Effect of Early Plasma Exchange on Survival in Patients with Severe Fever with Thrombocytopenia Syndrome: A Multicenter Study
- Affiliations
-
- 1Department of Internal Medicine, Kangwon National University School of Medicine, Chuncheon, Korea.
- 2Department of Internal Medicine, Jeju National University School of Medicine, Jeju, Korea. neosangtaek@naver.com
- 3Department of Internal Medicine, Daegu Fatima Hospital, Deagu, Korea.
- 4Department of Internal Medicine, Pusan National University Yangsan Hospital, Yangsan, Korea.
- 5Department of Internal Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea.
- 6Department of Internal Medicine, Keimyung University Dongsan Medical Center, Daegu, Korea.
- 7Department of Internal Medicine, Yeungnam University College of Medicine, Daegu, Korea.
- 8Department of Internal Medicine, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea.
- 9Department of Internal Medicine, Changwon Fatima Hospital, Changwon, Korea.
- KMID: 2419096
- DOI: http://doi.org/10.3349/ymj.2017.58.4.867
Abstract
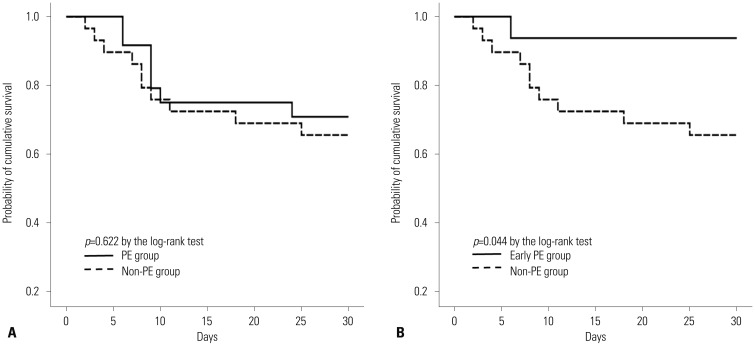
- Despite a high mortality rate, no specific treatment for severe fever with thrombocytopenia syndrome (SFTS) has been established. This study compared the clinical outcomes of SFTS patients treated with plasma exchange (PE group) with those who were not treated (non-PE group) at nine Korean hospitals between May 2013 and August 2015. A total of 53 SFTS patients were included: 24 (45.3%) PE cases and 29 (54.7%) non-PE cases. The overall in-hospital mortality rate was 32.1% (17/53). The in-hospital mortality rate of the PE group did not differ from that of the non-PE group (29.3% vs. 34.5%, p=0.680). Of the 24 PE cases, 16 (66.7%) were treated with PE within 7 days of symptom onset (early PE group). The early PE group survived longer than the non-PE group (mean 28.4 days vs. 22.6 days, p=0.044). Multivariate analysis showed an inverse association between early PE implementation and 30-day mortality (adjusted hazard ratio 0.052, 95% confidence interval 0.004-0.678, p=0.024). The results of this study suggest that early PE implementation may have a beneficial effect on the clinical outcome of SFTS patients.
MeSH Terms
Figure
Cited by 4 articles
-
Severe Fever with Thrombocytopenia Syndrome Patients with Hemophagocytic Lymphohistiocytosis Retrospectively Identified in Korea, 2008–2013
Kye-Hyung Kim, Myung Jin Lee, Mee Kyung Ko, Eun Yup Lee, Jongyoun Yi
J Korean Med Sci. 2018;33(50):. doi: 10.3346/jkms.2018.33.e319.Systems Biology-Based Platforms to Accelerate Research of Emerging Infectious Diseases
Soo-Jin Oh, Young-Ki Choi, Ok Sarah Shin
Yonsei Med J. 2018;59(2):176-186. doi: 10.3349/ymj.2018.59.2.176.Higher Fatality for Severe Fever with Thrombocytopenia Syndrome Complicated by Hemophagocytic Lymphohistiocytosis
In Young Jung, Kwangjin Ahn, Juwon Kim, Jun Yong Choi, Hyo Youl Kim, Young Uh, Young Keun Kim
Yonsei Med J. 2019;60(6):592-596. doi: 10.3349/ymj.2019.60.6.592.Proposal of the Need for New Korean Guidelines on the Use of Therapeutic Apheresis in Clinical Practice
Yousun Chung, Hyungsuk Kim, Dae-Hyun Ko
Ann Lab Med. 2022;42(6):703-707. doi: 10.3343/alm.2022.42.6.703.
