Korean J Radiol.
2018 Oct;19(5):859-865. 10.3348/kjr.2018.19.5.859.
Tree-in-Bud Pattern of Pulmonary Tuberculosis on Thin-Section CT: Pathological Implications
- Affiliations
-
- 1Department of Radiology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul 03080, Korea. imjgsnu@gmail.com
- 2Department of Radiology, Samsung Medical Center, Seoul 06351, Korea.
- 3University of Fukui, School of Medical Sciences, Bunkyo, Fukui-shi, Fukui 910-8507, Japan.
- KMID: 2418548
- DOI: http://doi.org/10.3348/kjr.2018.19.5.859
Abstract
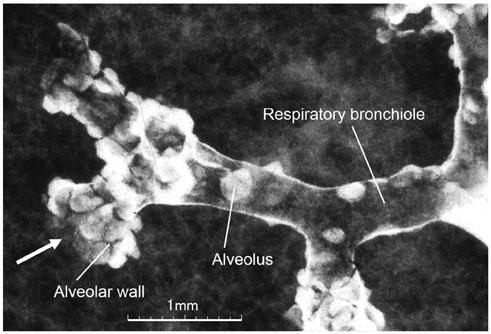
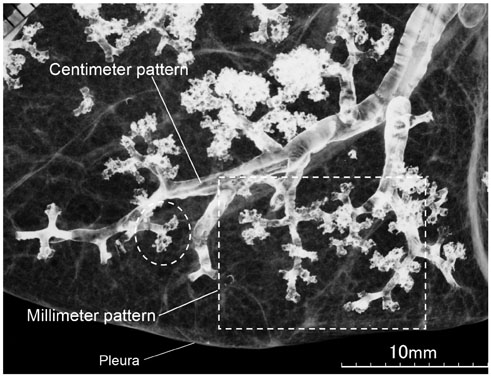
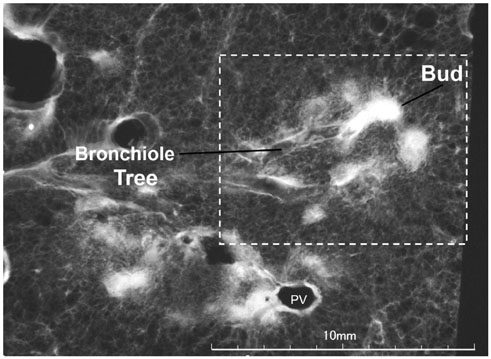
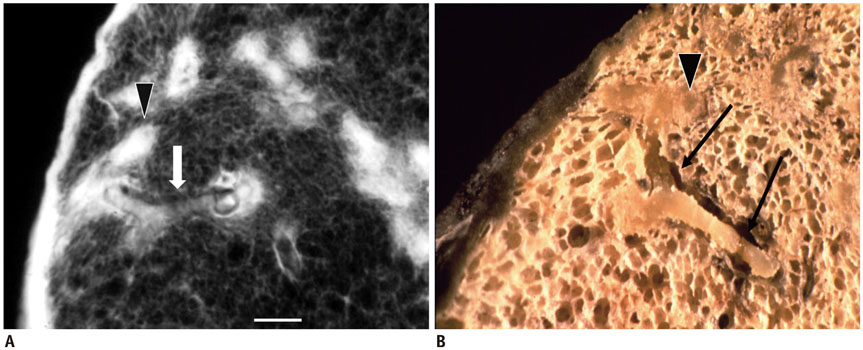
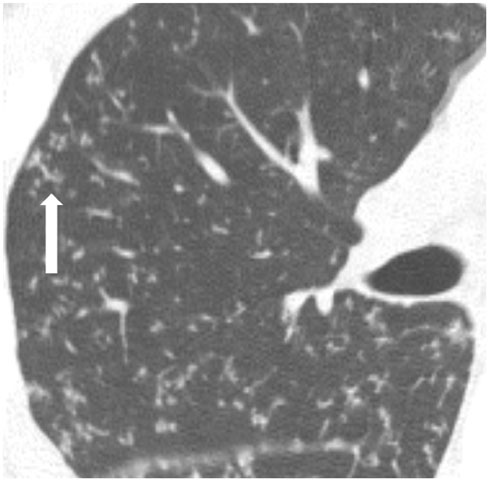
- The "tree-in-bud-pattern" of images on thin-section lung CT is defined by centrilobular branching structures that resemble a budding tree. We investigated the pathological basis of the tree-in-bud lesion by reviewing the pathological specimens of bronchograms of normal lungs and contract radiographs of the post-mortem lungs manifesting active pulmonary tuberculosis. The tree portion corresponds to the intralobular inflammatory bronchiole, while the bud portion represents filling of inflammatory substances within alveolar ducts, which are larger than the corresponding bronchioles. Inflammatory bronchiole per se represents the "tree" (stem) and inflammatory alveolar ducts constitute the "buds" or clubbing. "Clusters of micronodules", seen on 7-mm thick post-mortem radiographs with tuberculosis proved to be clusters of tree-in-bud lesions within the three-dimensional space of secondary pulmonary lobule based on radiological/pathological correlation. None of the post-mortem lung specimens showed findings of lung parenchymal lymphatics involvement.
Keyword
Figure
Cited by 1 articles
-
Diagnosis of pulmonary tuberculosis
Byung Woo Jhun, Hee Jae Huh, Won-Jung Koh
