Hip Pelvis.
2017 Jun;29(2):91-96. 10.5371/hp.2017.29.2.91.
Measuring the Impact of Femoral Head Size on Dislocation Rates Following Total Hip Arthroplasty
- Affiliations
-
- 1Department of Orthopaedic Surgery, Kwangju Christian Hospital, Gwangju, Korea. paedic@chol.com
- KMID: 2424236
- DOI: http://doi.org/10.5371/hp.2017.29.2.91
Abstract
- PURPOSE
The purpose of this study was to evaluate if the femoral head's size has an impact on dislocation rates following total hip arthroplasty (THA).
MATERIALS AND METHODS
Five hundreds forty-three THA performed using a posterolateral approach in our hospital and followed up more than 6 months were included in this study. We evaluated dislocation rates based on the size of femoral head (28 mm vs. over 32 mm) and further investigated the dislocation rates classified into primary and revision surgery. Patient-related and surgical factors were reviewed to evaluate risk factors impacting dislocation rates.
RESULTS
Dislocation occurred in 9.6% of cases (n=52; 32 males and 20 females). Of this dislocation group, 36 were treated with femoral heads 28 mm in diameter (9.8% of all patients treated with 28 mm femoral heads) and 16 were treated with femoral heads 32 mm and over (9.1% of all patients treated with femoral heads of at least 32 mm). The percentages of patients experiencing dislocation were not significantly different among the two groups (i.e., 28 mm vs. ≥32 mm). However, after revision surgery, the dislocation rate in the 28-mm group was significantly higher than the ≥32-mm group (P<0.05). In a case-control study comparing dislocation and non-dislocation groups, the risk of dislocation was 6 times higher in patients with habitual alcohol intake, and 9.2 times higher in patients with a neuropsychiatric disorder (P<0.05).
CONCLUSION
Patient factors are considered to have a more significant impact on dislocation rates following THA than the size of femoral head.
