Korean J Neurotrauma.
2018 Oct;14(2):159-163. 10.13004/kjnt.2018.14.2.159.
A Case of Posterior Inferior Cerebellar Artery Infarction after Cervical Chiropractic Manipulation
- Affiliations
-
- 1Department of Neurosurgery, Ewha Womans University Mokdong Hospital, Ewha Womans University College of Medicine, Seoul, Korea. nshsg@ewha.ac.kr
- KMID: 2424332
- DOI: http://doi.org/10.13004/kjnt.2018.14.2.159
Abstract
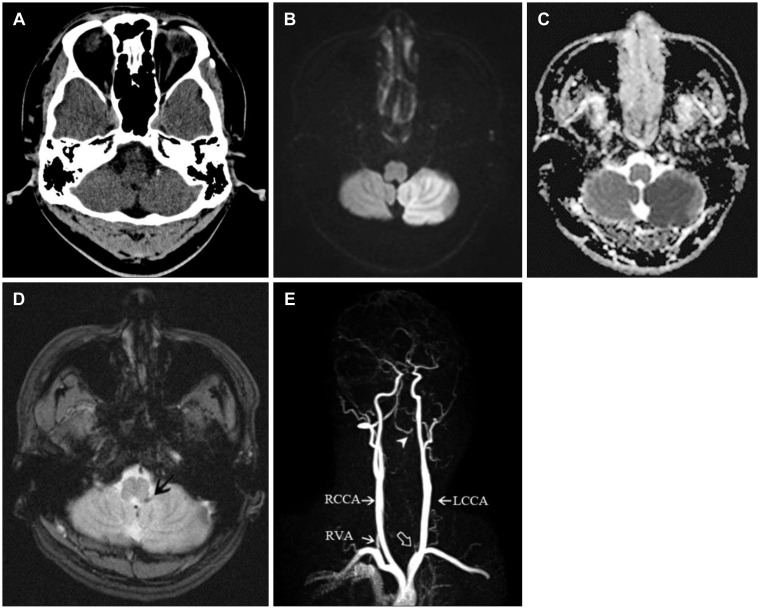
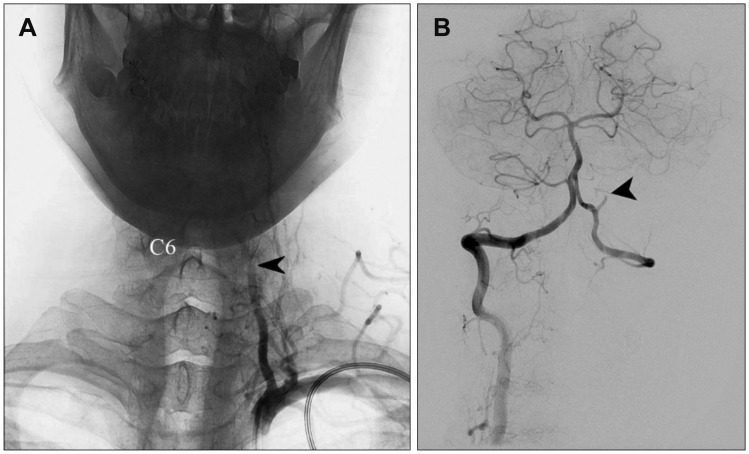
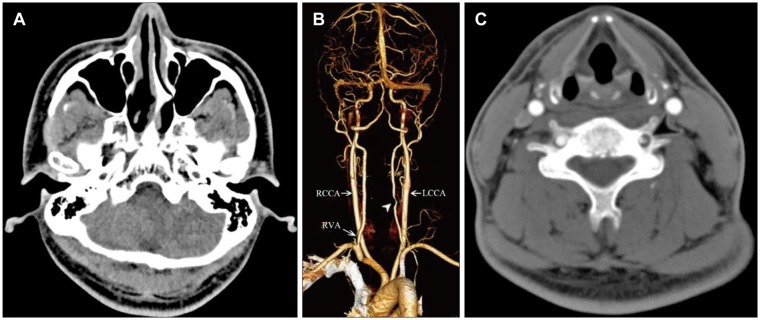
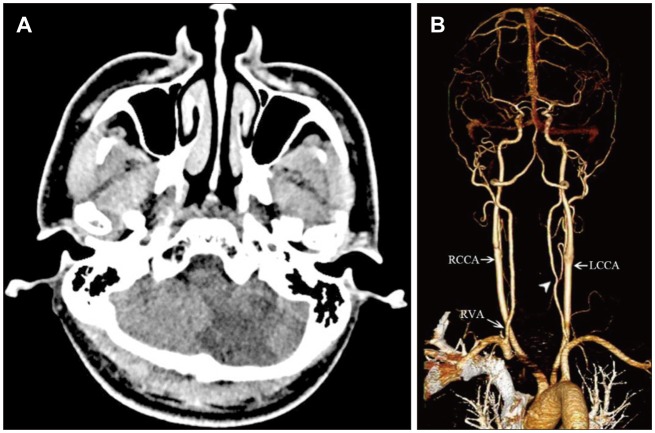
- We describe the case of a patient who had infarction of the posterior inferior cerebellar artery (PICA) after a chiropractic cervical manipulation. A 39-year-old man visited the emergency room with signs of cerebellar dysfunction, presenting with a 6-hour history of vertigo and imbalance. Two weeks ago, he was treated by a chiropractor for intermittent neck pain. At the time of admission, brain computed tomography, magnetic resonance imaging, and angiography revealed an acute infarction in the left PICA territory and occlusion of the extracranial vertebral artery (VA; V1/2 junction) as a result of the dissection of the VA. Angiography revealed complete occlusion of the left PICA and arterial dissection was shown in the extracranial portion of the VA. He was treated with antiplatelet therapy. Three weeks later, he was discharged without any sequelae. The possibility of VA dissection should be considered at least once in patients presenting with cerebellar dysfunctions with a recent history of chiropractic cervical manipulation.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Letter to the Editor: A Case of Posterior Inferior Cerebellar Artery Infarction after Cervical Chiropractic Manipulation (
Korean J Neurotrauma 2018;14:159–163)
Stephen Marc Perle, HanSuk Jung, JooHyun Ham, HwanTak Choi
Korean J Neurotrauma. 2019;15(1):72-73. doi: 10.13004/kjnt.2019.15.e5.
Reference
-
