Korean J Radiol.
2018 Dec;19(6):1066-1076. 10.3348/kjr.2018.19.6.1066.
Optimal Phase of Dynamic Computed Tomography for Reliable Size Measurement of Metastatic Neuroendocrine Tumors of the Liver: Comparison between Pre- and Post-Contrast Phases
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul 05505, Korea. medimash@gmail.com
- 2Department of Radiology, Ajou University School of Medicine and Graduate School of Medicine, Ajou University Hospital, Suwon 16499, Korea.
- 3Department of Radiology, University of Ulsan College of Medicine, Ulsan University Hospital, Ulsan 44033, Korea.
- 4Department of Imaging, Dana-Farber Cancer Institute, Brigham and Women's Hospital, Harvard Medical School, Boston, MA 02215, USA.
- 5Department of Radiology, University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH 44106, USA.
- KMID: 2424846
- DOI: http://doi.org/10.3348/kjr.2018.19.6.1066
Abstract
OBJECTIVE
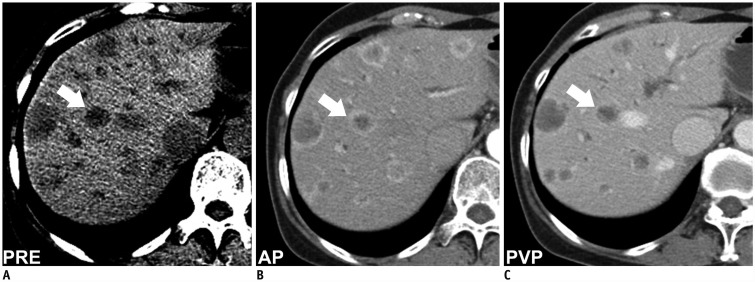
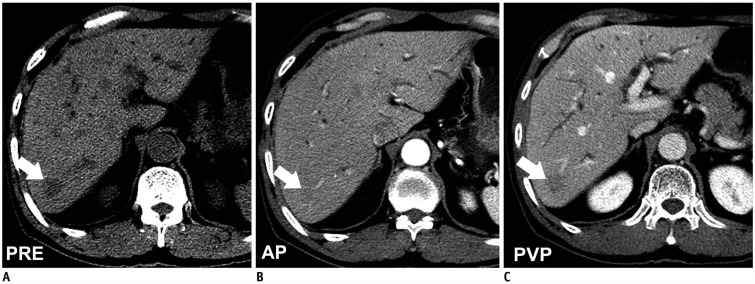
The reliability of size measurements of liver metastases from neuroendocrine tumors (NETs) on contrast-enhanced computed tomography (CT) phases made by different readers may be hampered due to transient, variable rim enhancement in arterial phase (AP) or portal venous phase (PVP) images. We aimed to assess the reliability of tumor size measurements in pre- and post-contrast scans.
MATERIALS AND METHODS
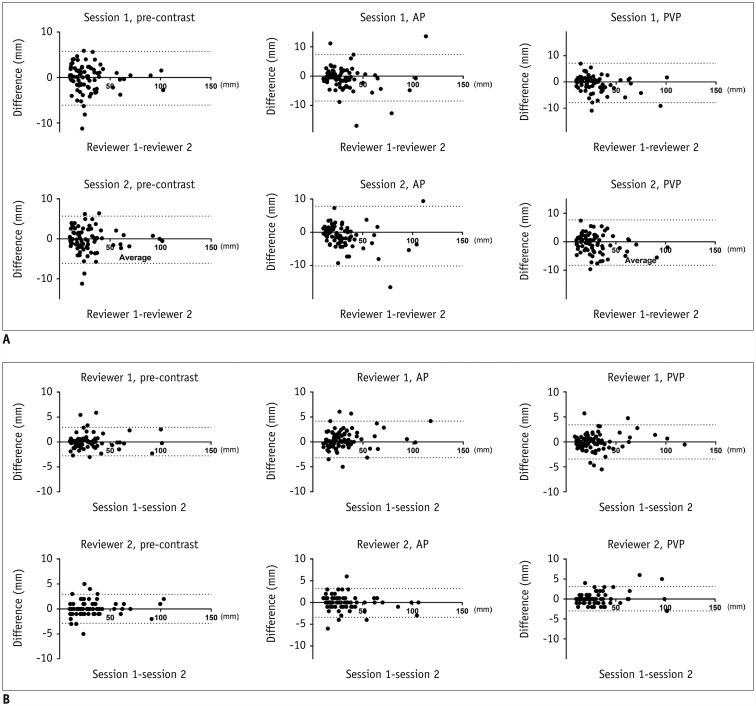
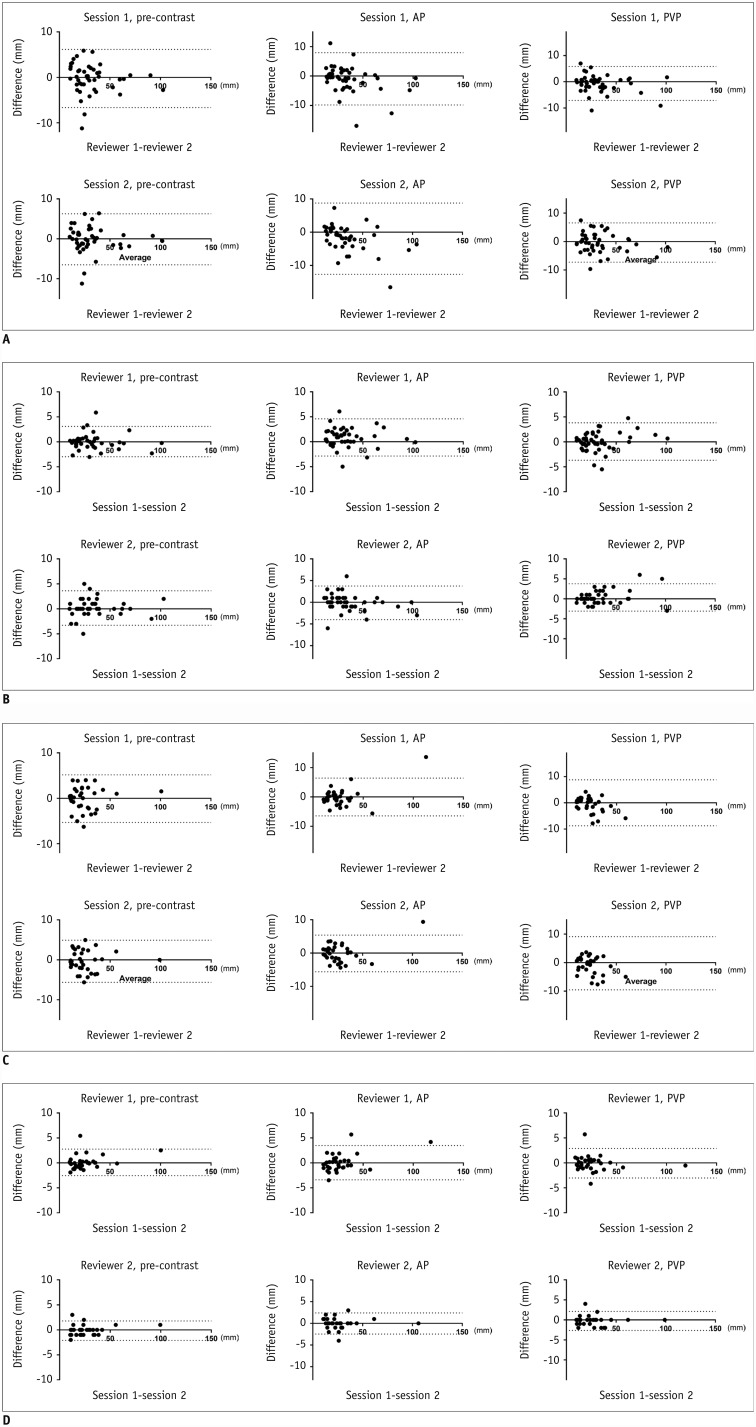
