Korean J Pain.
2018 Oct;31(4):277-288. 10.3344/kjp.2018.31.4.277.
Comparison of effectiveness for fluoroscopic cervical interlaminar epidural injections with or without steroid in cervical post-surgery syndrome
- Affiliations
-
- 1Pain Management Center of Paducah, Paducah, Kentucky, USA. drlm@thepainmd.com
- 2Massachusetts General Hospital and Harvard Medical School, Boston, MA, USA.
- KMID: 2421519
- DOI: http://doi.org/10.3344/kjp.2018.31.4.277
Abstract
- BACKGROUND
Neck and back pain are leading sources of disability placing substantial burden on health care systems. Surgical interventions in managing chronic neck pain secondary to various disorders continue to increase. Even though surgical interventions are effective, a significant proportion of patients continue to have symptomatology and develop cervical post-surgery syndrome. This study was performed to know the effectiveness of cervical interlaminar epidural injections with or without steroids.
METHODS
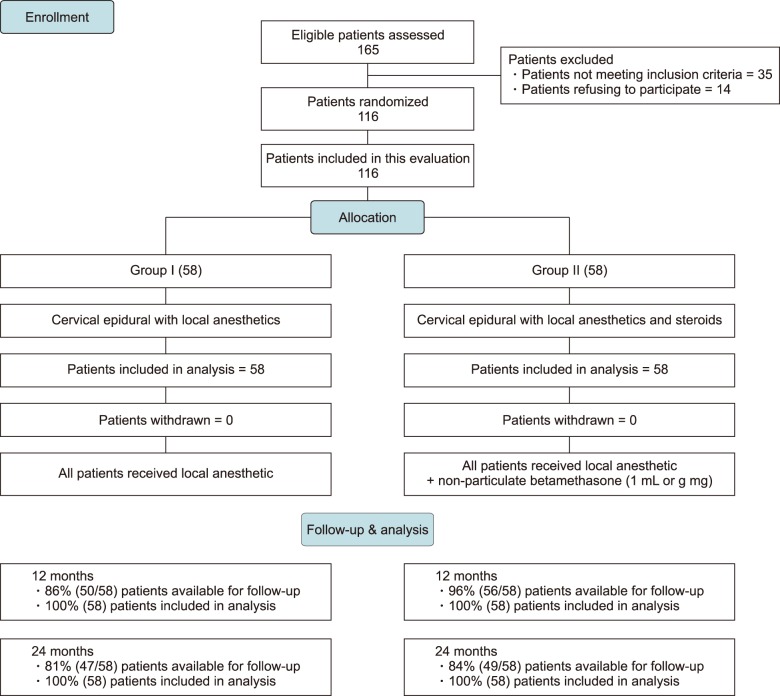
The effectiveness of fluoroscopic cervical interlaminar epidural injections in post-surgery syndrome was evaluated in a randomized, active controlled trial. The study population included 116 patients assigned to 2 groups. Group 1 received cervical interlaminar epidural injections with local anesthetic alone and Group 2 received injection with local anesthetic and steroids. The main outcomes were defined as significant improvement (greater than 50%) of pain relief using the numeric rating scale and/or functional status improvement using the Neck Disability Index (NDI).
