Korean Circ J.
2018 Nov;48(11):1002-1011. 10.4070/kcj.2018.0048.
Prognostic Significance of Left Axis Deviation in Acute Heart Failure Patients with Left Bundle branch block: an Analysis from the Korean Acute Heart Failure (KorAHF) Registry
- Affiliations
-
- 1Division of Cardiology, Department of Medicine, Sungkyunkwan University School of Medicine, Seoul, Korea. esjeon1107@gmail.com
- 2Division of Cardiology, Department of Medicine, Keimyung University Dongsan Medical Center, Daegu, Korea.
- 3Division of Cardiology, Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea.
- 4Division of Cardiology, Department of Medicine, University of Ulsan College of Medicine, Seoul, Korea.
- 5Division of Cardiology, Department of Medicine, Kyungpook National University College of Medicine, Daegu, Korea.
- 6Division of Cardiology, Department of Medicine, The Catholic University of Korea, Seoul, Korea.
- 7Division of Cardiology, Department of Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 8Division of Cardiology, Department of Medicine, Seoul National University Bundang Hospital, Seongnam, Korea.
- 9Division of Cardiology, Department of Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 10Division of Cardiology, Department of Medicine, Heart Research Center of Chonnam National University, Gwangju, Korea.
- 11Division of Cardiology, Department of Medicine, Chungbuk National University College of Medicine, Cheongju, Korea.
- 12Division of Cardiovascular and Rare Diseases, Department of Biomedical Science, National Institute of Health (NIH), Osong, Korea.
- KMID: 2422548
- DOI: http://doi.org/10.4070/kcj.2018.0048
Abstract
- BACKGROUND AND OBJECTIVES
The prognostic impact of left axis deviation (LAD) on clinical outcomes in acute heart failure syndrome (AHFS) with left bundle branch block (LBBB) is unknown. The aim of this study was to determine the prognostic significance of axis deviation in acute heart failure patients with LBBB.
METHODS
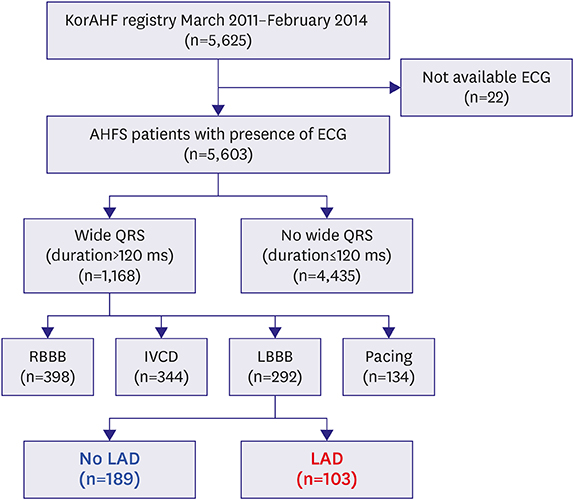
Between March 2011 and February 2014, 292 consecutive AHFS patients with LBBB were recruited from 10 tertiary university hospitals. They were divided into groups with no LAD (n=189) or with LAD (n=103) groups according to QRS axis <−30 degree. The primary outcome was all-cause mortality.
RESULTS
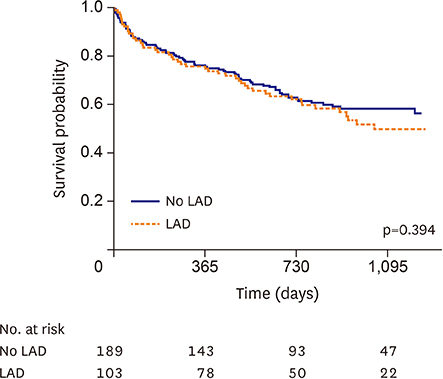
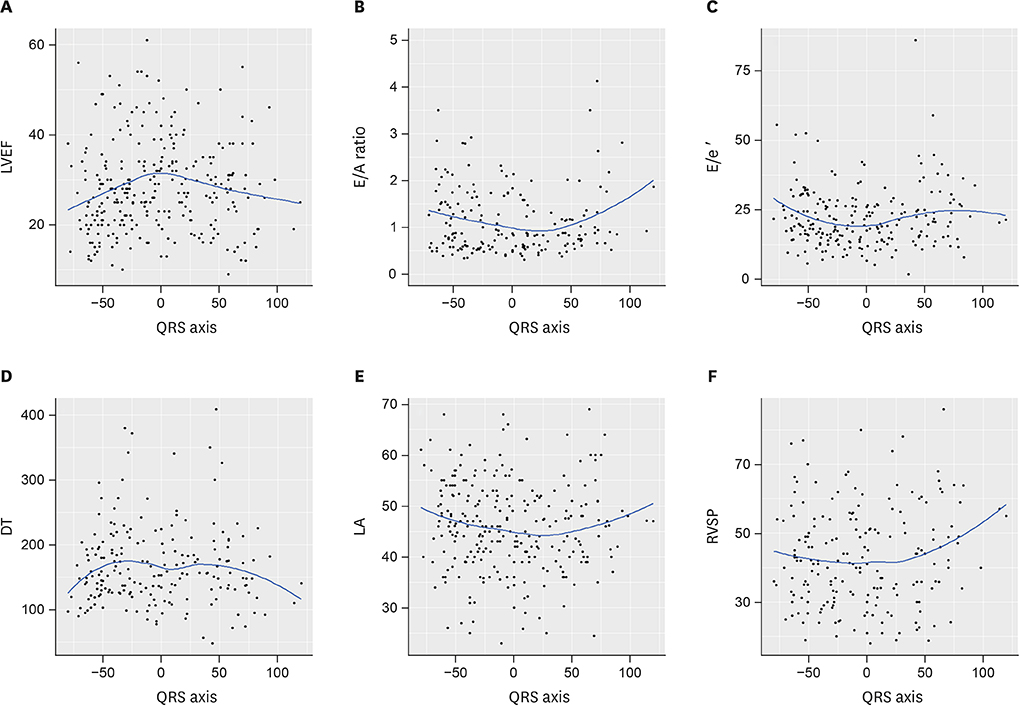
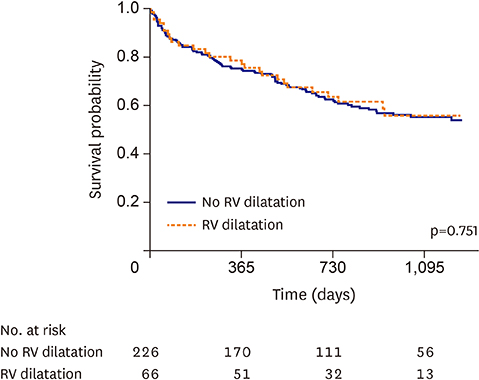
