Ann Dermatol.
2018 Oct;30(5):588-591. 10.5021/ad.2018.30.5.588.
Piperacillin-Tazobactam-Induced Linear IgA Bullous Dermatosis Supported by a T-Cell Activation Assay
- Affiliations
-
- 1Department of Dermatology, Taipei Veterans General Hospital, Taipei, Taiwan. hnliu@vghtpe.gov.tw
- 2Department of Dermatology, National Yang-Ming University, Taipei, Taiwan.
- 3Department of Dermatology, National Defense Medical Center, Taipei, Taiwan.
- KMID: 2419750
- DOI: http://doi.org/10.5021/ad.2018.30.5.588
Abstract
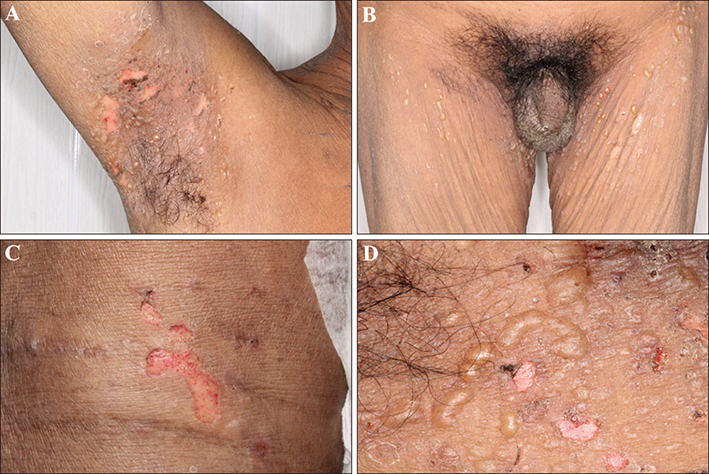
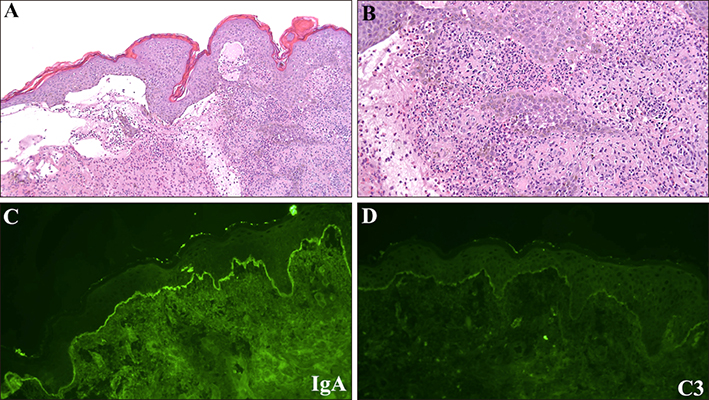
- Linear immunoglobulin (Ig) A bullous dermatosis (LABD) is a rare subepidermal autoimmune blistering disease characterized by linear IgA deposits at the basement membrane zone visualized with direct immunofluorescence (DIF). Most cases of LABD are idiopathic, but some are drug-induced with vancomycin being the most common causative agent. We herein report a patient presenting with blisters and erosive lesions, primarily in the intertriginous and flexor areas, consistent with a diagnosis of piperacillin-tazobactam-induced LABD based on the patient's clinical course and histopathology, DIF, and in vitro T-cell activation assay (TAA) findings. Only one case of piperacillin-tazobactam-induced LABD has been previously reported. In addition to its rarity, our case was also unique in that the skin lesions occurred in the intertriginous and flexor areas, uncommon locations for typical adult patients with LABD, and TAA strongly suggested an association with the causative drug.
MeSH Terms
Figure
Reference
-
1. Adler NR, McLean CA, Aung AK, Goh MS. Piperacillin-tazobactam-induced linear IgA bullous dermatosis presenting clinically as Stevens-Johnson syndrome/toxic epidermal necrolysis overlap. Clin Exp Dermatol. 2017; 42:299–302.
Article2. Fortuna G, Marinkovich MP. Linear immunoglobulin A bullous dermatosis. Clin Dermatol. 2012; 30:38–50.
Article3. Sakka N, Yahia KH, Volcon A, Brazilai A, Baum S. Intertriginous linear iga bullous dermatosis treated with colchicine. J Dermatol Clin Res. 2015; 3:1040.4. Lings K, Bygum A. Linear IgA bullous dermatosis: a retrospective study of 23 patients in Denmark. Acta Derm Venereol. 2015; 95:466–471.
Article5. Jha P, Swanson K, Stromich J, Michalski BM, Olasz E. A rare case of vancomycin-induced linear immunoglobulin A bullous dermatosis. Case Rep Dermatol Med. 2017; 2017:7318305.
Article6. Tomida E, Kato Y, Ozawa H, Hasegawa H, Ishii N, Hashimoto T, et al. Causative drug detection by drug-induced lymphocyte stimulation test in drug-induced linear IgA bullous dermatosis. Br J Dermatol. 2016; 175:1106–1108.
Article7. Chung WH, Hung SI, Yang JY, Su SC, Huang SP, Wei CY, et al. Granulysin is a key mediator for disseminated keratinocyte death in Stevens-Johnson syndrome and toxic epidermal necrolysis. Nat Med. 2008; 14:1343–1350.
Article8. Chung WH, Pan RY, Chu MT, Chin SW, Huang YL, Wang WC, et al. Oxypurinol-specific T cells possess preferential TCR clonotypes and express granulysin in allopurinol-induced severe cutaneous adverse reactions. J Invest Dermatol. 2015; 135:2237–2248.
Article9. Porębski G, Czarnobilska E, Bosak M. Cytotoxic-based assays in delayed drug hypersensitivity reactions induced by antiepileptic drugs. Pol Arch Med Wewn. 2015; 125:823–834.
Article10. Porebski G, Pecaric-Petkovic T, Groux-Keller M, Bosak M, Kawabata TT, Pichler WJ. In vitro drug causality assessment in Stevens-Johnson syndrome - alternatives for lymphocyte transformation test. Clin Exp Allergy. 2013; 43:1027–1037.
Article11. Schrijvers R, Gilissen L, Chiriac AM, Demoly P. Pathogenesis and diagnosis of delayed-type drug hypersensitivity reactions, from bedside to bench and back. Clin Transl Allergy. 2015; 5:31.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Vancomycin-induced Linear IgA Bullous Dermatosis
- A Case of Fulminant Linear IgA Bullous Dermatosis in an adult
- Vancomycin-induced Linear IgA Bullous Dermatosis: A Case Report and Review of the Literature
- A case of Linear IgA Bullous Dermatosis Probably Caused by Vancomycin
- A case of drug - induced linear IgA bullous dermatosis