RESULTS
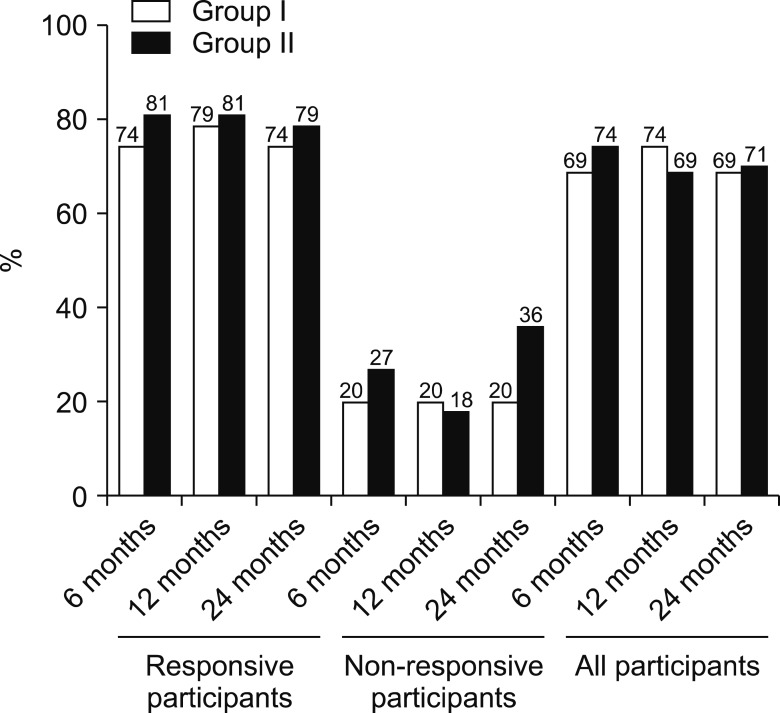
Both groups had similar results with significant improvement (≥ 50% pain relief and functional status improvement) in 69% of the patients in Group I, whereas, in Group II, 71% of the patients showed significant improvement at the end of 2 years. During a 2-year period, the average number of procedures was 5 to 6, with an average of approximately 12 weeks of significant improvement per procedure.
CONCLUSIONS
Fluoroscopic cervical interlaminar epidural injections administered in cervical post-surgery syndrome using local anesthetic, regardless of the use of steroids, may be effective in approximately 70% of the patients at 2-year follow-up.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Complications and safety of cervical interlaminar epidural block
Jae Hun Kim
Korean J Pain. 2024;37(3):185-187. doi: 10.3344/kjp.24186.
Reference
-
1. Nordin M, Randhawa K, Torres P, Yu H, Haldeman S, Brady O, et al. The global spine care initiative: a systematic review for the assessment of spine-related complaints in populations with limited resources and in low- and middle-income communities. Eur Spine J. 2018; [in press].
Article2. Dieleman JL, Baral R, Birger M, Bui AL, Bulchis A, Chapin A, et al. US spending on personal health care and public health, 1996–2013. JAMA. 2016; 316:2627–2646. PMID: 28027366.
Article3. Dieleman JL, Squires E, Bui AL, Campbell M, Chapin A, Hamavid H, et al. Factors associated with increase in US health care spending, 1996–2013. JAMA. 2017; 318:1668–1678. PMID: 29114831.
Article4. Murray CJ, Atkinson C, Bhalla K, Birbeck G, Burstein R, Chou D, et al. The state of US health, 1990–2010: burden of diseases, injuries, and risk factors. JAMA. 2013; 310:591–608. PMID: 23842577.5. Mokdad AH, Ballestros K, Echko M, Glenn S, Olsen HE, Mullany E, et al. The state of US health, 1990–2016: burden of diseases, injuries, and risk factors among US states. JAMA. 2018; 319:1444–1472. PMID: 29634829.6. Leboeuf-Yde C, Nielsen J, Kyvik KO, Fejer R, Hartvigsen J. Pain in the lumbar, thoracic or cervical regions: do age and gender matter? a population-based study of 34,902 Danish twins 20–71 years of age. BMC Musculoskelet Disord. 2009; 10:39. PMID: 19379477.
Article7. Hoy D, March L, Woolf A, Blyth F, Brooks P, Smith E, et al. The global burden of neck pain: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014; 73:1309–1315. PMID: 24482302.
