J Korean Neurosurg Soc.
2018 Sep;61(5):574-581. 10.3340/jkns.2018.0090.
Can the Zero-Profile Implant Be Used for Anterior Cervical Discectomy and Fusion in Traumatic Subaxial Disc Injury? A Preliminary, Retrospective Study
- Affiliations
-
- 1Department of Neurosurgery, Daegu Catholic University Medical Center, Catholic University of Daegu College of Medicine, Daegu, Korea. spinechoi@cu.ac.kr
- 2Department of Medical Statistics, Daegu Catholic University Medical Center, Catholic University of Daegu College of Medicine, Daegu, Korea.
- KMID: 2420065
- DOI: http://doi.org/10.3340/jkns.2018.0090
Abstract
OBJECTIVE
The zero-profile implant (Zero-P) is accepted for use in anterior cervical fusion for the treatment of degenerative cervical disease. However, evidence pertaining to its efficiency and safety in traumatic cervical injury is largely insufficient. This study aimed to compare the overall outcomes of patients who underwent Zero-P for traumatic cervical disc injury.
METHODS
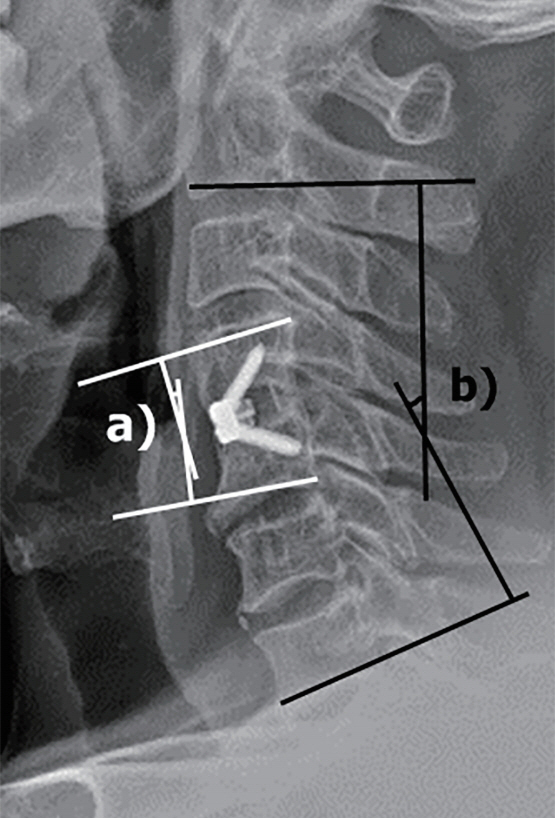
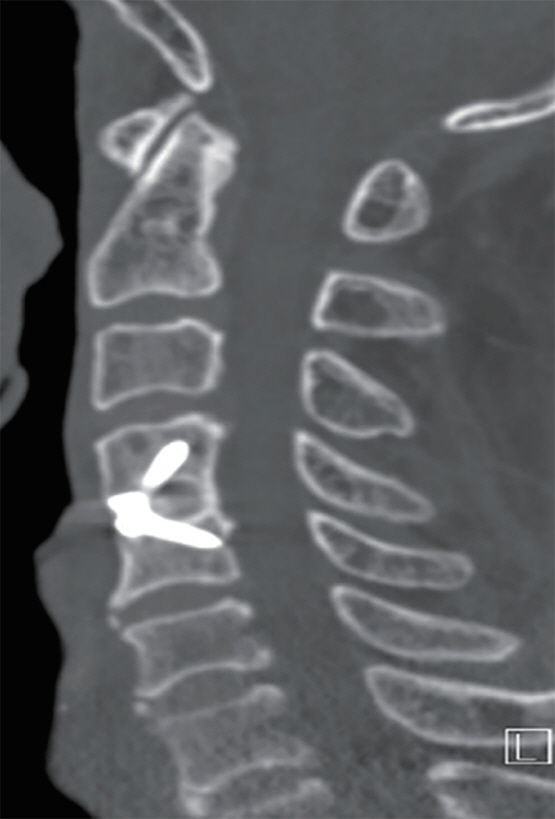
Data from a total of 53 consecutive patients who underwent surgery for traumatic or degenerative cervical disc disease using the Zero-P were reviewed. Seventeen patients (group A) had traumatic cervical disc injury and the remaining 36 (group B) had degenerative cervical disc herniation. The fusion and subsidence rates and Cobb angle were measured retrospectively from plain radiographs. The patients' clinical outcomes were evaluated using the Japanese Orthopedic Association (JOA) score and Odom's criteria.
RESULTS
The C2-7 Cobb and operative segmental angles increased by 3.45±7.61 and 2.94±4.59 in group A; and 2.46±7.31 and 2.88±5.49 in group B over 12 postoperative months, respectively. The subsidence and fusion rate was 35.0% and 95.0% in group A; and 36.6% and 95.1% in group B, respectively. None of the parameters differed significantly between groups. The clinical outcomes were similar in both groups in terms of increasing the JOA score and producing a grade higher than "good" using Odom's criteria.
