Ann Rehabil Med.
2018 Aug;42(4):551-559. 10.5535/arm.2018.42.4.551.
Influence of Nasogastric Tubes on Swallowing in Stroke Patients: Measuring Hyoid Bone Movement With Ultrasonography
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Sahmyook Medical Center, Seoul, Korea. wookster8888@gmail.com
- KMID: 2420047
- DOI: http://doi.org/10.5535/arm.2018.42.4.551
Abstract
OBJECTIVE
To investigate the influence of a nasogastric tube (NGT) on swallowing simulated saliva in stroke patients.
METHODS
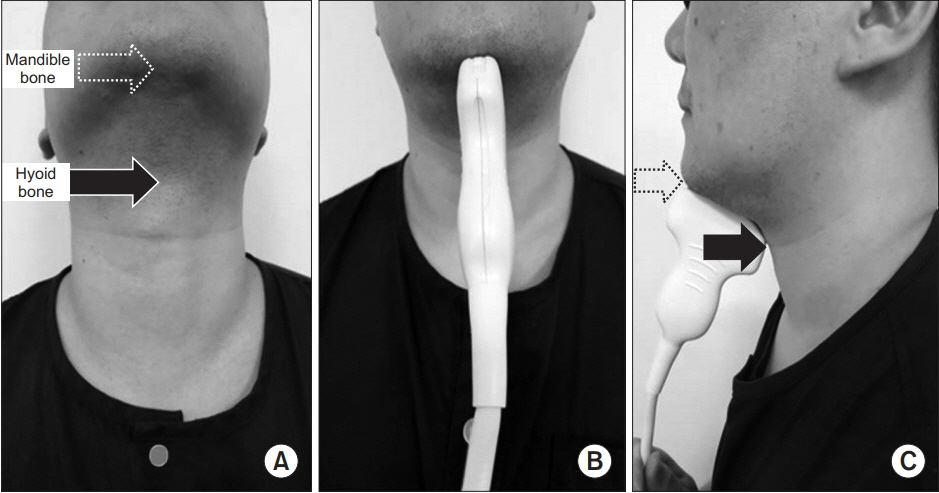
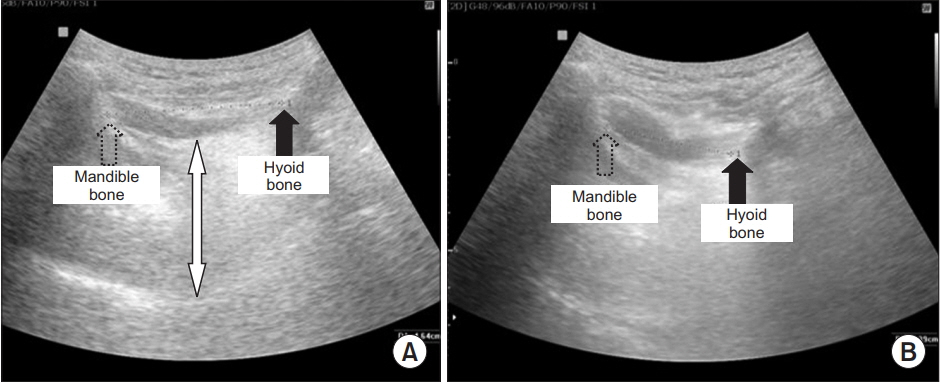
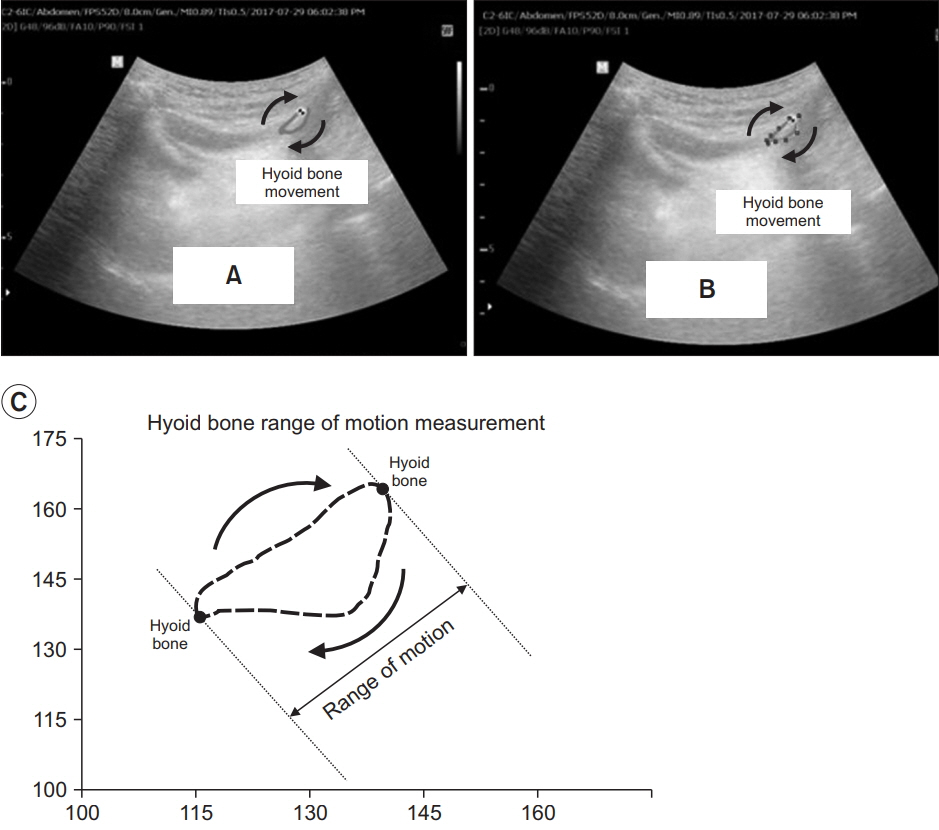
Three groups of participants were enrolled into the study: group A (20 stroke patients with a NGT), a control group B (25 stroke patients without a NGT), and group C (25 healthy adults with no brain lesions or dysphagia). Participants swallowed 1 mL of water to simulate saliva. Patients in group A were tested twice: once with a NGT (group A1) and once after the NGT was removed (group A2). The distance of hyoid bone movement was measured by subtracting the shortest distance between the mandible and hyoid bone (S) from the distance at resting state (R) measured with ultrasonography. The degree of the movement was calculated by (R-S)/R. The trajectory area of hyoid bone movement (Area) and the interval between the beginning of hyoid bone movement and the moment of the shortest hyoid−mandible approximation (Interval) was calculated by a computer program.
RESULTS
From group A: R-S and (R-S)/R of group A2 at 1.14±0.36 cm and 0.30±0.09 cm and were significantly greater than those of group A1 at 0.81±0.36 cm and 0.22±0.08 cm (p=0.009 and p=0.005). After removing the NGT as seen in group A2, R-S and (R-S)/R were improved to the level of those of group B at 1.20±0.32 cm and 0.30±0.09 cm (p=0.909 and p=0.997). The Area of group A2 was larger and the Interval of group A2 was shorter than those of group A1 though a comparison of these factors between A2 and A1 did not show a statistically significant difference.