Article8. Manchikanti L, Kaye AM, Knezevic NN, McAnally H, Slavin K, Trescot AM, et al. Responsible, safe, and effective prescription of opioids for chronic non-cancer pain: American society of interventional pain physicians (ASIPP) guidelines. Pain Physician. 2017; 20:S3–S92. PMID: 28226332.9. Manchikanti L, Pampati V, Hirsch JA. Utilization of interventional techniques in managing chronic pain in medicare population from 2000 to 2014: an analysis of patterns of utilization. Pain Physician. 2016; 19:E531–E546. PMID: 27228520.10. Manchikanti L, Soin A, Mann DP, Bakshi S, Pampati V, Hirsch JA. Reversal of growth of utilization of interventional techniques in managing chronic pain in medicare population post affordable care act. Pain Physician. 2017; 20:551–567. PMID: 29149139.11. Manchikanti L, Singh V, Hirsch JA. Facility payments for interventional pain management procedures: impact of proposed rules. Pain Physician. 2016; 19:E957–E984. PMID: 27676688.12. Manchikanti L, Kaye AD, Hirsch JA. Proposed medicare physician payment schedule for 2017: impact on interventional pain management practices. Pain Physician. 2016; 19:E935–E955. PMID: 27676687.13. Manchikanti L, Pampati V, Hirsch JA. Retrospective cohort study of usage patterns of epidural injections for spinal pain in the US fee-for-service Medicare population from 2000 to 2014. BMJ Open. 2016; 6:e013042.
Article14. Bakhsheshian J, Mehta VA, Liu JC. Current diagnosis and management of cervical spondylotic myelopathy. Global Spine J. 2017; 7:572–586. PMID: 28894688.
Article15. Derman PB, Lampe LP, Hughes AP, Pan TJ, Kueper J, Girardi FP, et al. Demographic, clinical, and operative factors affecting long-term revision rates after cervical spine arthrodesis. J Bone Joint Surg Am. 2016; 98:1533–1540. PMID: 27655980.
Article16. Gutman G, Rosenzweig DH, Golan JD. Surgical treatment of cervical radiculopathy: meta-analysis of randomized controlled trials. Spine (Phila Pa 1976). 2018; 43:E365–E372. PMID: 28700452.17. Patil PG, Turner DA, Pietrobon R. National trends in surgical procedures for degenerative cervical spine disease: 1990–2000. Neurosurgery. 2005; 57:753–758. PMID: 16239888.
Article18. Leavitt SB. NSAID dangers may limit pain-relief options. Pain-topics news/research updates [Internet];2010. cited 2010 Mar 14. Available at http://updates.pain-topics.org/2010/03/nsaid-dangers-may-limit-pain-relief.html.19. Moore A, Wiffen P, Kalso E. Antiepileptic drugs for neuropathic pain and fibromyalgia. JAMA. 2014; 312:182–183. PMID: 25005656.
Article20. Manchikanti L, Hirsch JA, Kaye AD, Boswell MV. Cervical zygapophysial (facet) joint pain: effectiveness of interventional management strategies. Postgrad Med. 2016; 128:54–68. PMID: 26653406.
Article21. Shamji MF, Cook C, Pietrobon R, Tackett S, Brown C, Isaacs RE. Impact of surgical approach on complications and resource utilization of cervical spine fusion: a nationwide perspective to the surgical treatment of diffuse cervical spondylosis. Spine J. 2009; 9:31–38. PMID: 18790678.
Article22. Manchikanti L, Malla Y, Cash KA, McManus CD, Pampati V. Fluoroscopic cervical interlaminar epidural injections in managing chronic pain of cervical postsurgery syndrome: preliminary results of a randomized, double-blind, active control trial. Pain Physician. 2012; 15:13–25. PMID: 22270734.23. Kaye AD, Manchikanti L, Abdi S, Atluri S, Bakshi S, Benyamin R, et al. Efficacy of epidural injections in managing chronic spinal pain: a best evidence synthesis. Pain Physician. 2015; 18:E939–E1004. PMID: 26606031.24. Manchikanti L, Knezevic NN, Boswell MV, Kaye AD, Hirsch JA. Epidural injections for lumbar radiculopathy and spinal stenosis: a comparative systematic review and meta-analysis. Pain Physician. 2016; 19:E365–E410. PMID: 27008296.25. Manchikanti L, Pampati V, Benyamin RM, Hirsch JA. Cost utility analysis of lumbar interlaminar epidural injections in the treatment of lumbar disc herniation, central spinal stenosis, and axial or discogenic low back pain. Pain Physician. 2017; 20:219–228. PMID: 28535546.26. Manchikanti L, Pampati V, Kaye AD, Hirsch JA. Therapeutic lumbar facet joint nerve blocks in the treatment of chronic low back pain: cost utility analysis based on a randomized controlled trial. Korean J Pain. 2018; 31:27–38. PMID: 29372023.
