J Cerebrovasc Endovasc Neurosurg.
2018 Jun;20(2):127-132. 10.7461/jcen.2018.20.2.127.
Revision Superficial Temporal Artery-Middle Cerebral Artery Bypass Surgery for Recurrent Acute Ischemic Stroke Due to Delayed Occlusion of the Bypass Graft
- Affiliations
-
- 1Department of Neurosurgery, Busan-Ulsan Regional Cardio-Cerebrovascular Center, Dong-A University College of Medicine, Busan, Korea. nsparkhs@dau.ac.kr
- 2Department of Radiology, Busan-Ulsan Regional Cardio-cerebrovascular Center, Dong-A University College of Medicine, Busan, Korea.
- 3Department of Neurology, Busan-Ulsan Regional Cardio-cerebrovascular Center, Dong-A University College of Medicine, Busan, Korea.
- KMID: 2422607
- DOI: http://doi.org/10.7461/jcen.2018.20.2.127
Abstract
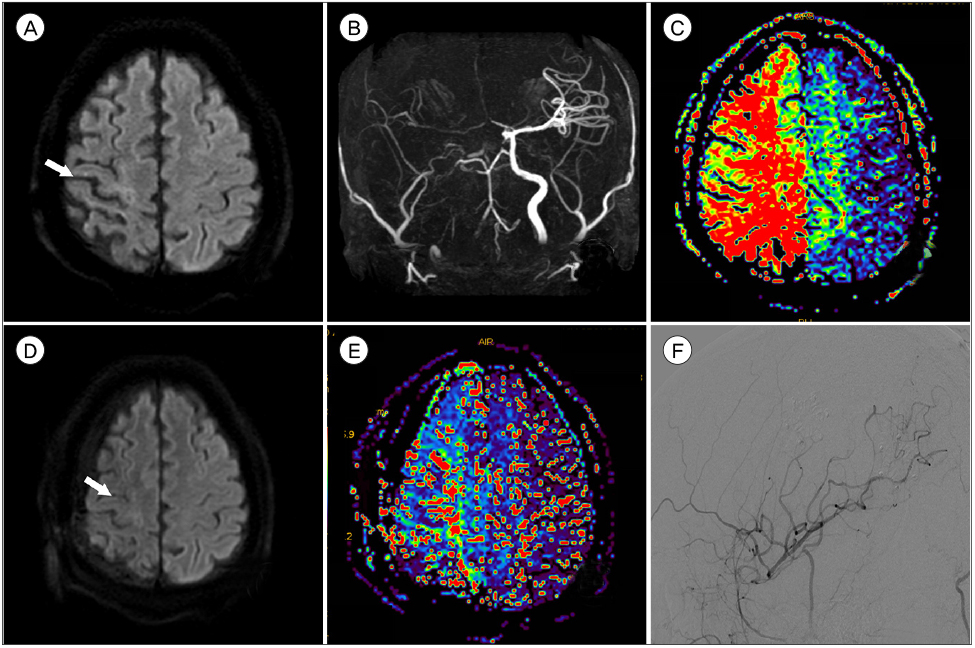
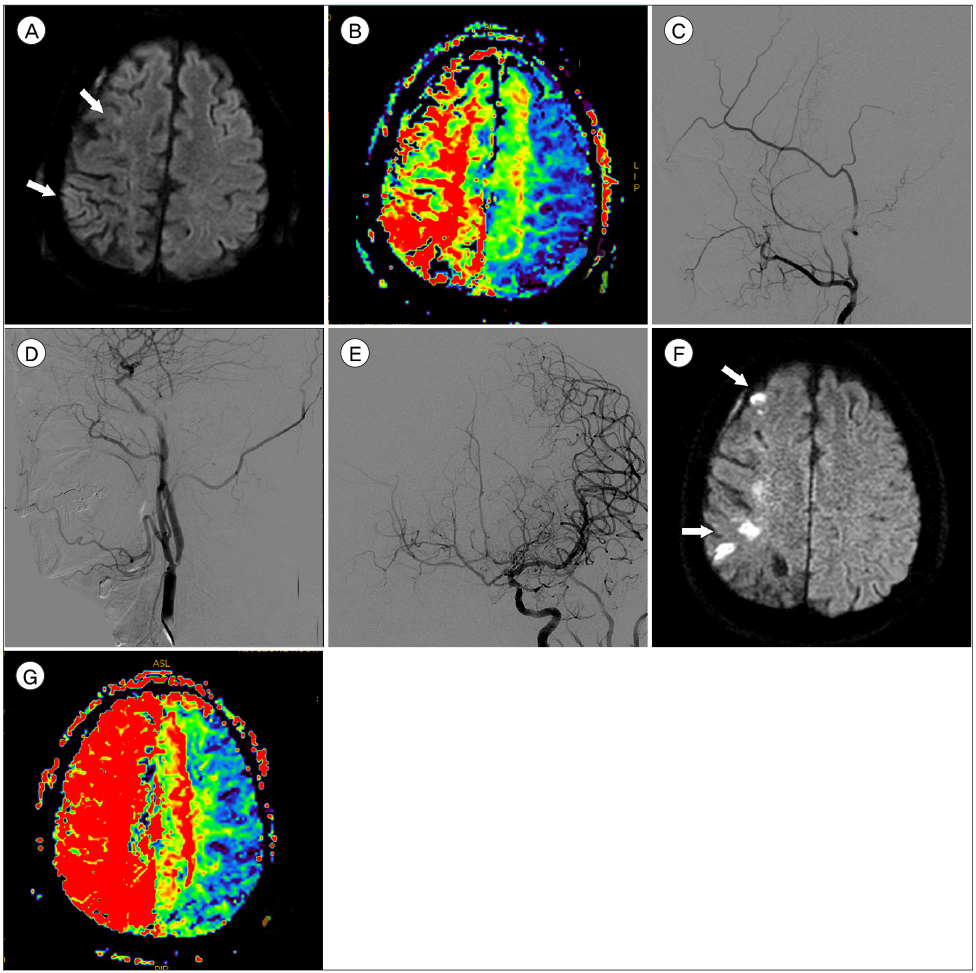
- Intravenous thrombolysis (IVT) and endovascular treatment (EVT) are currently the main treatments for reperfusion in acute ischemic stroke. Although the EVT recanalization rate has increased, unsuccessful recanalization is still observed in 10-30% cases. Superficial temporal artery-middle cerebral artery (STA-MCA) bypass is considered a rescue therapy in such cases, but in most centers it is not usually performed for acute ischemic stroke. Graft occlusion is rare following STA-MCA bypass, but it might lead to recurrent ischemic stroke. We hereby report on a patient with right MCA infarction and in whom EVT failed due to complete proximal internal carotid artery occlusion. He underwent an emergency STA-MCA bypass, resulting in a full recovery of his motor weakness. However, six months later, the patient experienced recurrent acute ischemic stroke due to bypass graft occlusion. His EVT failed again but revision bypass surgery, using STA remnant branch, was successful with full motor weakness recovery. We recommend a revision bypass surgery as a feasible therapeutic option for recurrent cerebral infarction caused by delayed STA graft occlusion.
MeSH Terms
Figure
Reference
-
1. Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015; 03. 372(11):1009–1018.
Article2. Cherian J, Srinivasan V, Kan P, Duckworth EAM. Double-barrel superficial temporal artery-middle cerebral artery bypass: can it be considered “high-flow?”. Oper Neurosurg (Hagerstown). 2018; 03. 14(3):288–294.
