Yonsei Med J.
2017 Jul;58(4):703-709. 10.3349/ymj.2017.58.4.703.
Comparison of De Novo versus Upgrade Cardiac Resynchronization Therapy; Focused on the Upgrade for Pacing-Induced Cardiomyopathy
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Heart Vascular Stroke Institute, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. orthovics@gmail.com
- 2Department of Cardiology, Hallym University Medical Center, Seoul, Korea.
- KMID: 2419074
- DOI: http://doi.org/10.3349/ymj.2017.58.4.703
Abstract
- PURPOSE
This study aimed to determine whether upgrade cardiac resynchronization therapy (CRT) shows better outcomes than de novo CRT. To do so, we compared the efficacy of CRT between de novo and upgrade groups, focusing particularly on the effect of upgrade CRT on patients with pacing-induced cardiomyopathy (PiCM).
MATERIALS AND METHODS
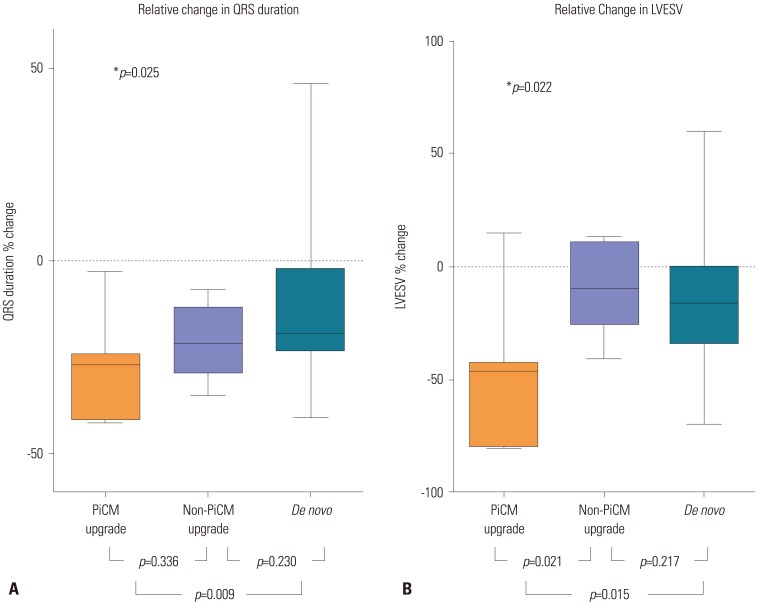
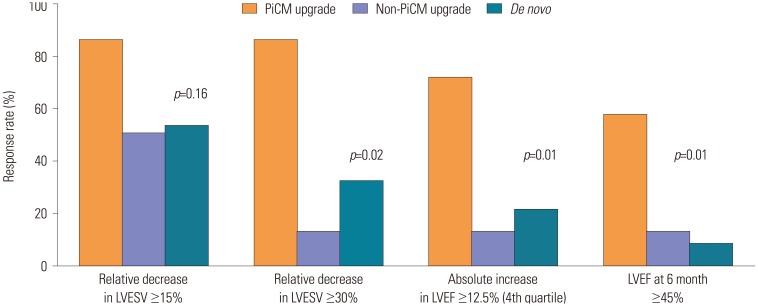
PiCM was defined as new-onset dilated cardiomyopathy following pacemaker implantation in patients with baseline normal ejection fraction ≥50%. Electro-mechanical reverse remodeling and clinical outcomes were compared among the de novo (n=62), PiCM upgrade (n=7), and non-PiCM upgrade (n=8) CRT groups.
RESULTS
The PiCM upgrade group showed significantly greater electro-mechanical reverse remodeling than the de novo CRT or non-PiCM upgrade groups at 6-month follow-up. The rate of super-responders was significantly higher in the PiCM upgrade group than the other CRT groups. The group factor of the PiCM upgrade was identified as an independent predictor of super-responder in multivariate analysis (odds ratio 10.4, 95% confidential interval 1.08-99.4, p=0.043). During the median follow-up of 15.8 months, the PiCM upgrade group showed the lowest rate of composite clinical outcomes, including cardiac death, heart transplantation, and heart failure-related rehospitalization (p=0.059).
