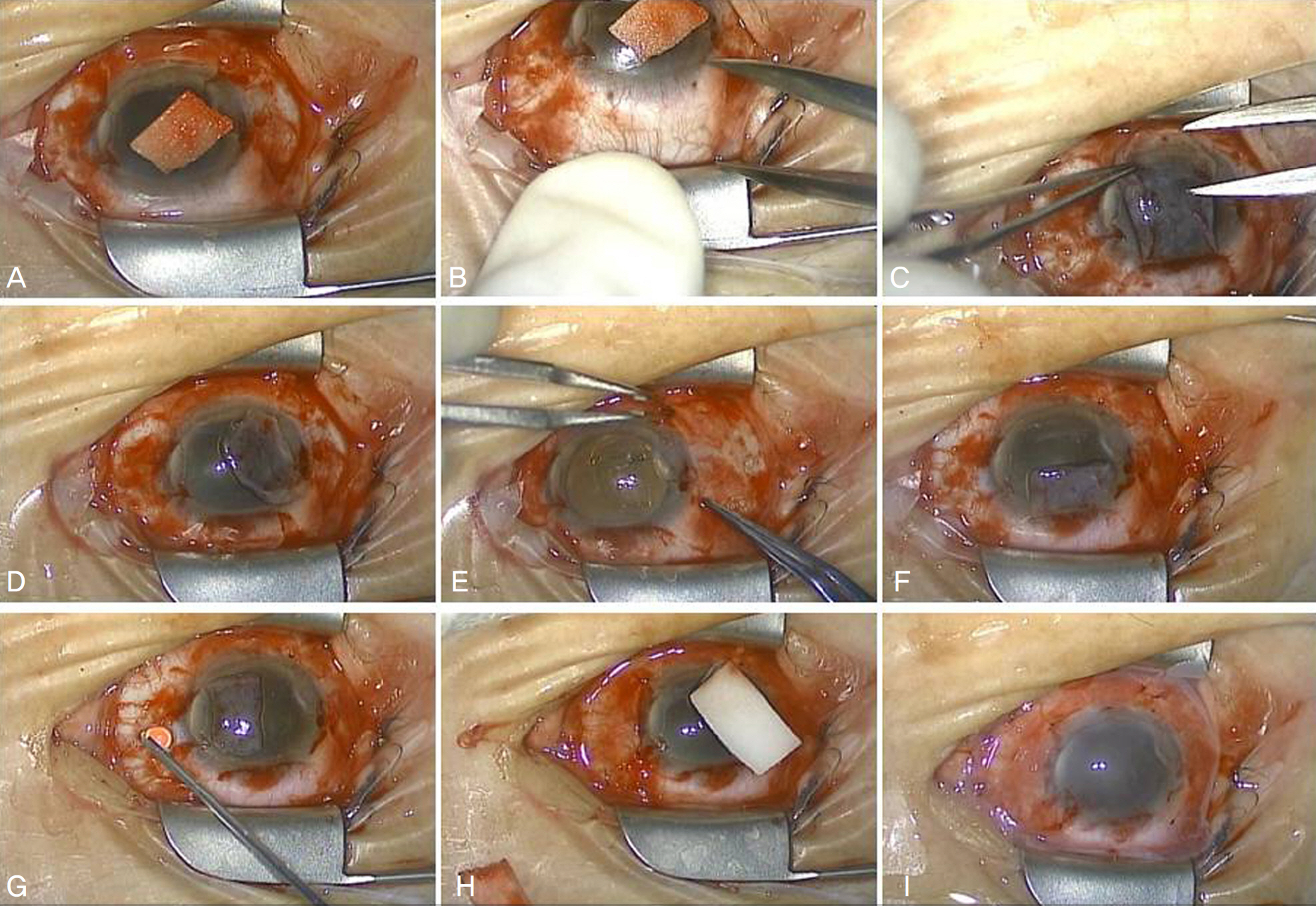
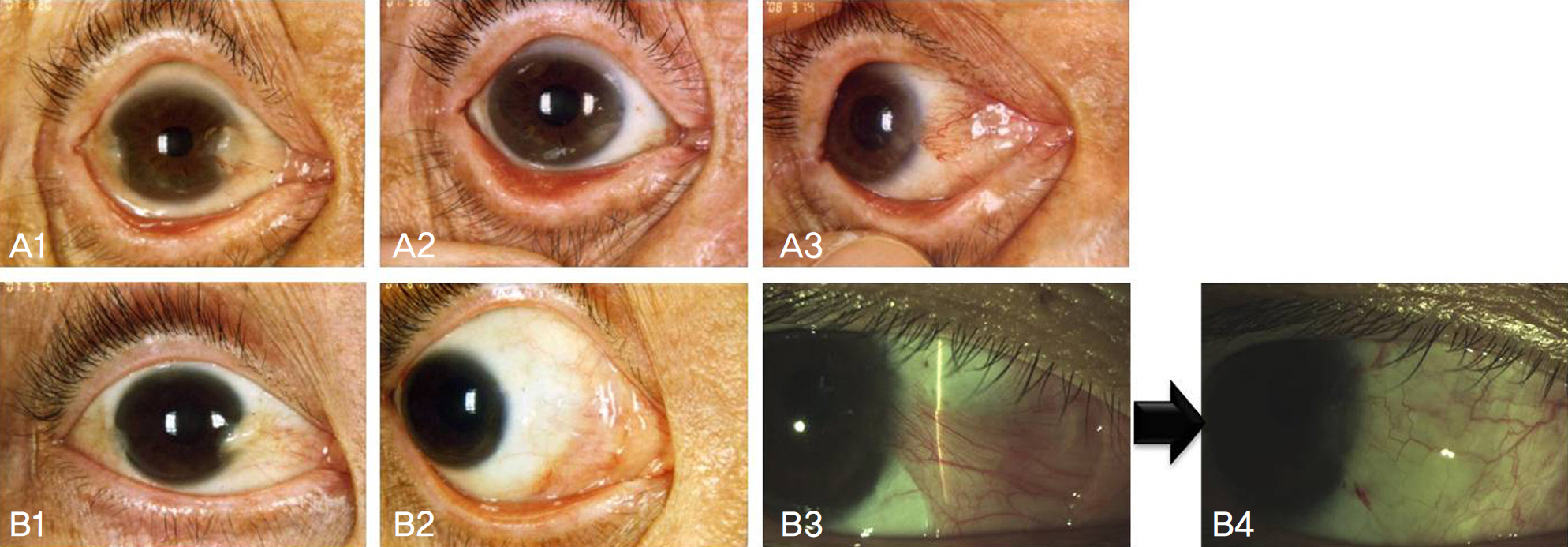
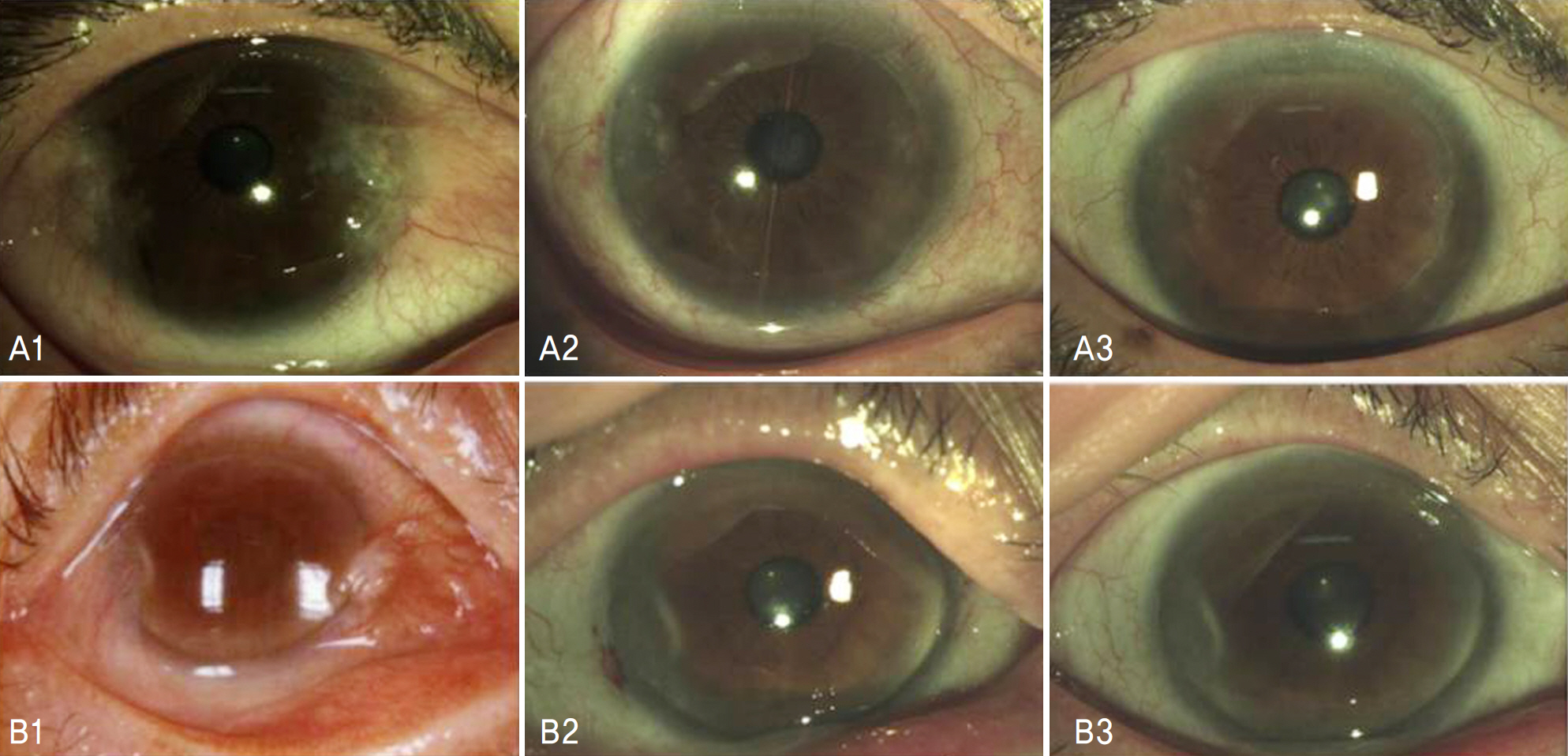
To evaluate two surgical methods-amniotic membrane transplantation (AMT) and split-conjunctival grafts (SCG)-for double-head pterygium, with regard to the postoperative outcome and recurrence rate.
METHODS
In a total of 16 eyes (14 patients), 7 eyes (6 patients) receiving amniotic membrane transplantation and 9 eyes (8 patients) receiving split-conjunctival grafts were compared to evaluate recurrence and complications.
RESULTS
Within the amniotic membrane transplantation group, two eyes (29%) had corneal recurrence, and 3 eyes (43%) had conjunctival recurrence. The mean follow-up period was 21.9+/-3.5 months, and all recurrences were on the nasal side. The average period preceding the corneal recurrences