Reference
-
1. Li DX. Severe fever with thrombocytopenia syndrome: a newly discovered emerging infectious disease. Clin Microbiol Infect. 2015; 21:614–620. PMID: 25769426.
Article2. Liu Q, He B, Huang SY, Wei F, Zhu XQ. Severe fever with thrombocytopenia syndrome, an emerging tick-borne zoonosis. Lancet Infect Dis. 2014; 14:763–772. PMID: 24837566.
Article3. Liu S, Chai C, Wang C, Amer S, Lv H, He H, et al. Systematic review of severe fever with thrombocytopenia syndrome: virology, epidemiology, and clinical characteristics. Rev Med Virol. 2014; 24:90–102. PMID: 24310908.4. Deng B, Zhang S, Geng Y, Zhang Y, Wang Y, Yao W, et al. Cytokine and chemokine levels in patients with severe fever with thrombocytopenia syndrome virus. PLoS One. 2012; 7:e41365. PMID: 22911786.
Article5. Choi SJ, Park SW, Bae IG, Kim SH, Ryu SY, Kim HA, et al. Severe fever with thrombocytopenia syndrome in South Korea, 2013-2015. PLoS Negl Trop Dis. 2016; 10:e0005264. PMID: 28033338.
Article6. Oh WS, Heo ST, Kim SH, Choi WJ, Han MG, Kim JY. Plasma exchange and ribavirin for rapidly progressive severe fever with thrombocytopenia syndrome. Int J Infect Dis. 2014; 18:84–86. PMID: 24161209.
Article7. Park SW, Han MG, Yun SM, Park C, Lee WJ, Ryou J. Severe fever with thrombocytopenia syndrome virus, South Korea, 2013. Emerg Infect Dis. 2014; 20:1880–1882. PMID: 25341085.
Article8. Gai ZT, Zhang Y, Liang MF, Jin C, Zhang S, Zhu CB, et al. Clinical progress and risk factors for death in severe fever with thrombocytopenia syndrome patients. J Infect Dis. 2012; 206:1095–1102. PMID: 22850122.
Article9. Zhang YZ, He YW, Dai YA, Xiong Y, Zheng H, Zhou DJ, et al. Hemorrhagic fever caused by a novel Bunyavirus in China: pathogenesis and correlates of fatal outcome. Clin Infect Dis. 2012; 54:527–533. PMID: 22144540.
Article10. Deng B, Zhou B, Zhang S, Zhu Y, Han L, Geng Y, et al. Clinical features and factors associated with severity and fatality among patients with severe fever with thrombocytopenia syndrome Bunyavirus infection in Northeast China. PLoS One. 2013; 8:e80802. PMID: 24236203.
Article11. Sun Y, Jin C, Zhan F, Wang X, Liang M, Zhang Q, et al. Host cytokine storm is associated with disease severity of severe fever with thrombocytopenia syndrome. J Infect Dis. 2012; 206:1085–1094. PMID: 22904342.
Article12. Stegmayr B. Apheresis in patients with severe sepsis and multi organ dysfunction syndrome. Transfus Apher Sci. 2008; 38:203–208. PMID: 18492616.
Article13. Kim UJ, Kim DM, Ahn JH, Kang SJ, Jang HC, Park KH, et al. Successful treatment of rapidly progressing severe fever with thrombocytopenia syndrome with neurological complications using intravenous immunoglobulin and corticosteroid. Antivir Ther. 2015; 21:637–640.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Fatal Pulmonary Event during Plasma Exchange in a Patient with Severe Fever with Thrombocytopenia Syndrome
- Strategies Against Severe Fever with Thrombocytopenia Syndrome Increasing in Korea
- Beneficial Effects of Plasma Exchange in Severe Guillain-Barre Syndrome
- Two Treatment Cases of Severe Fever and Thrombocytopenia Syndrome with Oral Ribavirin and Plasma Exchange
- Plasma Exchange in a Patient with Post-abortion Hemolytic Uremic Syndrome