CONCLUSION
The upgrade CRT for PiCM patients showed better performance in terms of electro-mechanical reverse remodeling than de novo implantation or upgrade CRT in non-PiCM patients.
MeSH Terms
Figure
Cited by 1 articles
-
Efficacy of Cardiac Resynchronization Therapy Using Automated Dynamic Optimization and Left Ventricular-only Pacing
Hye Bin Gwag, Youngjun Park, Seong Soo Lee, June Soo Kim, Kyoung-Min Park, Young Keun On, Seung-Jung Park
J Korean Med Sci. 2019;34(27):. doi: 10.3346/jkms.2019.34.e187.
Reference
-
1. Sweeney MO, Hellkamp AS. Heart failure during cardiac pacing. Circulation. 2006; 113:2082–2088. PMID: 16636167.
Article2. Sweeney MO, Hellkamp AS, Ellenbogen KA, Greenspon AJ, Freedman RA, Lee KL, et al. Adverse effect of ventricular pacing on heart failure and atrial fibrillation among patients with normal baseline QRS duration in a clinical trial of pacemaker therapy for sinus node dysfunction. Circulation. 2003; 107:2932–2937. PMID: 12782566.
Article3. Cho EJ, Park SJ, Park KM, On YK, Kim JS. Paced QT interval as a risk factor for new-onset left ventricular systolic dysfunction and cardiac death after permanent pacemaker implantation. Int J Cardiol. 2016; 203:158–163. PMID: 26523358.
Article4. Thackray SD, Witte KK, Nikitin NP, Clark AL, Kaye GC, Cleland JG. The prevalence of heart failure and asymptomatic left ventricular systolic dysfunction in a typical regional pacemaker population. Eur Heart J. 2003; 24:1143–1152. PMID: 12804929.
Article5. Yang JH, Kim JY, Kim SH, Oh YS. Reversal of pacing-induced cardiomyopathy by normal QRS axis pacing. Korean Circ J. 2016; 46:421–424. PMID: 27275181.
Article6. Mazza A, Bendini MG, Leggio M, Riva U, Ciardiello C, Valsecchi S, et al. Incidence and predictors of heart failure hospitalization and death in permanent pacemaker patients: a single-centre experience over medium-term follow-up. Europace. 2013; 15:1267–1272. PMID: 23444421.
Article7. O'Keefe JH Jr, Abuissa H, Jones PG, Thompson RC, Bateman TM, McGhie AI, et al. Effect of chronic right ventricular apical pacing on left ventricular function. Am J Cardiol. 2005; 95:771–773. PMID: 15757609.8. Zhang XH, Chen H, Siu CW, Yiu KH, Chan WS, Lee KL, et al. New-onset heart failure after permanent right ventricular apical pacing in patients with acquired high-grade atrioventricular block and normal left ventricular function. J Cardiovasc Electrophysiol. 2008; 19:136–141. PMID: 18005026.
Article9. Cleland JG, Daubert JC, Erdmann E, Freemantle N, Gras D, Kappenberger L, et al. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med. 2005; 352:1539–1549. PMID: 15753115.
Article10. Moss AJ, Hall WJ, Cannom DS, Klein H, Brown MW, Daubert JP, et al. Cardiac-resynchronization therapy for the prevention of heart-failure events. N Engl J Med. 2009; 361:1329–1338. PMID: 19723701.
Article11. European Society of Cardiology (ESC). European Heart Rhythm Association (EHRA). Brignole M, Auricchio A, Baron-Esquivias G, Bordachar P, et al. 2013 ESC guidelines on cardiac pacing and cardiac resynchronization therapy: the task force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Europace. 2013; 15:1070–1118. PMID: 23801827.12. Foley PW, Muhyaldeen SA, Chalil S, Smith RE, Sanderson JE, Leyva F. Long-term effects of upgrading from right ventricular pacing to cardiac resynchronization therapy in patients with heart failure. Europace. 2009; 11:495–501. PMID: 19307283.