Article27. Manchikanti L, Pampati V, Kaye AD, Hirsch JA. Cost utility analysis of cervical therapeutic medial branch blocks in managing chronic neck pain. Int J Med Sci. 2017; 14:1307–1316. PMID: 29200944.
Article28. Cleland JA, Childs JD, Whitman JM. Psychometric properties of the neck disability index and numeric pain rating scale in patients with mechanical neck pain. Arch Phys Med Rehabil. 2008; 89:69–74. PMID: 18164333.
Article29. Browner WS, Newman TB, Cummings SR, Hulley SB. Estimating sample size and power. In : Hulley SB, Cummings SR, Browner WS, Grady D, Hearst N, Newman TB, editors. Designing clinical research: an epidemiologic approach. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins;2001. p. 65–84.30. Zhai J, Zhang L, Li M, Tian Y, Zheng W, Chen J, et al. Epidural injection with or without steroid in managing chronic low back and lower extremity pain: a meta-analysis of ten randomized controlled trials. Int J Clin Exp Med. 2015; 8:8304–8316. PMID: 26309483.31. Manchikanti L, Cash KA, Pampati V, Wargo BW, Malla Y. A randomized, double-blind, active control trial of fluoroscopic cervical interlaminar epidural injections in chronic pain of cervical disc herniation: results of a 2-year follow-up. Pain Physician. 2013; 16:465–478. PMID: 24077193.32. Manchikanti L, Cash KA, Pampati V, Malla Y. Two-year follow-up results of fluoroscopic cervical epidural injections in chronic axial or discogenic neck pain: a randomized, double-blind, controlled trial. Int J Med Sci. 2014; 11:309–320. PMID: 24578607.
Article33. Manchikanti L, Malla Y, Cash KA, McManus CD, Pampati V. Fluoroscopic epidural injections in cervical spinal stenosis: preliminary results of a randomized, double-blind, active control trial. Pain Physician. 2012; 15:E59–E70. PMID: 22270749.34. Manchikanti L, Cash KA, McManus CD, Pampati V, Fellows B. Results of 2-year follow-up of a randomized, double-blind, controlled trial of fluoroscopic caudal epidural injections in central spinal stenosis. Pain Physician. 2012; 15:371–384. PMID: 22996849.35. Manchikanti L, Singh V, Cash KA, Pampati V, Datta S. Fluoroscopic caudal epidural injections in managing post lumbar surgery syndrome: two-year results of a randomized, double-blind, active-control trial. Int J Med Sci. 2012; 9:582–591. PMID: 23028241.
Article36. Tunis SR, Stryer DB, Clancy CM. Practical clinical trials: increasing the value of clinical research for decision making in clinical and health policy. JAMA. 2003; 290:1624–1632. PMID: 14506122.37. Sherman RE, Anderson SA, Dal Pan GJ, Gray GW, Gross T, Hunter NL, et al. Real-world evidence - what is it and what can it tell us? N Engl J Med. 2016; 375:2293–2297. PMID: 27959688.