The study coordinator selected target lesions according to Response Evaluation Criteria in Solid Tumors 1.1 guidelines in 44 consecutive patients with pathologically confirmed NET liver metastases. Two blinded readers measured the longest diameters of target lesions on pre-contrast, AP, and PVP images twice with a 4-week interval. Inter- and intra-observer agreements were evaluated using Bland-Altman plots and 95% limit of agreement (LOA) calculations.
RESULTS
Of the 79 target lesions (approximate mean size of 3 cm), 45 showed rim enhancement. Inter-observer agreement assessed based on LOA was highest in pre-contrast CT images (−6.1-5.7 mm), followed by PVP (−7.9-7.1 mm) and AP (−8.5-7.4 mm) images. Intra-observer agreement showed the same trend: −2.8-2.9 mm and −2.9-2.9 mm for readers 1 and 2, respectively, on pre-contrast CT, −2.8-2.9 mm and −3.0-3.2 mm, respectively, on PVP, and −3.2-4.2 mm and −3.4-3.2 mm, respectively, on AP images. Mean tumor diameters differed significantly among the phases in the following increasing order: pre-contrast CT, PVP, and AP images.
CONCLUSION
There was better inter- and intra-observer agreement in size measurements of NET liver metastases on precontrast scans than on AP and PVP scans. Pre-contrast CT may be the optimal for measuring NET liver metastases if its accuracy is proven.
Keyword
MeSH Terms
Figure
Reference
-
1. Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000; 92:205–216. PMID: 10655437.2. Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009; 45:228–247. PMID: 19097774.
Article3. Thiesse P, Ollivier L, Di Stefano-Louineau D, Négrier S, Savary J, Pignard K, et al. Response rate accuracy in oncology trials: reasons for interobserver variability. Groupe Français d'Immunothérapie of the Fédération Nationale des Centres de Lutte Contre le Cancer. J Clin Oncol. 1997; 15:3507–3514. PMID: 9396404.
