Korean Circ J.
2018 Nov;48(11):989-999. 10.4070/kcj.2017.0387.
Complete Versus Culprit-Only Revascularization for ST-Segment Elevation Myocardial Infarction and Multivessel Disease in the 2(nd) Generation Drug-Eluting Stent Era: Data from the INTERSTELLAR Registry
- Affiliations
-
- 1Department of Cardiology, Inha University Hospital, Incheon, Korea. denki1@inha.ac.kr
- 2Department of Cardiology, Gachon University Gil Medical Center, Incheon, Korea.
- 3Department of Cardiology, Sejong General Hospital, Bucheon, Korea.
- 4Department of Cardiology, Soonchunhyang University Bucheon Hospital, Bucheon, Korea. denki1@inha.ac.kr
- KMID: 2422546
- DOI: http://doi.org/10.4070/kcj.2017.0387
Abstract
- BACKGROUND AND OBJECTIVES
We aimed to compare outcomes of complete revascularization (CR) versus culprit-only revascularization for ST-segment elevation myocardial infarction (STEMI) and multivessel disease (MVD) in the 2nd generation drug-eluting stent (DES) era.
METHODS
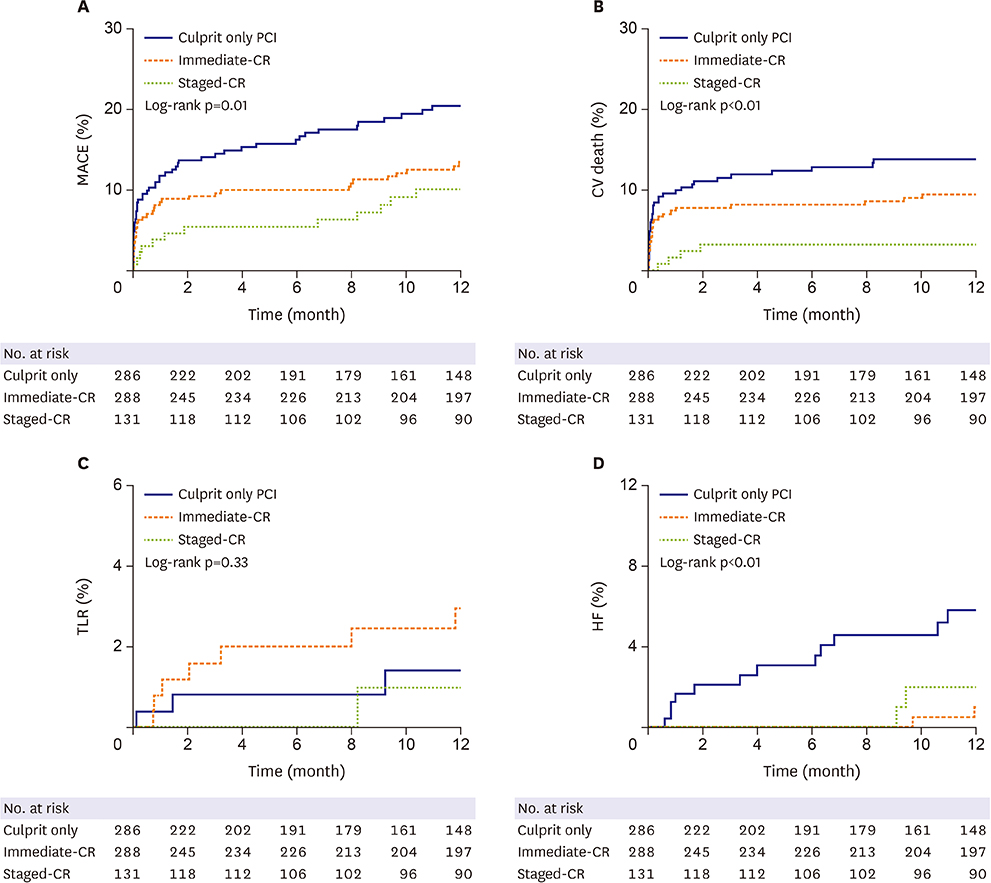
From 2009 to 2014, patients with STEMI and MVD, who underwent primary percutaneous coronary intervention (PCI) using a 2nd generation DES for culprit lesions were enrolled. CR was defined as PCI for a non-infarct-related artery during the index admission. Major adverse cardiovascular event (MACE) was defined as cardiovascular (CV) death, non-fatal myocardial infarction, target lesion revascularization, or heart failure during the follow-up year.