was 7.2+/-1.8 months. Within the split-conjunctival grafts group, the mean follow-up was 13.6+/-2.1 months, and neither the corneal nor conjunctival recurrences were observed. In addition, the eyes of this group were more aesthetically stable, with only one eye exhibiting pseudo-pterygium at the donor site.
CONCLUSIONS
In cases of double-head pterygium without contraindication of conjunctival autograft, the split-conjunctival grafts produced fewer recurrences and showed enhanced cosmetic results, as compared to the amniotic membrane transplantation, indicating that the split-conjunctival grafts is the superior choice over amniotic membrane transplantation.
MeSH Terms
Figure
Reference
-
References
1. Kenyon KR, Wagoner MD, Hettinger ME. Conjunctival autograft transplantation for advanced and recurrent pterygium. Ophthalmology. 1985; 92:1461–70.
Article2. Prabhasawat P, Barton K, Burkett G, Tseng SC. Comparison of abdominal autografts, amniotic membrane grafts, and primary closure for pterygium excision. Ophthalmology. 1997; 104:974–85.3. Sanchez-Thorin JC, Rocha G, Yelin JB. Meta-analysis on the abdominal rates after bare sclera resection with and without mitomycin C use and conjunctival autograft placement in surgery for primary pterygium. Br J Ophthalmol. 1998; 82:661–5.4. Ma DH, See LC, Liau SB, Tsai RJ. Aminotic membrane graft for abdominal pterygium: comparision with conjunctival autograft and topical mitomycin C treatment. Br J Ophthalmol. 2000; 84:973–8.5. Hirst LW. Prospective study of primary pterygium surgery using pterygium extended removal followed by extended conjunctival transplantation. Ophthalmology. 2008; 115:1663–72.
