Pediatr Gastroenterol Hepatol Nutr.
2018 Oct;21(4):289-296. 10.5223/pghn.2018.21.4.289.
Validation of Serum Aminotransferases Levels to Define Severe Dengue Fever in Children
- Affiliations
-
- 1Department of Pediatrics, Era's Lucknow Medical College, Lucknow, India. drchhavi.nanda@gmail.com
- 2Department of Gastroenterology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India.
- KMID: 2421991
- DOI: http://doi.org/10.5223/pghn.2018.21.4.289
Abstract
- PURPOSE
We aimed to study the pattern of liver-injury in children with dengue fever (DF) and validate serum aminotransferase ≥1,000 IU/L as a marker of severe DF.
METHODS
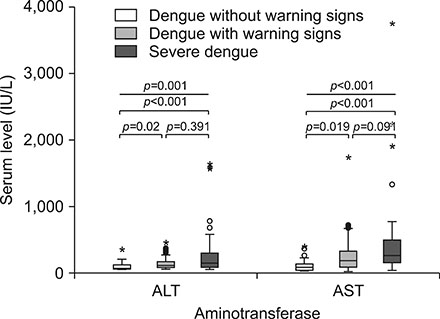
Children admitted with DF were included. DF was defined by presence of clinical criteria and positive serological or antigen tests in absence of other etiology. DF severity was graded as dengue without or with warning signs and severe dengue. Liver-injury was defined as alanine aminotransferase (ALT) more than twice the upper limit of normal (boys, 30 IU/L; girls, 21 IU/L).
RESULTS
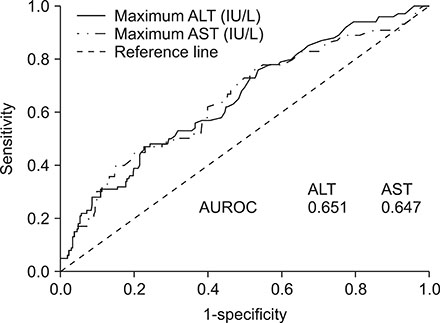
Of 372 children with DF, 144 (38.7%) had liver-injury. Risk of liver-injury and aminotransferase levels increased with DF severity (p < 0.001). Recommended ALT and aspartate aminotransferase (AST) cut-off at ≥1,000 IU/L had sensitivity 4.8% (5/105), specificity 99.3% (265/267) for detection of severe DF. In children with ALT and AST < 1,000 IU/L (n=365), the area under receiver operating curves for prediction for severe DF, were 0.651 (95% confidence interval [CI], 0.588-0.714; p < 0.001) for ALT and 0.647 (95% CI, 0.582-0.712; p < 0.001) for AST. Serum ALT at 376 IU/L and AST at 635 IU/L had sensitivity and specificity comparable to ≥1,000 IU/L for defining severe DF.
CONCLUSION
Liver-injury is common in DF. The ALT and AST levels increase with DF severity. ALT and AST levels of ≥1,000 IU/L could be lowered to 376 IU/L and 635 IU/L respectively for defining severe DF.
MeSH Terms
Figure
Reference
-
1. World Health Organization. Dengue: guidelines for diagnosis treatment prevention and control. Geneva: WHO;2009. p. 147.2. World Health Organization. Dengue haemorrhagic fever: diagnosis, treatment, prevention and control. Geneva: WHO;1997. p. 84.3. Alexander N, Balmaseda A, Coelho IC, Dimaano E, Hien TT, Hung NT, et al. Multicentre prospective study on dengue classification in four South-east Asian and three Latin American countries. Trop Med Int Health. 2011; 16:936–948.
Article4. Barniol J, Gaczkowski R, Barbato EV, da Cunha RV, Salgado D, Martinez E, et al. Usefulness and applicability of the revised dengue case classification by disease: multi-centre study in 18 countries. BMC Infect Dis. 2011; 11:106.
Article5. Seneviratne SL, Malavige GN, de Silva HJ. Pathogenesis of liver involvement during dengue viral infections. Trans R Soc Trop Med Hyg. 2006; 100:608–614.
Article6. Ling LM, Wilder-Smith A, Leo YS. Fulminant hepatitis in dengue haemorrhagic fever. J Clin Virol. 2007; 38:265–268.
Article7. Souza LJ, Alves JG, Nogueira RM, Gicovate Neto C, Bastos DA, Siqueira EW, et al. Aminotransferase changes and acute hepatitis in patients with dengue fever: analysis of 1,585 cases. Braz J Infect Dis. 2004; 8:156–163.
Article8. Kye Mon K, Nontprasert A, Kittitrakul C, Tangkijvanich P, Leowattana W, Poovorawan K. Incidence and clinical outcome of acute liver failure caused by dengue in a hospital for tropical diseases, Thailand. Am J Trop Med Hyg. 2016; 95:1338–1344.
Article9. Ahmad S, Dhar M, Srivastava S, Bhat NK, Shirazi N, Biswas D, et al. Dengue hepatitis sans dysfunction: experience of a single tertiary referral centre in the north Indian state of Uttarakhand. Trop Doct. 2013; 43:62–65.
Article10. Itha S, Kashyap R, Krishnani N, Saraswat VA, Choudhuri G, Aggarwal R. Profile of liver involvement in dengue virus infection. Natl Med J India. 2005; 18:127–130.11. Saha AK, Maitra S, Hazra SCh. Spectrum of hepatic dysfunction in 2012 dengue epidemic in Kolkata, West Bengal. Indian J Gastroenterol. 2013; 32:400–403.
Article12. Poustchi H, George J, Esmaili S, Esna-Ashari F, Ardalan G, Sepanlou SG, et al. Gender differences in healthy ranges for serum alanine aminotransferase levels in adolescence. PLoS One. 2011; 6:e21178.
Article13. Schiff ER, Sorrell MF, Maddrey WC, Schiff L. Schiff's diseases of the liver. 10th ed. Philadelphia, PA: Lippincott Williams & Wilkins;2007.14. Roy A, Sarkar D, Chakraborty S, Chaudhuri J, Ghosh P, Chakraborty S. Profile of hepatic involvement by dengue virus in dengue infected children. N Am J Med Sci. 2013; 5:480–485.
Article15. Jagadishkumar K, Jain P, Manjunath VG, Umesh L. Hepatic involvement in dengue fever in children. Iran J Pediatr. 2012; 22:231–236.16. Martinez Vega R, Phumratanaprapin W, Phonrat B, Dhitavat J, Sutherat M, Choovichian V. Differences in liver impairment between adults and children with dengue infection. Am J Trop Med Hyg. 2016; 94:1073–1079.
Article17. Chongsrisawat V, Hutagalung Y, Poovorawan Y. Liver function test results and outcomes in children with acute liver failure due to dengue infection. Southeast Asian J Trop Med Public Health. 2009; 40:47–53.18. Lee LK, Gan VC, Lee VJ, Tan AS, Leo YS, Lye DC. Clinical relevance and discriminatory value of elevated liver aminotransferase levels for dengue severity. PLoS Negl Trop Dis. 2012; 6:e1676.
Article19. Chhavi N, Zutshi K, Singh NK, Awasthi A, Goel A. Serum liver enzyme pattern in birth asphyxia associated liver injury. Pediatr Gastroenterol Hepatol Nutr. 2014; 17:162–169.
Article