J Korean Med Assoc. 2019;62(1):18-24. doi: 10.5124/jkma.2019.62.1.18.
Reference
-
1. Im JG, Itoh H, Shim YS, Lee JH, Ahn J, Han MC, et al. Pulmonary tuberculosis: CT findings--early active disease and sequential change with antituberculous therapy. Radiology. 1993; 186:653–660.
Article2. Collins J, Blankenbaker D, Stern EJ. CT patterns of bronchiolar disease: what is “tree-in-bud”. AJR Am J Roentgenol. 1998; 171:365–370.
Article3. Eisenhuber E. The tree-in-bud sign. Radiology. 2002; 222:771–772.
Article4. Rossi SE, Franquet T, Volpacchio M, Giménez A, Aguilar G. Tree-in-bud pattern at thin-section CT of the lungs: radiologic-pathologic overview. Radiographics. 2005; 25:789–801.
Article5. Gosset N, Bankier AA, Eisenberg RL. Tree-in-bud pattern. AJR Am J Roentgenol. 2009; 193:W472–W477.
Article6. Verma N, Chung JH, Mohammed TL. “Tree-in-bud sign”. J Thorac Imaging. 2012; 27:W27.
Article7. Li Q, Fan X, Huang XT, Luo TY, Chu ZG, Chen L, et al. Tree-in-bud pattern in central lung cancer: CT findings and pathologic correlation. Lung Cancer. 2015; 88:260–266.
Article8. Tack D, Nollevaux MC, Gevenois PA. Tree-in-bud pattern in neoplastic pulmonary emboli. AJR Am J Roentgenol. 2001; 176:1421–1422.
Article9. Franquet T, Giménez A, Prats R, Rodríguez-Arias JM, Rodríguez C. Thrombotic microangiopathy of pulmonary tumors: a vascular cause of tree-in-bud pattern on CT. AJR Am J Roentgenol. 2002; 179:897–899.
Article10. Li Ng Y, Hwang D, Patsios D, Weisbrod G. Tree-in-bud pattern on thoracic CT due to pulmonary intravascular metastases from pancreatic adenocarcinoma. J Thorac Imaging. 2009; 24:150–151.
Article11. Moon JW, Lee HY, Han J, Lee KS. Tree-in-bud sign as a manifestation of localized pulmonary lymphatic metastasis from a pancreas cancer. Intern Med. 2011; 50:3027–3029.12. Hansell DM, Bankier AA, MacMahon H, McLoud TC, Müller NL, Remy J. Fleischner Society: glossary of terms for thoracic imaging. Radiology. 2008; 246:697–722.
