Ann Rehabil Med.
2018 Aug;42(4):584-590. 10.5535/arm.2018.42.4.584.
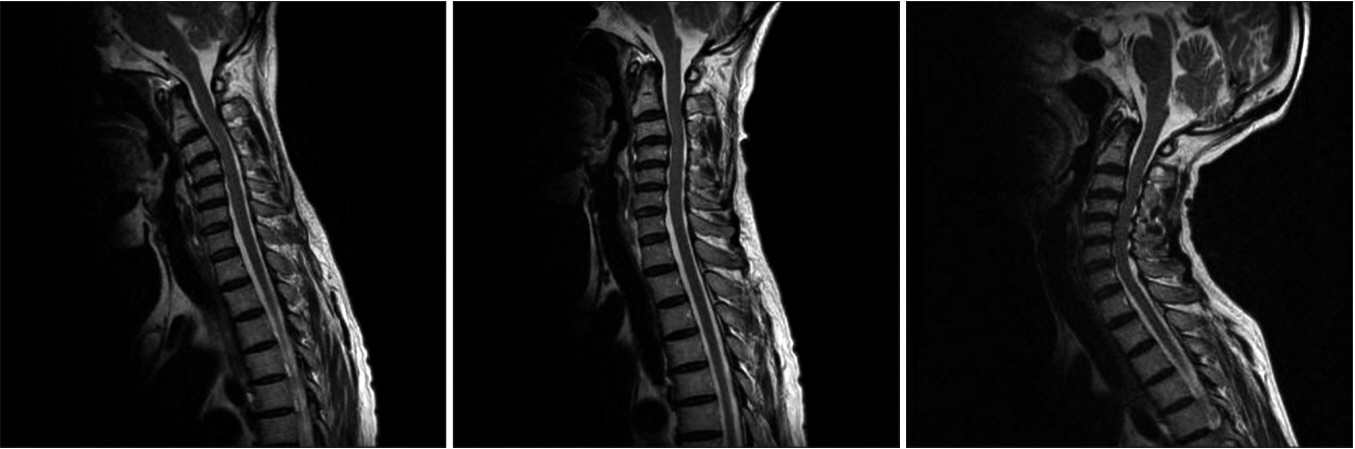
A Dynamic Magnetic Resonance Imaging Study of Changes in Severity of Cervical Spinal Stenosis in Flexion and Extension
- Affiliations
-
- 1Department of Rehabilitation Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. keewonkimm.d@gmail.com
- KMID: 2420051
- DOI: http://doi.org/10.5535/arm.2018.42.4.584
Abstract
OBJECTIVE
To evaluate changes in the severity of cervical spinal stenosis (CSS) in flexion and extension and determine whether the rate of change with motion varied with severity.
METHODS
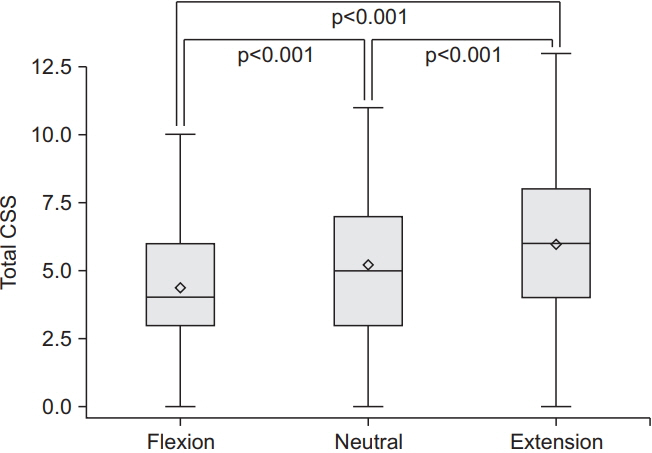
The study included 92 symptomatic patients with a mean age of 57.80±10.41, who underwent cervical spine dynamic magnetic resonance imaging. The severity of stenosis was evaluated using a semi-quantitative CSS score, ranging from 0 (no spinal stenosis) to 18 (severe stenosis). Radiological evaluation included flexion, neutral, and extension measurements, as determined by the C2-C7 Cobb angle. The severity of stenosis was represented by the total CSS score. The total CSS score in flexion, neutral, and extension positions was compared using repeated measures one-way analysis of variance. The change rate of stenosis per angle motion (CRSPAM) was defined as change in total CSS score divided by change in Cobb angle. The correlation of CRSPAM with severity of stenosis, represented by total CSS score in neutral position, was evaluated using Pearson correlation analysis.
RESULTS
The total CSS score was significantly higher in extension (6.04±2.68) than in neutral position (5.25±2.47) (p < 0.001), and significantly higher in neutral than in flexion position (4.40±2.45) (p < 0.001). The CRSPAM was significantly and positively correlated with total CSS score in neutral position in the flexion-extension range (r=0.22, p=0.04) and flexion-neutral range (r=0.27, p=0.01).
CONCLUSION
In symptomatic CSS patients, the radiological severity of stenosis increases with extension and decreases with flexion. In patients with CSS, the rate of variation in spinal stenosis increases with increased severity.