CONCLUSION
A NGT interferes with the movement of the hyoid bone when swallowing 1 mL of water in stroke patients though the movement is restored to normal after removing the NGT.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Epiglottic Retroflexion is a Key Indicator of Functional Recovery of Post-stroke Dysphagia
Ji Soo Choi, Hyun Bang, Goo Joo Lee, Han Gil Seo, Byung-Mo Oh, Tai Ryoon Han
Ann Rehabil Med. 2020;44(1):1-10. doi: 10.5535/arm.2020.44.1.1.
Reference
-
1. Daniels SK, Ballo LA, Mahoney MC, Foundas AL. Clinical predictors of dysphagia and aspiration risk: outcome measures in acute stroke patients. Arch Phys Med Rehabil. 2000; 81:1030–3.
Article2. Finestone HM, Greene-Finestone LS, Wilson ES, Teasell RW. Malnutrition in stroke patients on the rehabilitation service and at follow-up: prevalence and predictors. Arch Phys Med Rehabil. 1995; 76:310–6.
Article3. Behrens R, Lang T, Muschweck H, Richter T, Hofbeck M. Percutaneous endoscopic gastrostomy in children and adolescents. J Pediatr Gastroenterol Nutr. 1997; 25:487–91.
Article4. Rosenvinge SK, Starke ID. Improving care for patients with dysphagia. Age Ageing. 2005; 34:587–93.
Article5. Hayes JC. Current feeding policies for patients with stroke. Br J Nurs. 1998; 7:580–8.6. Kim MH, Kim YH, Kim YM, Ju YH, Lee YM, Chung EH. A study on the applying of training program to facilitate deglution: on spontaneous intracerebral hemorrhage patients with nasogastric tube. J Korean Acad Adult Nurs. 2001; 13:136–47.7. Geeganage C, Beavan J, Ellender S, Bath PM. Interventions for dysphagia and nutritional support in acute and subacute stroke. Cochrane Database Syst Rev. 2012; 10:CD000323.
Article8. Ishida R, Palmer JB, Hiiemae KM. Hyoid motion during swallowing: factors affecting forward and upward displacement. Dysphagia. 2002; 17:262–72.