RESULTS
In total, 705 MVD patients were suitable for the analysis, of whom 286 (41%) underwent culprit-only PCI and 419 (59%) underwent CR during the index admission. The incidence of MACE was 11.5% in the CR group versus 18.5% in the culprit-only group (hazard ratio [HR], 0.56; 95% confidence interval [CI], 0.37-0.86; p<0.01; adjusted HR, 0.64; 95% CI, 0.40-0.99; p=0.04). The CR group revealed a significantly lower incidence of CV death (7.2% vs. 12.9%; HR, 0.51; 95% CI, 0.31-0.86; p=0.01 and adjusted HR, 0.57; 95% CI; 0.32-0.97; p=0.03, respectively).
CONCLUSIONS
CR was associated with better outcomes including reductions in MACE and CV death at 1 year of follow-up compared with culprit-only PCI in the 2nd generation DES era.
MeSH Terms
Figure
Cited by 2 articles
-
Treat or Not to Treat Non-culprit Coronary Artery with Significant Stenosis during Primary Percutaneous Coronary Intervention
Seung-Jun Lee, Jung-Sun Kim
Korean Circ J. 2018;48(11):1000-1001. doi: 10.4070/kcj.2018.0193.Optimal Timing of Coronary Intervention in Non-Culprit Lesion in ST Elevation Myocardial Infarction with Multi-Vessel Disease
Jongkwon Seo, Jung-Sun Kim
Korean Circ J. 2020;50(3):234-235. doi: 10.4070/kcj.2020.0041.
Reference
-
1. Wald DS, Morris JK, Wald NJ, et al. Randomized trial of preventive angioplasty in myocardial infarction. N Engl J Med. 2013; 369:1115–1123.
Article2. Gershlick AH, Khan JN, Kelly DJ, et al. Randomized trial of complete versus lesion-only revascularization in patients undergoing primary percutaneous coronary intervention for STEMI and multivessel disease: the CvLPRIT trial. J Am Coll Cardiol. 2015; 65:963–972.3. Engstrøm T, Kelbæk H, Helqvist S, et al. Complete revascularisation versus treatment of the culprit lesion only in patients with ST-segment elevation myocardial infarction and multivessel disease (DANAMI-3—PRIMULTI): an open-label, randomised controlled trial. Lancet. 2015; 386:665–671.
Article4. Levine GN, Bates ER, Blankenship JC, et al. 2015 ACC/AHA/SCAI focused update on primary percutaneous coronary intervention for patients with ST-elevation myocardial infarction: an update of the 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention and the 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction. J Am Coll Cardiol. 2016; 67:1235–1250.5. Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC). Steg PG, James SK, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012; 33:2569–2619.6. Dahal K, Rijal J, Panta R, Lee J, Azrin M, Lootens R. Multi-vessel versus culprit-vessel and staged percutaneous coronary intervention in STEMI patients with multivessel disease: a meta-analysis of randomized controlled trials. Cardiovasc Revasc Med. 2014; 15:408–413.
Article7. El-Hayek GE, Gershlick AH, Hong MK, et al. Meta-analysis of randomized controlled trials comparing multivessel versus culprit-only revascularization for patients with ST-segment elevation myocardial infarction and multivessel disease undergoing primary percutaneous coronary intervention. Am J Cardiol. 2015; 115:1481–1486.
Article8. Villablanca PA, Briceno DF, Massera D, et al. Culprit-lesion only versus complete multivessel percutaneous intervention in ST-elevation myocardial infarction: A systematic review and meta-analysis of randomized trials. Int J Cardiol. 2016; 220:251–259.
Article9. Anantha Narayanan M, Reddy YN, Sundaram V, et al. What is the optimal approach to a non- culprit stenosis after ST-elevation myocardial infarction - Conservative therapy or upfront revascularization? An updated meta-analysis of randomized trials. Int J Cardiol. 2016; 216:18–24.
Article10. Baber U, Mehran R, Sharma SK, et al. Impact of the everolimus-eluting stent on stent thrombosis: a meta-analysis of 13 randomized trials. J Am Coll Cardiol. 2011; 58:1569–1577.11. Palmerini T, Biondi-Zoccai G, Della Riva D, et al. Stent thrombosis with drug-eluting and bare-metal stents: evidence from a comprehensive network meta-analysis. Lancet. 2012; 379:1393–1402.