Article6. Solomon A, Pires RT, Tseng SC, et al. Amniotic membrane abdominal after extensive removal of primary and recurrent pterygia. Ophthalmology. 2001; 108:449–60.7. Avisar R, Snir M, Weinberger D. Outcome of double-head pterygium surgery. Cornea. 2003; 22:501–3.8. Maheshwari S. Split-conjunctival grafts for double-head pterygium. Indian J Ophthalmol. 2005; 53:53–5.9. Wu WK, Wong VW, Chi SC, Lam DS. Surgical management of dou-ble-head pterygium by using a novel technique: conjunctival rotational autograft combined with conjunctival autograft. Cornea. 2007; 26:1056–9.10. Rubinfeld RS, Pfister RR, Stein RM, et al. Serious complications of topical mitomycin C after pterygium surgery. Ophthalmology. 1992; 99:1647–54.11. Safianik B, Ben-Zion I, Garzozi HJ. Serious corneoscleral complications after pterygium excision with mitomycin C. Br J Ophthalmol. 2002; 86:357–8.
Article12. Ti SE, Tan DT. Tectonic corneal lamellar grafting for severe scleral melting after pterygium surgery. Ophthalmology. 2003; 110:1126–36.
Article13. Wan Norliza WM, Raihan IS, Azwa JA, Ibrahim M. Scleral melting 16 years after pterygium excision with topical Mitomycin C adjuvant therapy. Cont Lens Anterior Eye. 2006; 29:165–7.
Article14. Jang JH, Choi TH. The effect of amniotic membrane transplantation for pterygium excision. J Korean Ophthalmol Soc. 2005; 46:597–604.15. Katircioglu YA, Altiparmak UE, Duman S. Comparison of three methods for the treatment of pterygium: amniotic membrane graft, conjunctival autograft and conjunctival autograft plus mitomycin C. Orbit. 2007; 26:5–13.
Article16. Kim YI, Paek KU, Park HS. Ocular surface reconstruction with abdominal membrane transplantation in pterygium. J Korean Ophthalmol Soc. 1999; 40:1178–83.17. Kim MJ, Tchah HW. Treatment of pterygium with amniotic abdominal transplantation. J Korean Ophthalmol Soc. 1998; 39:59–64.18. Tananuvat N, Martin T. The results of amniotic membrane transplantation for primary pterygium compared with conjunctival autograft. Cornea. 2004; 23:458–63.
Article19. Hirst LW. The treatment of pterygium. Surv Ophthalmol. 2003; 48:145–80.
Article20. John T. Pterygium excision and conjunctival mini-autograft: Preliminary report. Eye. 2001; 15:292–6.
Article21. Dupps WJ Jr, Jeng BH, Meisler DM. Narrow-strip conjunctival abdominal for treatment of pterygium. Ophthalmology. 2007; 114:227–31.22. Coroneo MT, Di Girolam N, Wakefield D. The pathogenesis of pterygia. Curr Opin Ophthalmol. 1999; 10:282–8.
Article23. Yoon KC, Heo H, Jeong IY, Park YG. The use of fibrin glue for abdominal autotransplantation in pterygium. J Korean Ophthalmol Soc. 2006; 47:198–204.24. Koranyi G, Seregard S, Kopp ED. Cut and paste: a no suture, small abdominal approach to pterygium surgery. Br J Ophthalmol. 2004; 88:911–4.26. Kim HH, Mun HJ, Park YJ, et al. Conjunctivolimbal autograft using a fibrin adhesive in pterygium surgery. Korean J Ophthalmol. 2008; 22:147–54.
Article27. Dolezalova V. Is the occurrence of a temporal pterygium really so rare? Ophthalmologica. 1977; 174:88–91.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Simplified way to Remove the Head of Pterygium
- A Clinical Observation on the Argon Laser Effect of the Pterygium
- The Historical Observation of the Pterygium Surgery
- On the New Surgical Treatment of Pterygium
- Use of Immunosuppressant in the Treatment of Surgically Induced Necrotizing Scleritis (SINS) after Pterygium Excision