Article13. Heo JN, Choi YW, Jeon SC, Park CK. Pulmonary tuberculosis: another disease showing clusters of small nodules. AJR Am J Roentgenol. 2005; 184:639–642.
Article14. Ko JM, Park HJ, Kim CH. Clinicoradiologic evidence of pulmonary lymphatic spread in adult patients with tuberculosis. AJR Am J Roentgenol. 2015; 204:38–43.
Article15. Heitzman ER. The lung: radiologic pathologic correlations. 2nd ed. St Louis, MO: Mosby;1984. p. 4–9.16. Itoh H, Tokunaga S, Asamoto H, Furuta M, Funamoto Y, Kitaichi M, et al. Radiologic-pathologic correlations of small lung nodules with special reference to peribronchiolar nodules. AJR Am J Roentgenol. 1978; 130:223–231.
Article17. Reid L, Simon G. The peripheral pattern in the normal bronchogram and its relation to peripheral pulmonary anatomy. Thorax. 1958; 13:103–109.
Article18. Hunter RL. Pathology of post primary tuberculosis of the lung: an illustrated critical review. Tuberculosis (Edinb). 2011; 91:497–509.
Article19. Akira M, Kitatani F, Lee YS, Kita N, Yamamoto S, Higashihara T, et al. Diffuse panbronchiolitis: evaluation with high-resolution CT. Radiology. 1988; 168:433–438.
Article20. Nakatsu M, Hatabu H, Morikawa K, Uematsu H, Ohno Y, Nishimura K, et al. Large coalescent parenchymal nodules in pulmonary sarcoidosis: “sarcoid galaxy” sign. AJR Am J Roentgenol. 2002; 178:1389–1393.
Article21. Mays TJ. Pulmonary consumption, pneumonia, and allied diseases of the lungs: their etiology, pathology and treatment, with a chapter on physical diagnosis. 1st ed. New York, NY: E.B. Treat & Co.;1901. p. 247–288.22. Gunn FD. Tuberculosis. In : Anderson WAD, editor. Pathology. 4th ed. St Louis, MO: C.V. Mosby Company;1961. p. 246–263.23. Haque AK. The pathology and pathophysiology of mycobacterial infections. J Thorac Imaging. 1990; 5:8–16.
Article24. Basaraba RJ, Smith EE, Shanley CA, Orme IM. Pulmonary lymphatics are primary sites of Mycobacterium tuberculosis infection in guinea pigs infected by aerosol. Infect Immun. 2006; 74:5397–5401.25. Kim WS, Choi JI, Cheon JE, Kim IO, Yeon KM, Lee HJ. Pulmonary tuberculosis in infants: radiographic and CT findings. AJR Am J Roentgenol. 2006; 187:1024–1033.
Article26. Kim WS, Moon WK, Kim IO, Lee HJ, Im JG, Yeon KM, et al. Pulmonary tuberculosis in children: evaluation with CT. AJR Am J Roentgenol. 1997; 168:1005–1009.
Article27. Miller WT Jr, Panosian JS. Causes and imaging patterns of tree-in-bud opacities. Chest. 2013; 144:1883–1892.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Thin-Section CT Findings of Nontuberculous Mycobacterial Pulmonary Diseases: Comparison Between Mycobacterium avium-intracellulare Complex and Mycobacterium abscessus Infection
- Pulmonary Manifestations of Fat Embolism on Thin-section CT: A Case Report
- Pulmonary Tuberculosis with Airspace Consolidation vs Mycoplasma Pneumonia in Adults: High-Resolution CT Findings
- Cystic Lung Changes in a Thin Section CT in an Asymptomatic Young Adult with Unilateral Pulmonary Vein Atresia: A Case Report
- Hematogenous Candida Pneumonia in Major Burn Patients: Plain Chest Radiograph and Thin-section CT Findings