Article9. Logemann JA, Kahrilas PJ, Cheng J, Pauloski BR, Gibbons PJ, Rademaker AW, et al. Closure mechanisms of laryngeal vestibule during swallow. Am J Physiol. 1992; 262(2 Pt 1):G338–44.
Article10. Hsiao MY, Chang YC, Chen WS, Chang HY, Wang TG. Application of ultrasonography in assessing oropharyngeal dysphagia in stroke patients. Ultrasound Med Biol. 2012; 38:1522–8.
Article11. Chen YC, Hsiao MY, Wang YC, Fu CP, Wang TG. Reliability of ultrasonography in evaluating hyoid bone movement. J Med Ultrasound. 2017; 25:90–5.
Article12. Morgan A, Ward E, Murdoch B, Bilbie K. Acute characteristics of pediatric dysphagia subsequent to traumatic brain injury: videofluoroscopic assessment. J Head Trauma Rehabil. 2002; 17:220–41.13. Shin HY, Lee JY, Song J, Lee S, Lee J, Lim B, et al. Causeof-death statistics in the Republic of Korea, 2014. J Korean Med Assoc. 2016; 59:221–32.
Article14. Ring H, Feder M, Schwartz J, Samuels G. Functional measures of first-stroke rehabilitation inpatients: usefulness of the Functional Independence Measure total score with a clinical rationale. Arch Phys Med Rehabil. 1997; 78:630–5.
Article15. Huggins PS, Tuomi SK, Young C. Effects of nasogastric tubes on the young, normal swallowing mechanism. Dysphagia. 1999; 14:157–61.
Article16. Robbins J, Hamilton JW, Lof GL, Kempster GB. Oropharyngeal swallowing in normal adults of different ages. Gastroenterology. 1992; 103:823–9.
Article17. Robbins JA. The impact of oral motor dysfunction on swallowing: from beginning to end. Semin Speech Lang. 1992; 13:55–69.
Article18. Macrae PR, Doeltgen SH, Jones RD, Huckabee ML. Intra- and inter-rater reliability for analysis of hyoid displacement measured with sonography. J Clin Ultrasound. 2012; 40:74–8.
Article19. Huang YL, Hsieh SF, Chang YC, Chen HC, Wang TG. Ultrasonographic evaluation of hyoid-larynx approximation in dysphagic stroke patients. Ultrasound Med Biol. 2009; 35:1103–8.
Article20. Shawker TH, Sonies B, Hall TE, Baum BF. Ultrasound analysis of tongue, hyoid, and larynx activity during swallowing. Invest Radiol. 1984; 19:82–6.
Article21. Yabunaka K, Sanada H, Sanada S, Konishi H, Hashimoto T, Yatake H, et al. Sonographic assessment of hyoid bone movement during swallowing: a study of normal adults with advancing age. Radiol Phys Technol. 2011; 4:73–7.
Article22. Fanucci A, Cerro P, Ietto F, Brancaleone C, Berardi F. Physiology of oral swallowing studied by ultrasonography. Dentomaxillofac Radiol. 1994; 23:221–5.
Article23. Kuhl V, Eicke BM, Dieterich M, Urban PP. Sonographic analysis of laryngeal elevation during swallowing. J Neurol. 2003; 250:333–7.
Article24. Dziewas R, Warnecke T, Hamacher C, Oelenberg S, Teismann I, Kraemer C, et al. Do nasogastric tubes worsen dysphagia in patients with acute stroke? BMC Neurol. 2008; 8:28.
Article25. Gomes GF, Pisani JC, Macedo ED, Campos AC. The nasogastric feeding tube as a risk factor for aspiration and aspiration pneumonia. Curr Opin Clin Nutr Metab Care. 2003; 6:327–33.
Article26. Rahnemai-Azar AA, Rahnemaiazar AA, Naghshizadian R, Kurtz A, Farkas DT. Percutaneous endoscopic gastrostomy: indications, technique, complications and management. World J Gastroenterol. 2014; 20:7739–51.
Article27. Paik NJ, Kim SJ, Lee HJ, Jeon JY, Lim JY, Han TR. Movement of the hyoid bone and the epiglottis during swallowing in patients with dysphagia from different etiologies. J Electromyogr Kinesiol. 2008; 18:329–35.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Influence of Nasogastric Tubes on Swallowing Function in Stroke Patient with Dysphagia
- Effect of Decannulation on Pharyngeal and Laryngeal Movement in Post-Stroke Tracheostomized Patients
- Digital Image Motion Analysis of the Pharyngeal Movement during Swallowing in Dysphagia Patients
- Usefulness of Submental Ultrasonographic Evaluation for Dysphagia Patients
- The Effect of Nasogastric Tube on Swallowing Function in Stroke Patients with Dysphagia