MeSH Terms
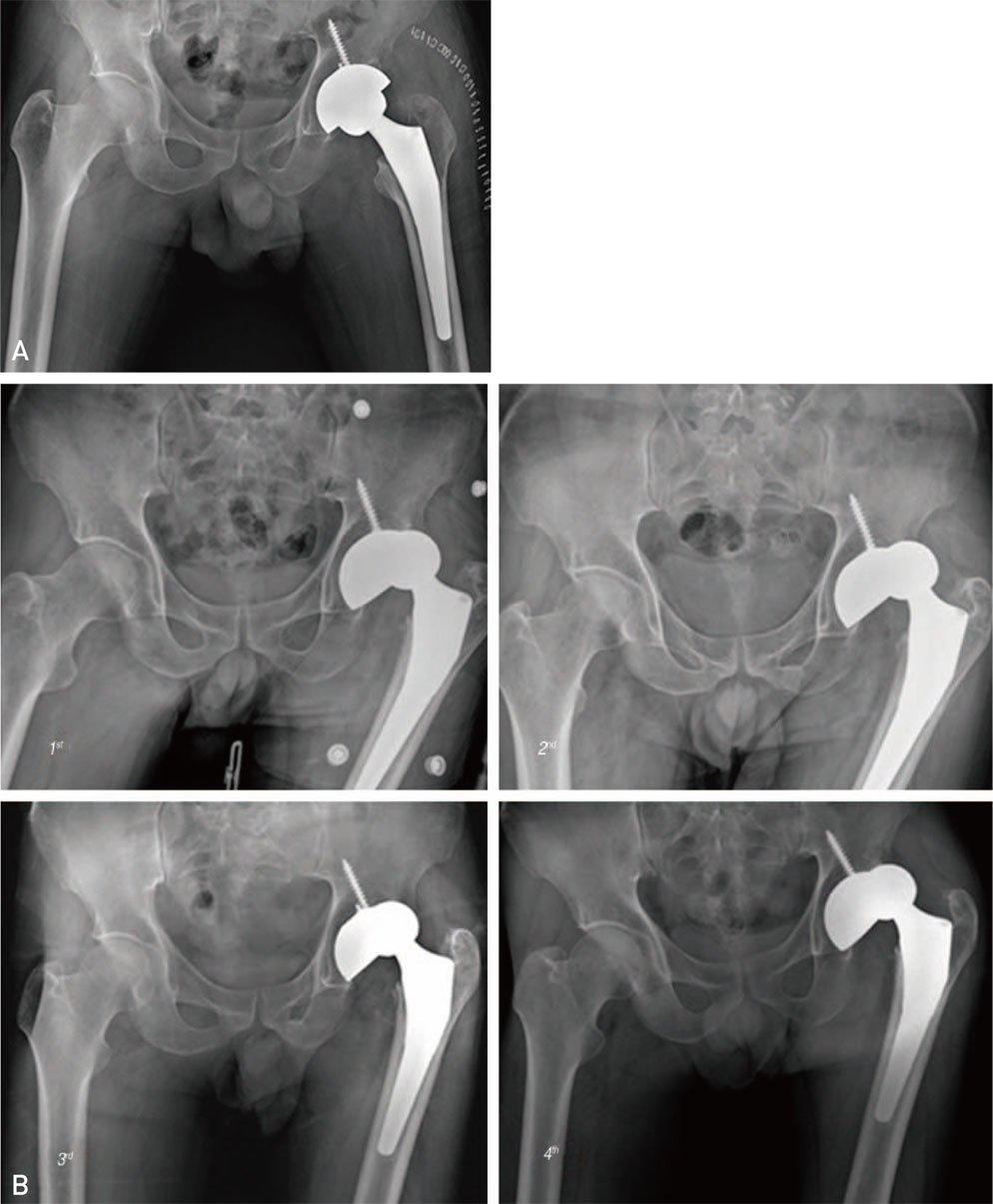
Figure
Reference
-
1. Woo RY, Morrey BF. Dislocations after total hip arthroplasty. J Bone Joint Surg Am. 1982; 64:1295–1306.
Article2. Ali Khan MA, Brakenbury PH, Reynolds IS. Dislocation following total hip replacement. J Bone Joint Surg Br. 1981; 63-B:214–218.
Article3. Fackler CD, Poss R. Dislocation in total hip arthroplasties. Clin Orthop Relat Res. 1980; (151):169–178.
Article4. Berry DJ. Unstable total hip arthroplasty: detailed overview. Instr Course Lect. 2001; 50:265–274.5. Carlsson AS, Gentz CF. Postoperative dislocation in the Charnley and Brunswik total hip arthroplasty. Clin Orthop Relat Res. 1977; (125):177–182.
Article6. Eftekhar NS. Dislocation and instability complicating low friction arthroplasty of the hip joint. Clin Orthop Relat Res. 1976; (121):120–125.
Article7. Ekelund A, Rydell N, Nilsson OS. Total hip arthroplasty in patients 80 years of age and older. Clin Orthop Relat Res. 1992; (281):101–106.
Article8. Etienne A, Cupic Z, Charnley J. Postoperative dislocation after Charnley low-friction arthroplasty. Clin Orthop Relat Res. 1978; (132):19–23.
Article9. Turner RS. Postoperative total hip prosthetic femoral head dislocations. Incidence, etiologic factors, and management. Clin Orthop Relat Res. 1994; (301):196–204.
Article10. Cuckler JM, Moore KD, Lombardi AV Jr, McPherson E, Emerson R. Large versus small femoral heads in metal-on-metal total hip arthroplasty. J Arthroplasty. 2004; 19:8 Suppl 3. 41–44.
Article11. Maloney WJ. Orthopaedic crossfire--Larger femoral heads: a triumph of hope over reason! In opposition. J Arthroplasty. 2003; 18:3 Suppl 1. 85–87.
Article12. Kluess D, Martin H, Mittelmeier W, Schmitz KP, Bader R. Influence of femoral head size on impingement, dislocation and stress distribution in total hip replacement. Med Eng Phys. 2007; 29:465–471.
Article13. Jolles BM, Zangger P, Leyvraz PF. Factors predisposing to dislocation after primary total hip arthroplasty: a multivariate analysis. J Arthroplasty. 2002; 17:282–288.
Article14. Urbaniak JR, Coogan PG, Gunneson EB, Nunley JA. Treatment of osteonecrosis of the femoral head with free vascularized fibular grafting. A long-term follow-up study of one hundred and three hips. J Bone Joint Surg Am. 1995; 77:681–694.
Article15. Roberts JM, Fu FH, McClain EJ, Ferguson AB Jr. A comparison of the posterolateral and anterolateral approaches to total hip arthroplasty. Clin Orthop Relat Res. 1984; (187):205–210.
Article16. Bartz RL, Nobel PC, Kadakia NR, Tullos HS. The effect of femoral component head size on posterior dislocation of the artificial hip joint. J Bone Joint Surg Am. 2000; 82:1300–1307.
Article17. Morrey BF. Instability after total hip arthroplasty. Orthop Clin North Am. 1992; 23:237–248.
Article18. Coventry MB. Late dislocations in patients with Charnley total hip arthroplasty. J Bone Joint Surg Am. 1985; 67:832–841.
Article19. Paterno SA, Lachiewicz PF, Kelley SS. The influence of patient-related factors and the position of the acetabular component on the rate of dislocation after total hip replacement. J Bone Joint Surg Am. 1997; 79:1202–1210.
Article20. Son WY, Moon JK, Han SW, Yang JH, Yoo SY. The risk factors associated with hip dislocation after total hip replacement. J Korean Hip Soc. 2006; 18:167–172.
Article21. Suh KT, Park BG, Choi YJ. A posterior approach to primary total hip arthroplasty with soft tissue repair. Clin Orthop Relat Res. 2004; (418):162–167.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Early Dislocation Rate with Large Femoral Heads in Primary Total Hip Arthroplasty
- Current Concepts of Using Large Femoral Heads in Total Hip Arthroplasty
- Dislocation as a Complication after Total Hip Arthroplasty
- A Use of Large Femoral Head in Total Hip Arthroplasty: Early Follow-up Results
- Reduction of the Femoral Head First, and Assembly of the MUTARS® Device in Case of Impossible Reduction during Total Hip Arthroplasty