Article38. International conference on harmonisation of technical requirements for registration of pharmaceuticals for human use. ICH harmonised tripartite guideline. Choice of control group and related issues in clinical trials E10 [Internet]. Geneva: ICH Steering Committee;2000. cited 2018 May 9. Available at https://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E10/Step4/E10_Guideline.pdf.39. Pasqualucci A, Varrassi G, Braschi A, Peduto VA, Brunelli A, Marinangeli F, et al. Epidural local anesthetic plus corticosteroid for the treatment of cervical brachial radicular pain: single injection versus continuous infusion. Clin J Pain. 2007; 23:551–557. PMID: 17710003.
Article40. Tachihara H, Sekiguchi M, Kikuchi S, Konno S. Do corticosteroids produce additional benefit in nerve root infiltration for lumbar disc herniation? Spine (Phila Pa 1976). 2008; 33:743–747. PMID: 18379400.
Article41. Sato C, Sakai A, Ikeda Y, Suzuki H, Sakamoto A. The prolonged analgesic effect of epidural ropivacaine in a rat model of neuropathic pain. Anesth Analg. 2008; 106:313–320. PMID: 18165597.
Article42. Song T, Gu K, Wang W, Wang H, Yang Y, Yang L, et al. Prolonged suppression of neuropathic pain by sequential delivery of lidocaine and thalidomide drugs using PEGylated graphene oxide. J Pharm Sci. 2015; 104:3851–3860. PMID: 26220057.
Article43. Byröd G, Otani K, Brisby H, Rydevik B, Olmarker K. Methylprednisolone reduces the early vascular permeability increase in spinal nerve roots induced by epidural nucleus pulposus application. J Orthop Res. 2000; 18:983–987. PMID: 11192260.
Article44. Lee HM, Weinstein JN, Meller ST, Hayashi N, Spratt KF, Gebhart GF. The role of steroids and their effects on phospholipase A2. An animal model of radiculopathy. Spine (Phila Pa 1976). 1998; 23:1191–1196. PMID: 9636970.45. Hayashi N, Weinstein JN, Meller ST, Lee HM, Spratt KF, Gebhart GF. The effect of epidural injection of betamethasone or bupivacaine in a rat model of lumbar radiculopathy. Spine (Phila Pa 1976). 1998; 23:877–885. PMID: 9580954.
Article46. Pennypacker KR, Hong JS, McMillian MK. Implications of prolonged expression of Fos-related antigens. Trends Pharmacol Sci. 1995; 16:317–321. PMID: 7482997.
Article47. Johansson A, Hao J, Sjölund B. Local corticosteroid application blocks transmission in normal nociceptive C-fibres. Acta Anaesthesiol Scand. 1990; 34:335–338. PMID: 2167604.
Article48. Kawakami M, Weinstein JN, Chatani K, Spratt KF, Meller ST, Gebhart GF. Experimental lumbar radiculopathy. Behavioral and histologic changes in a model of radicular pain after spinal nerve root irritation with chromic gut ligatures in the rat. Spine (Phila Pa 1976). 1994; 19:1795–1802. PMID: 7973977.
Article49. Decosterd I, Woolf CJ. Spared nerve injury: an animal model of persistent peripheral neuropathic pain. Pain. 2000; 87:149–158. PMID: 10924808.
Article50. Norimoto M, Ohtori S, Yamashita M, Inoue G, Yamauchi K, Koshi T, et al. Direct application of the TNF-alpha inhibitor, etanercept, does not affect CGRP expression and phenotypic change of DRG neurons following application of nucleus pulposus onto injured sciatic nerves in rats. Spine (Phila Pa 1976). 2008; 33:2403–2408. PMID: 18824950.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Delayed Pneumocephalus Following Fluoroscopy Guided Cervical Interlaminar Epidural Steroid Injection: A Rare Complication and Anatomical Considerations
- Epidural Steroid Injection in the Treatment of Cervical Radiculopathy
- Management of Cervical Radiculopathy with Epidural Steroid Injection
- Cervical Interlaminar Epidural Steroid Injection for Unilateral Cervical Radiculopathy: Comparison of Midline and Paramedian Approaches for Efficacy
- A Comparison of the Spread Level of the Cervical Epidural Block in Terms of Volume