Article4. Luersen GF, Wei W, Tamm EP, Bhosale PR, Szklaruk J. Evaluation of magnetic resonance (MR) biomarkers for assessment of response with response evaluation criteria in solid tumors: comparison of the measurements of neuroendocrine tumor liver metastases (NETLM) with various MR sequences and at multiple phases of contrast administration. J Comput Assist Tomogr. 2016; 40:717–722. PMID: 27636124.5. Patten RM, Byun JY, Freeny PC. CT of hypervascular hepatic tumors: are unenhanced scans necessary for diagnosis? AJR Am J Roentgenol. 1993; 161:979–984. PMID: 8273641.
Article6. Soyer P, Gueye C, Somveille E, Laissy JP, Scherrer A. MR diagnosis of hepatic metastases from neuroendocrine tumors versus hemangiomas: relative merits of dynamic gadolinium chelate-enhanced gradient-recalled echo and unenhanced spin-echo images. AJR Am J Roentgenol. 1995; 165:1407–1413. PMID: 7484575.
Article7. Soyer P, Tidjani K, Laissy JP, Sibert A, Menu Y. Dynamic Gd-DOTA-enhanced MR imaging of hepatic metastases from pancreatic neuroendocrine tumors. Eur J Radiol. 1994; 18:180–184. PMID: 7957287.
Article8. Chalian H, Töre HG, Horowitz JM, Salem R, Miller FH, Yaghmai V. Radiologic assessment of response to therapy: comparisonof RECIST Versions 1.1 and 1.0. Radiographics. 2011; 31:2093–2105. PMID: 22084190.9. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Iniciativa STROBE. [The Strengthening the Reporting of Observational Studies in Epidemiology [STROBE] statement: guidelines for reporting observational studies]. Gac Sanit. 2008; 22:144–150. PMID: 18420014.
Article10. Sprawls P. AAPM tutorial. CT image detail and noise. Radiographics. 1992; 12:1041–1046. PMID: 1529128.
Article11. Ha HI, Hong SS, Kim MJ, Lee K. 100 kVp low-tube voltage abdominal CT in adults: radiation dose reduction and image quality comparison of 120 kVp abdominal CT. J Korean Soc Radiol. 2016; 75:285–295.
Article12. Krajewski KM, Nishino M, Franchetti Y, Ramaiya NH, Van den Abbeele AD, Choueiri TK. Intraobserver and interobserver variability in computed tomography size and attenuation measurements in patients with renal cell carcinoma receiving antiangiogenic therapy: implications for alternative response criteria. Cancer. 2014; 120:711–721. PMID: 24264883.
Article13. Raunig DL, McShane LM, Pennello G, Gatsonis C, Carson PL, Voyvodic JT, et al. QIBA Technical Performance Working Group. Quantitative imaging biomarkers: a review of statistical methods for technical performance assessment. Stat Methods Med Res. 2015; 24:27–67. PMID: 24919831.
Article14. Barnhart HX, Barboriak DP. Applications of the repeatability of quantitative imaging biomarkers: a review of statistical analysis of repeat data sets. Transl Oncol. 2009; 2:231–235. PMID: 19956383.
Article15. Park JE, Han K, Sung YS, Chung MS, Koo HJ, Yoon HM, et al. Selection and reporting of statistical methods to assess reliability of a diagnostic test: conformity to recommended methods in a peer-reviewed journal. Korean J Radiol. 2017; 18:888–897. PMID: 29089821.
Article16. Jee HB, Park MJ, Lee HS, Park MS, Kim MJ, Chung YE. Is non-contrast CT adequate for the evaluation of hepatic metastasis in patients who cannot receive iodinated contrast media? PLoS One. 2015; 10:e0134133. PMID: 26218533.
Article17. van Persijn van Meerten EL, Gelderblom H, Bloem JL. RECIST revised: implications for the radiologist. A review article on the modified RECIST guideline. Eur Radiol. 2010; 20:1456–1467. PMID: 20033179.
Article18. Sahu S, Schernthaner R, Ardon R, Chapiro J, Zhao Y, Sohn JH, et al. Imaging biomarkers of tumor response in neuroendocrine liver metastases treated with transarterial chemoembolization: can enhancing tumor burden of the whole liver help predict patient survival? Radiology. 2017; 283:883–894. PMID: 27831830.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Enhancenent Patterns and Detection Rate of IV etastatic Adenocarcinoma of the Liver in Early and Late Phase of Spiral CT
- Spiral CT for the Measurement of Hepatic Metastatic Mass from Gastrointestinal Malignant Tumor: Relative Value of Arterial, Portal and Delayed Phase Scanning
- Spiral CT for the Detection of Metastatic Tumor of the Liver: Relative Value of Arterial, Portal Venous and Delayed Phase Scanning
- Hepatic Masses: Differential Diagnosis with Two Phases Imaging by Using Spiral CT
- Contrast Enhancement Characteristics of Hepatocellular Carcinoma on Two-Phase Dynamic Scan with Spiral CT