Article13. Kabutoya T, Mitsuhashi T, Hata Y, Hashimoto T, Nakagami R, Osada J, et al. Beneficial effects of upgrading from right ventricular pacing to cardiac resynchronization therapy in patients with heart failure compared to de novo cardiac resynchronization therapy. J Arrhythmia. 2010; 26:16–20.
Article14. Bogale N, Witte K, Priori S, Cleland J, Auricchio A, Gadler F, et al. The European Cardiac Resynchronization Therapy Survey: comparison of outcomes between de novo cardiac resynchronization therapy implantations and upgrades. Eur J Heart Fail. 2011; 13:974–983. PMID: 21771823.
Article15. Tayal B, Gorcsan J 3rd, Delgado-Montero A, Goda A, Ryo K, Saba S, et al. Comparative long-term outcomes after cardiac resynchronization therapy in right ventricular paced patients versus native wide left bundle branch block patients. Heart Rhythm. 2016; 13:511–518. PMID: 26545939.
Article16. Adelstein E, Schwartzman D, Gorcsan J 3rd, Saba S. Predicting hyperresponse among pacemaker-dependent nonischemic cardiomyopathy patients upgraded to cardiac resynchronization. J Cardiovasc Electrophysiol. 2011; 22:905–911. PMID: 21332868.
Article17. Rad MM, Blaauw Y, Dinh T, Pison L, Crijns HJ, Prinzen FW, et al. Left ventricular lead placement in the latest activated region guided by coronary venous electroanatomic mapping. Europace. 2015; 17:84–93. PMID: 25186457.
Article18. Solomon SD, Foster E, Bourgoun M, Shah A, Viloria E, Brown MW, et al. Effect of cardiac resynchronization therapy on reverse remodeling and relation to outcome: multicenter automatic defibrillator implantation trial: cardiac resynchronization therapy. Circulation. 2010; 122:985–992. PMID: 20733097.19. Çelebi Ö, Knaus T, Blaschke F, Habedank D, Döhner W, Nitardy A, et al. Extraordinarily favorable left ventricular reverse remodeling through long-term cardiac resynchronization: super-response to cardiac resynchronization. Pacing Clin Electrophysiol. 2012; 35:870–876. PMID: 22553930.
Article20. Verhaert D, Grimm RA, Puntawangkoon C, Wolski K, De S, Wilkoff BL, et al. Long-term reverse remodeling with cardiac resynchronization therapy: results of extended echocardiographic follow-up. J Am Coll Cardiol. 2010; 55:1788–1795. PMID: 20413027.21. Killu AM, Grupper A, Friedman PA, Powell BD, Asirvatham SJ, Espinosa RE, et al. Predictors and outcomes of “super-response” to cardiac resynchronization therapy. J Card Fail. 2014; 20:379–386. PMID: 24632340.
Article22. Steffel J, Milosevic G, Hürlimann A, Krasniqi N, Namdar M, Ruschitzka F, et al. Characteristics and long-term outcome of echocardiographic super-responders to cardiac resynchronisation therapy: ‘real world’ experience from a single tertiary care centre. Heart. 2011; 97:1668–1674. PMID: 21821856.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Rapid and Potent Antiarrhythmic Effect of Cardiac Resynchronization Therapy in a Patient with Advanced Dilated Cardiomyopathy and a Large Ventricular Arrhythmia Burden
- Successful Placement of a Left Ventricular Pacing Lead Despite Coronary Sinus Dissection During Cardiac Resynchronization Therapy
- Current Role of Conduction System Pacing in Patients Requiring Permanent Pacing
- Cardiac Resynchronization Therapy: Biventricular Pacing
- Reversal of Pacing-Induced Cardiomyopathy by Normal QRS Axis Pacing