CONCLUSION
The application of Zero-P in patients with traumatic cervical disc injury was found to be acceptable when compared with the clinical and radiological outcomes of degenerative cervical spondylosis.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Aebi M. Surgical treatment of upper, middle and lower cervical injuries and non-unions by anterior procedures. Eur Spine J 19 Suppl. 1:S33–S39. 2010.
Article2. Barbagallo GM, Romano D, Certo F, Milone P, Albanese V. Zero-P: a new zero-profile cage-plate device for single and multilevel ACDF. A single institution series with four years maximum follow-up and review of the literature on zero-profile devices. Eur Spine J 22 Suppl. 6:S868–S878. 2013.
Article3. Brembilla C, Lanterna LA, Gritti P, Signorelli A, Biroli F. The use of a stand-alone interbody fusion cage in subaxial cervical spine trauma: a preliminary report. J Neurol Surg A Cent Eur Neurosurg. 76:13–19. 2015.
Article4. Cho HJ, Hur JW, Lee JB, Han JS, Cho TH, Park JY. Cervical stand-alone polyetheretherketone cage versus zero-profile anchored spacer in singlelevel anterior cervical discectomy and fusion : minimum 2-year assessment of radiographic and clinical outcome. J Korean Neurosurg Soc. 58:119–124. 2015.
Article5. Choi MK, Kim SB, Park CK, Kim SM. Comparison of the clinical and radiologic outcomes obtained with single- versus two-level anterior cervical decompression and fusion using stand-alone PEEK cages filled with allograft. Acta Neurochir (Wien). 158:481–487. 2016.
Article6. Choi MK, Kim SB, Park CK, Lee SH, Jo DJ. Relation of deep paraspinal muscles’ cross-sectional area of the cervical spine and bone union in anterior cervical decompression and fusion: a retrospective study. World Neurosurg. 96:91–100. 2016.
Article7. Glaser JA, Jaworski BA, Cuddy BG, Albert TJ, Hollowell JP, McLain RF, et al. Variation in surgical opinion regarding management of selected cervical spine injuries. A preliminary study. Spine (Phila Pa 1976). 23:975–982. discussion 983. 1998.
Article8. Halani SH, Baum GR, Riley JP, Pradilla G, Refai D, Rodts GE Jr, et al. Esophageal perforation after anterior cervical spine surgery: a systematic review of the literature. J Neurosurg Spine. 25:285–291. 2016.
Article9. Kaiser MG, Haid RW Jr, Subach BR, Barnes B, Rodts GE Jr. Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery. 50:229–236. discussion 236-238. 2002.
Article10. Lowery GL, McDonough RF. The significance of hardware failure in anterior cervical plate fixation. Patients with 2- to 7-year follow-up. Spine (Phila Pa 1976). 23:181–186. discussion 186-187. 1998.
Article11. Njoku I Jr, Alimi M, Leng LZ, Shin BJ, James AR, Bhangoo S, et al. Anterior cervical discectomy and fusion with a zero-profile integrated plate and spacer device: a clinical and radiological study: clinical article. J Neurosurg Spine. 21:529–537. 2014.
Article12. Odom GL, Finney W, Woodhall B. Cervical disk lesions. J Am Med Assoc. 166:23–28. 1958.
Article13. Scholz M, Reyes PM, Schleicher P, Sawa AG, Baek S, Kandziora F, et al. A new stand-alone cervical anterior interbody fusion device: biomechanical comparison with established anterior cervical fixation devices. Spine (Phila Pa 1976). 34:156–160. 2009.14. Shao H, Chen J, Ru B, Yan F, Zhang J, Xu S, et al. Zero-profile implant versus conventional cage-plate implant in anterior cervical discectomy and fusion for the treatment of degenerative cervical spondylosis: a meta-analysis. J Orthop Surg Res. 10:148. 2015.
Article15. Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 40-A:607–624. 1958.
Article16. Son DK, Son DW, Kim HS, Sung SK, Lee SW, Song GS. Comparative study of clinical and radiological outcomes of a zero-profile device concerning reduced postoperative Dysphagia after single level anterior cervical discectomy and fusion. J Korean Neurosurg Soc. 56:103–107. 2014.
Article17. Song KS, Piyaskulkaew C, Chuntarapas T, Buchowski JM, Kim HJ, Park MS, et al. Dynamic radiographic criteria for detecting pseudarthrosis following anterior cervical arthrodesis. J Bone Joint Surg Am. 96:557–563. 2014.
Article18. Wang T, Ma L, Yang DL, Wang H, Bai ZL, Zhang LJ, et al. Factors predicting dysphagia after anterior cervical surgery: a multicenter retrospective study for 2 years of follow-up. Medicine (Baltimore). 96:e7916. 2017.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anterior Cervical Discectomy
- Clinical Results of Anterior Cervical Discectomy and Fusion with Prefilled Cage in Patient with Traumatic Cervical Injury
- Analysis of Posterior Cervical Fixation and Fusion in Subaxial Cervical Spine Injury
- Outcomes of Unstable Subaxial Cervical Spine Fractures Managed by Posteroanterior Stabilization and Fusion
- A Prospective Study of Clinical and Radiological Outcomes of Zero-Profile Cage Screw Implants for Single-Level Anterior Cervical Discectomy and Fusion: Is Segmental Lordosis Maintained at 2 Years?