Pediatr Gastroenterol Hepatol Nutr.
2018 Oct;21(4):297-305. 10.5223/pghn.2018.21.4.297.
Epidemiology of Hyperbilirubinemia in a Quaternary Pediatric Emergency Department over a Three-Year Period
- Affiliations
-
- 1Division of Emergency Medicine, Phoenix Children's Hospital, Phoenix, AZ, United States. ztimmons@phoenixchildrens.com
- 2Division of Pediatrics, Cardon Children's Medical Center, Mesa, AZ, United States.
- 3Division of Gastroenterology, Texas Children's Hospital, Houston, TX, United States.
- KMID: 2421992
- DOI: http://doi.org/10.5223/pghn.2018.21.4.297
Abstract
- PURPOSE
There is a lack of scholarly reports on pediatric emergency department (PED) exposure to hyperbilirubinemia. We aimed to describe the epidemiology of hyperbilirubinemia in patients presenting to a PED over a three-year period.
METHODS
This was a retrospective cohort study, completed at an urban quaternary academic PED. Patients were included if they presented to the PED from 2010 to 2012, were 0 to 18 years in age, and had an elevated serum bilirubin for age. A chart review was completed to determine the incidence of hyperbilirubinemia, etiology, diagnostic work up and prognosis. The data set was stratified into four age ranges.
RESULTS
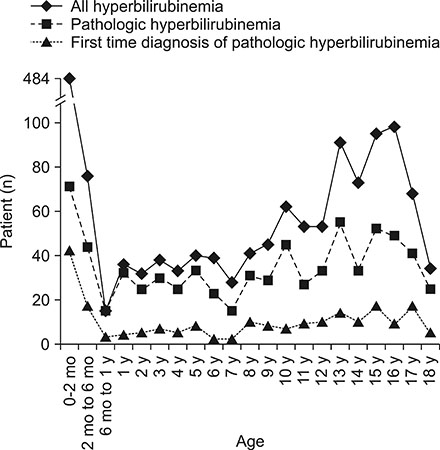
We identified 1,534 visits where a patient was found to have hyperbilirubinemia (0.8% of all visits). In 47.7% of patients hyperbilirubinemia was determined to have arisen from an identifiable pathologic etiology (0.38% of all visits). First-time diagnosis of pathologic hyperbilirubinemia occurred in 14% of hyperbilirubinemia visits (0.11% of all visits). There were varying etiologies of hyperbilirubinemia across age groups but a male predominance in all (55.0%). 15 patients went on to have a liver transplant and 20 patients died. First-time pathologic hyperbilirubinemia patients had a mortality rate of 0.95% for their initial hospitalization.
CONCLUSION
Hyperbilirubinemia was not a common presentation to the PED and a minority of cases were pathologic in etiology. The etiologies of hyperbilirubinemia varied across each of our study age groups. A new discovery of pathologic hyperbilirubinemia and progression to liver transplant or death during the initial presentation was extremely rare.
Keyword
MeSH Terms
Figure
Reference
-
1. Colletti JE, Kothari S, Jackson DM, Kilgore KP, Barringer K. An emergency medicine approach to neonatal hyperbilirubinemia. Emerg Med Clin North Am. 2007; 25:1117–1135. vii
Article2. Harb R, Thomas DW. Conjugated hyperbilirubinemia: screening and treatment in older infants and children. Pediatr Rev. 2007; 28:83–91.
Article3. Miloh T, Breglio KJ, Chu J. Treatment of pediatric patients with jaundice in the ED. Pediatr Emerg Med Pract. 2010; 7.4. Moyer V, Freese DK, Whitington PF, Olson AD, Brewer F, Colletti RB, et al. Guideline for the evaluation of cholestatic jaundice in infants: recommendations of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr. 2004; 39:115–128.
Article5. Leung AK, Sauve RS. Breastfeeding and breast milk jaundice. J R Soc Health. 1989; 109:213–217.
Article6. Shapiro SM. Bilirubin toxicity in the developing nervous system. Pediatr Neurol. 2003; 29:410–421.
Article7. Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013; 41:580–637.
Article8. Fretzayas A, Moustaki M, Liapi O, Karpathios T. Gilbert syndrome. Eur J Pediatr. 2012; 171:11–15.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Implementation of Quaternary Prevention in the Korean Healthcare System: Lessons From the 2015 Middle East Respiratory Syndrome Coronavirus Outbreak in the Republic of Korea
- Neonatal Hyperbilirubinemia
- Phototherapy for Neonatal Hyperbilirubinemia
- Evaluation of transcutaneous minolta bilirubinometer in neonatal hyperbilirubinemia
- A Clinical Observation of Neonatal Hyperbilirubinemia due to ABO Incompatibility