1. Albuquerque FC, Hu YC, Dashti SR, Abla AA, Clark JC, Alkire B, et al. Craniocervical arterial dissections as sequelae of chiropractic manipulation: patterns of injury and management. J Neurosurg. 2011; 115:1197–1205. PMID: 21923248.
Article2. Chen WL, Chern CH, Wu YL, Lee CH. Vertebral artery dissection and cerebellar infarction following chiropractic manipulation. Emerg Med J. 2006; 23:e1. PMID: 16373786.
Article3. Cho IY, Hwang SK. A case of lateral medullary infarction after endovascular trapping of the vertebral artery dissecting aneurysm. J Korean Neurosurg Soc. 2012; 51:160–163. PMID: 22639714.
Article4. Hutchinson PJ, Pickard JD, Higgins JN. Neurological picture. Vertebral artery dissection presenting as cerebellar infarction. J Neurol Neurosurg Psychiatry. 2000; 68:98–99. PMID: 10601413.5. Liu D. Cervical manipulation leading to dissection was not performed by a chiropractor. Emerg Med J. 2007; 24:146.6. Menéndez-González M, García C, Suárez E, Fernández-Díaz D, Blázquez-Menes B. Wallenberg's syndrome secondary to dissection of the vertebral artery caused by chiropractic manipulation. Rev Neurol. 2003; 37:837–839. PMID: 14606051.7. Ramphul N, Geary U. Caveats in the management and diagnosis of cerebellar infarct and vertebral artery dissection. Emerg Med J. 2009; 26:303–304. PMID: 19307404.
Article8. Rothwell DM, Bondy SJ, Williams JI. Chiropractic manipulation and stroke: a population-based case-control study. Stroke. 2001; 32:1054–1060. PMID: 11340209.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Letter to the Editor: A Case of Posterior Inferior Cerebellar Artery Infarction after Cervical Chiropractic Manipulation (Korean J Neurotrauma 2018;14:159–163)
- Authors' Reply to Letter to the Editor: A Case of Posterior Inferior Cerebellar Artery Infarction after Cervical Chiropractic Manipulation (Korean J Neurotrauma 2018;14:159–163)
- Three cases of posterior circulation infarction related with cervical manipulation or trauma
- Cervical Spinal Cord Infarction Presenting as Chest Pain in Patients with Acute Cerebellar Infarction
- A Case of Central Retinal Artery Occlusion after Chiropractic Manipulation of the Neck