The median follow-up duration was 24 months. On multivariate analysis, the rate of all-cause death did not significantly differ between the normal axis and LAD groups (39.7% vs. 46.6%, adjusted hazard ratio, 1.01; 95% confidence interval, 0.66, 1.53; p=0.97). However, on the multiple linear regression analysis to evaluate the predictors of the left ventricular ejection fraction (LVEF), presence of LAD significantly predicted a worse LVEF (adjusted beta, −3.25; 95% confidence interval, −5.82, −0.67; p=0.01). Right ventricle (RV) dilatation was defined as at least 2 of 3 electrocardiographic criteria (late R in lead aVR, low voltages in limb leads, and R/S ratio < 1 in lead V5) and was more frequent in the LAD group than in the normal axis group (p < 0.001).
CONCLUSIONS
Among the AHFS with LBBB patients, LAD did not predict mortality, but it could be used as a significant predictor of worse LVEF and RV dilatation (Trial registry at KorAHF registry, ClinicalTrial.gov, NCT01389843).
MeSH Terms
Figure
Cited by 1 articles
-
Left Axis Deviation in Patients with Acute Heart Failure with Left Bundle Branch Block: Does It Really Matter?
Eue-Keun Choi
Korean Circ J. 2018;48(11):1012-1013. doi: 10.4070/kcj.2018.0222.
Reference
-
1. Baldasseroni S, Opasich C, Gorini M, et al. Left bundle-branch block is associated with increased 1-year sudden and total mortality rate in 5517 outpatients with congestive heart failure: a report from the Italian network on congestive heart failure. Am Heart J. 2002; 143:398–405.
Article2. Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016; 37:2129–2200.3. Bristow MR, Saxon LA, Boehmer J, et al. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N Engl J Med. 2004; 350:2140–2150.
Article4. Zusterzeel R, Selzman KA, Sanders WE, et al. Cardiac resynchronization therapy in women: US Food and Drug Administration meta-analysis of patient-level data. JAMA Intern Med. 2014; 174:1340–1348.5. Zareba W, Klein H, Cygankiewicz I, et al. Effectiveness of cardiac resynchronization therapy by QRS morphology in the Multicenter Automatic Defibrillator Implantation Trial-Cardiac Resynchronization Therapy (MADIT-CRT). Circulation. 2011; 123:1061–1072.
Article6. Brenyo A, Rao M, Barsheshet A, et al. QRS axis and the benefit of cardiac resynchronization therapy in patients with mildly symptomatic heart failure enrolled in MADIT-CRT. J Cardiovasc Electrophysiol. 2013; 24:442–448.
Article7. Rabkin SW, Mathewson FA, Tate RB. Natural history of marked left axis deviation (left anterior hemiblock). Am J Cardiol. 1979; 43:605–611.