Keyword
MeSH Terms
Figure
Reference
-
1. Baptiste DC, Fehlings MG. Pathophysiology of cervical myelopathy. Spine J. 2006; 6(6 Suppl):190S–7S.
Article2. Lebl DR, Bono CM. Update on the diagnosis and management of cervical spondylotic myelopathy. J Am Acad Orthop Surg. 2015; 23:648–60.
Article3. Toledano M, Bartleson JD. Cervical spondylotic myelopathy. Neurol Clin. 2013; 31:287–305.
Article4. Muhle C, Weinert D, Falliner A, Wiskirchen J, Metzner J, Baumer M, et al. Dynamic changes of the spinal canal in patients with cervical spondylosis at flexion and extension using magnetic resonance imaging. Invest Radiol. 1998; 33:444–9.
Article5. Chen CJ, Hsu HL, Niu CC, Chen TY, Chen MC, Tseng YC, et al. Cervical degenerative disease at flexionextension MR imaging: prediction criteria. Radiology. 2003; 227:136–42.
Article6. Hayashi T, Wang JC, Suzuki A, Takahashi S, Scott TP, Phan K, et al. Risk factors for missed dynamic canal stenosis in the cervical spine. Spine (Phila Pa 1976). 2014; 39:812–9.
Article7. Lao L, Daubs MD, Scott TP, Phan KH, Wang JC. Missed cervical disc bulges diagnosed with kinematic magnetic resonance imaging. Eur Spine J. 2014; 23:1725–9.
Article8. Kim YH, Kim SI, Park S, Hong SH, Chung SG. Effects of cervical extension on deformation of intervertebral disk and migration of nucleus pulposus. PM R. 2017; 9:329–38.
Article9. Muhle C, Metzner J, Weinert D, Falliner A, Brinkmann G, Mehdorn MH, et al. Classification system based on kinematic MR imaging in cervical spondylitic myelopathy. AJNR Am J Neuroradiol. 1998; 19:1763–71.10. Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976). 2001; 26:1873–8.
Article11. Kang Y, Lee JW, Koh YH, Hur S, Kim SJ, Chai JW, et al. New MRI grading system for the cervical canal stenosis. AJR Am J Roentgenol. 2011; 197:W134–40.
Article12. Ohara A, Miyamoto K, Naganawa T, Matsumoto K, Shimizu K. Reliabilities of and correlations among five standard methods of assessing the sagittal alignment of the cervical spine. Spine (Phila Pa 1976). 2006; 31:2585–91.
Article13. Scannell JP, McGill SM. Disc prolapse: evidence of reversal with repeated extension. Spine (Phila Pa 1976). 2009; 34:344–50.14. Adams MA, Roughley PJ. What is intervertebral disc degeneration, and what causes it? Spine (Phila Pa 1976). 2006; 31:2151–61.
Article15. Tracy JA, Bartleson JD. Cervical spondylotic myelopathy. Neurologist. 2010; 16:176–87.
Article16. Sayit E, Daubs MD, Aghdasi B, Montgomery SR, Inoue H, Wang CJ, et al. Dynamic changes of the ligamentum flavum in the cervical spine assessed with kinetic magnetic resonance imaging. Global Spine J. 2013; 3:69–74.
Article17. Lebl DR, Hughes A, Cammisa FP Jr, O’Leary PF. Cervical spondylotic myelopathy: pathophysiology, clinical presentation, and treatment. HSS J. 2011; 7:170–8.
Article18. Morishita Y, Hida S, Miyazaki M, Hong SW, Zou J, Wei F, et al. The effects of the degenerative changes in the functional spinal unit on the kinematics of the cervical spine. Spine (Phila Pa 1976). 2008; 33:E178–82.
Article19. Miyazaki M, Hymanson HJ, Morishita Y, He W, Zhang H, Wu G, et al. Kinematic analysis of the relationship between sagittal alignment and disc degeneration in the cervical spine. Spine (Phila Pa 1976). 2008; 33:E870–6.
Article20. Clare HA, Adams R, Maher CG. A systematic review of efficacy of McKenzie therapy for spinal pain. Aust J Physiother. 2004; 50:209–16.
Article21. Ball JM, Cagle P, Johnson BE, Lucasey C, Lukert BP. Spinal extension exercises prevent natural progression of kyphosis. Osteoporos Int. 2009; 20:481–9.
Article22. Shedid D, Benzel EC. Cervical spondylosis anatomy: pathophysiology and biomechanics. Neurosurgery. 2007; 60(1 Supp1 1):S7–13.23. Machino M, Yukawa Y, Imagama S, Ito K, Katayama Y, Matsumoto T, et al. Age-related and degenerative changes in the osseous anatomy, alignment, and range of motion of the cervical spine: a comparative study of radiographic data from 1016 patients with cervical spondylotic myelopathy and 1230 asymptomatic subjects. Spine (Phila Pa 1976). 2016; 41:476–82.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Influence of Changes in Cervical Lordosis on Bulging Disk and Spinal Stenosis: Functional MR Imaging
- Efficacy of Dynamic Radiographs in Routine Evaluations for Degenerative Cervical Spine Disease
- Dynamic Cord Compression Causing Cervical Myelopathy
- Utility of cervical dynamic magnetic resonance imaging for evaluating patients with cervical myelopathy: a retrospective study
- Kinematic Analysis of the Cervical Cord and Cervical Canal by Dynamic Neck Motion