Article12. Räber L, Magro M, Stefanini GG, et al. Very late coronary stent thrombosis of a newer-generation everolimus-eluting stent compared with early-generation drug-eluting stents: a prospective cohort study. Circulation. 2012; 125:1110–1121.13. Cutlip DE, Windecker S, Mehran R, et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007; 115:2344–2351.14. Mauri L, Kereiakes DJ, Yeh RW, et al. Twelve or 30 months of dual antiplatelet therapy after drug-eluting stents. N Engl J Med. 2014; 371:2155–2166.15. Nordmann AJ, Briel M, Bucher HC. Mortality in randomized controlled trials comparing drug-eluting vs. bare metal stents in coronary artery disease: a meta-analysis. Eur Heart J. 2006; 27:2784–2814.
Article16. Ong AT, McFadden EP, Regar E, de Jaegere PP, van Domburg RT, Serruys PW. Late angiographic stent thrombosis (LAST) events with drug-eluting stents. J Am Coll Cardiol. 2005; 45:2088–2092.
Article17. Navarese EP, Kubica J, Castriota F, et al. Safety and efficacy of biodegradable vs. durable polymer drug-eluting stents: evidence from a meta-analysis of randomised trials. EuroIntervention. 2011; 7:985–994.
Article18. Di Lorenzo E, Sauro R, Varricchio A, et al. Randomized comparison of everolimus-eluting stents and sirolimus-eluting stents in patients with ST elevation myocardial infarction: RACES-MI trial. JACC Cardiovasc Interv. 2014; 7:849–856.19. Sarno G, Lagerqvist B, Nilsson J, et al. Stent thrombosis in new-generation drug-eluting stents in patients with STEMI undergoing primary PCI: a report from SCAAR. J Am Coll Cardiol. 2014; 64:16–24.20. Giustino G, Baber U, Stefanini GG, et al. Impact of clinical presentation (stable angina pectoris vs unstable angina pectoris or non-ST-elevation myocardial infarction vs ST-elevation myocardial infarction) on long-term outcomes in women undergoing percutaneous coronary intervention with drug-eluting stents. Am J Cardiol. 2015; 116:845–852.
Article21. Di Lorenzo E, Sauro R, Capasso M, et al. Long-term results of the randomized comparison of everolimus-eluting stents and sirolimus-eluting stent in patients with ST elevation myocardial infarction (RACES-MI trial). Int J Cardiol. 2016; 202:177–182.
Article22. Politi L, Sgura F, Rossi R, et al. A randomised trial of target-vessel versus multi-vessel revascularisation in ST-elevation myocardial infarction: major adverse cardiac events during long-term follow-up. Heart. 2010; 96:662–667.
Article23. Di Mario C, Mara S, Flavio A, et al. Single vs multivessel treatment during primary angioplasty: results of the multicentre randomised HEpacoat for cuLPrit or multivessel stenting for Acute Myocardial Infarction (HELP AMI) Study. Int J Cardiovasc Intervent. 2004; 6:128–133.24. Thiele H, Akin I, Sandri M, et al. PCI strategies in patients with acute myocardial infarction and cardiogenic shock. N Engl J Med. 2017; 377:2419–2432.25. Yu X, Li Y, Wang Q, Liang M, Xu K, Han Y. “One-time” versus staged multivessel intervention in intermediate to very high-risk patients with non-ST-segment elevation acute coronary syndromes. Korean Circ J. 2016; 46:774–783.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Status of Coronary Intervention in Patients with ST-Segment Elevation Myocardial Infarction and Multivessel Coronary Artery Disease
- Drug-Eluting Stent: Present and Future
- Culprit-Lesion-Only Versus Multivessel Revascularization Using Drug-Eluting Stents in Patients With ST-Segment Elevation Myocardial Infarction: A Korean Acute Myocardial Infarction Registry-Based Analysis
- Three-Year Outcomes Based on Left Ventricular Ejection Fraction in Patients With Non-ST-Segment Elevation Myocardial Infarction Undergoing Newer-Generation Drug-Eluting Stent Implantation
- Intracoronary Imaging-Guided Revascularization for Non-Culprit Lesions in Patients With ST-Elevation Myocardial Infarction and Multivessel Disease