Article3. Choi JH, Park HS. Emergent Double-barrel bypass shortly after intravenous administration of recombinant tissue plasminogen activator for acute ischemic stroke. J Cerebrovasc Endovasc Neurosurg. 2016; 09. 18(3):258–263.
Article4. Duckworth EA, Rao VY, Patel AJ. Double-barrel bypass for cerebral ischemia: technique, rationale, and preliminary experience with 10 consecutive cases. Neurosurgery. 2013; 09. 73:1 Suppl Operative. ons30–ons38. discussion ons37-8.
Article5. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015; 03. 372(11):1019–1030.6. Halsey JH Jr, Morawetz RB, Blauenstein UW. The hemodynamic effect of STA-MCA bypass. Stroke. 1982; Mar-Apr. 13(2):163–167.
Article7. Hong KS, Bang OY, Kang DW, Yu KH, Bae HJ, Lee JS, et al. Stroke statistics in Korea: part I. Epidemiology and risk factors: a report from the korean stroke society and clinical research center for stroke. J Stroke. 2013; 01. 15(1):2–20.
Article8. Hwang G, Oh CW, Bang JS, Jung CK, Kwon OK, Kim JE, et al. Superficial temporal artery to middle cerebral artery bypass in acute ischemic stroke and stroke in progress. Neurosurgery. 2011; 03. 68(3):723–729. discussion 729-30.
Article9. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015; 06. 372(24):2296–2306.
Article10. Kim MJ, Kang SY, Kwon SB, Jung S, Lee MJ, Jeong MG, et al. Contralateral cerebral infarction after unilateral carotid angioplasty with stenting. J Neurocrit Care. 2008; 12. 1(2):164–167.11. Nussbaum ES, Janjua TM, Defillo A, Lowary JL, Nussbaum LA. Emergency extracranial-intracranial bypass surgery for acute ischemic stroke. J Neurosurg. 2010; 03. 112(3):666–673.
Article12. Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015; 06. 372(24):2285–2295.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Emergency Superficial Temporal Middle Cerebral Artery Bypass Surgery for Acute Symptomatic Middle Cerebral Artery Occlusion With Hemodynamic Disturbance
- STA-Distal ACA Bypass Using a Contralateral STA Interposition Graft for Symptomatic ACA Stenosis
- ST A-MCA Anastomosis in Ischemic Stroke
- Revascularization for Symptomatic Occlusion of the Anterior Cerebral Artery Using Superficial Temporal Artery
- Internal maxillary artery (IMax) – middle cerebral artery bypass in a patient with bilateral atherosclerotic carotid occlusion: A technical case report