Article8. Yano K, Peskoe SM, Rhoads GG, Moore JO, Kagan A. Left axis deviation and left anterior hemiblock among 8,000 Japanese-American men. Am J Cardiol. 1975; 35:809–815.
Article9. Swiryn S, Abben R, Denes P, Rosen KM. Electrocardiographic determinants of axis during left bundle branch block: study in patients with intermittent left bundle branch block. Am J Cardiol. 1980; 46:53–58.
Article10. Flowers NC. Left bundle branch block: a continuously evolving concept. J Am Coll Cardiol. 1987; 9:684–697.
Article11. Dhingra RC, Amat-Y-Leon F, Wyndham C, et al. Significance of left axis deviation in patients with chronic left bundle branch block. Am J Cardiol. 1978; 42:551–556.
Article12. Park CS, Cha MJ, Choi EK, Oh S. Prognostic implication of the QRS axis and its association with myocardial scarring in patients with left bundle branch block. Korean Circ J. 2017; 47:263–269.
Article13. Patel PJ, Verdino RJ. Usefulness of QRS axis change to predict mortality in patients with left bundle branch block. Am J Cardiol. 2013; 112:390–394.
Article14. Surawicz B, Childers R, Deal BJ, et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part III: intraventricular conduction disturbances: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. J Am Coll Cardiol. 2009; 53:976–981.15. Lee SE, Cho HJ, Lee HY, et al. A multicentre cohort study of acute heart failure syndromes in Korea: rationale, design, and interim observations of the Korean Acute Heart Failure (KorAHF) registry. Eur J Heart Fail. 2014; 16:700–708.
Article16. Lee SE, Lee HY, Cho HJ, et al. Clinical characteristics and outcome of acute heart failure in Korea: results from the Korean Acute Heart Failure Registry (KorAHF). Korean Circ J. 2017; 47:341–353.
Article17. Schiller NB, Shah PM, Crawford M, et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr. 1989; 2:358–367.18. Van Bommel RJ, Marsan NA, Delgado V, et al. Value of the surface electrocardiogram in detecting right ventricular dilatation in the presence of left bundle branch block. Am J Cardiol. 2011; 107:736–740.
Article19. Lichstein E, Mahapatra R, Gupta PK, Chadda KD. Significance of complete left bundle branch block with left axis deviation. Am J Cardiol. 1979; 44:239–242.
Article20. Perrotta L, Kandala JD, Biase L, et al. Prognostic Impact of QRS axis deviation in patients treated with cardiac resynchronization therapy. J Cardiovasc Electrophysiol. 2016; 27:315–320.
Article21. Das MK, Cheriparambil K, Bedi A, et al. Prolonged QRS duration (QRS >/=170 ms) and left axis deviation in the presence of left bundle branch block: A marker of poor left ventricular systolic function? Am Heart J. 2001; 142:756–759.22. Havelda CJ, Sohi GS, Flowers NC, Horan LG. The pathologic correlates of the electrocardiogram: complete left bundle branch block. Circulation. 1982; 65:445–451.
Article23. Haft JI, Herman MV, Gorlin R. Left bundle branch block: etiologic, hemodynamic, and ventriculographic considerations. Circulation. 1971; 43:279–287.24. de Groote P, Millaire A, Foucher-Hossein C, et al. Right ventricular ejection fraction is an independent predictor of survival in patients with moderate heart failure. J Am Coll Cardiol. 1998; 32:948–954.
Article25. Ghio S, Gavazzi A, Campana C, et al. Independent and additive prognostic value of right ventricular systolic function and pulmonary artery pressure in patients with chronic heart failure. J Am Coll Cardiol. 2001; 37:183–188.
Article26. Damy T, Ghio S, Rigby AS, et al. Interplay between right ventricular function and cardiac resynchronization therapy: an analysis of the CARE-HF trial (Cardiac Resynchronization-Heart Failure). J Am Coll Cardiol. 2013; 61:2153–2160.27. Sharma A, Bax JJ, Vallakati A, et al. Meta-analysis of the relation of baseline right ventricular function to response to cardiac resynchronization therapy. Am J Cardiol. 2016; 117:1315–1321.
Article28. Rapacciuolo A, Maffè S, Palmisano P, et al. Prognostic role of right ventricular function in patients with heart failure undergoing cardiac resynchronization therapy. Clin Cardiol. 2016; 39:640–645.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Left Axis Deviation in Patients with Acute Heart Failure with Left Bundle Branch Block: Does It Really Matter?
- Prognostic Implication of the QRS Axis and its Association with Myocardial Scarring in Patients with Left Bundle Branch Block
- Rate-dependent Left Bundle Branch Block during General Anesthesia : A case report
- Paradigm Shifts of Heart Failure Therapy: Do We Need Another Paradigm?
- A Clinical Report of Anesthetic Management on the Patient with Complete Left Bundle Branch Block