Thin-Section CT Findings of Nontuberculous Mycobacterial Pulmonary Diseases: Comparison Between Mycobacterium avium-intracellulare Complex and Mycobacterium abscessus Infection
- Affiliations
-
- 1Department of Radiology and Center for Imaging Science, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. kyungs.lee@samsung.com
- 2Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Biostatistics Units, Samsung Biomedical Research Institute, Seoul, Korea.
- KMID: 1781760
- DOI: http://doi.org/10.3346/jkms.2005.20.5.777
Abstract
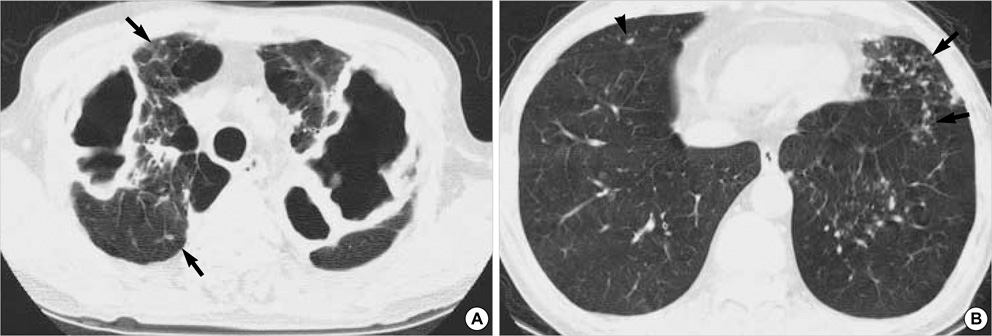
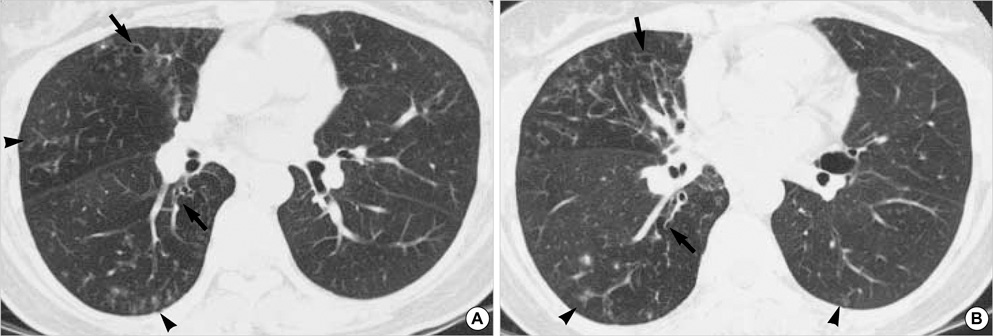
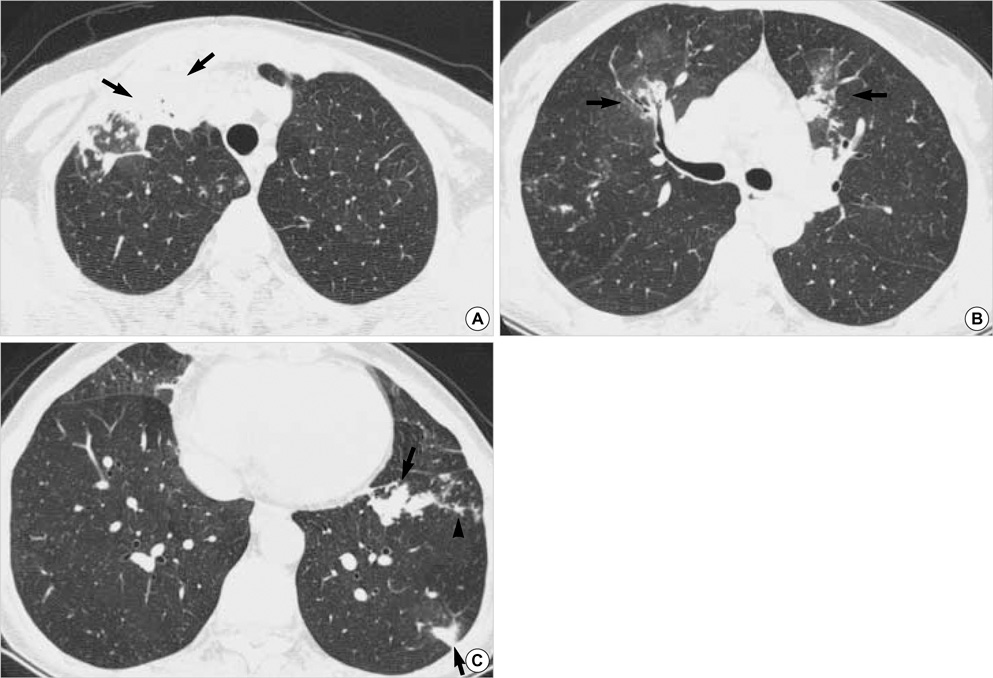
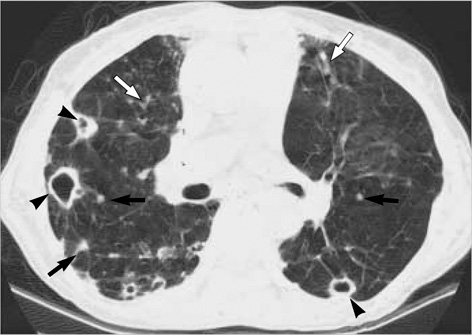
- We aimed to compare the CT findings of nontuberculous mycobacterial pulmonary diseases caused by Mycobacterium avium-intracellulare complex (MAC) and Mycobacterium abscessus. Two chest radiologists analyzed retrospectively the thin-section CT findings of 51 patients with MAC and 36 with M. abscessus infection in terms of patterns and forms of lung lesions. No significant difference was found between MAC and M. abscessus infection in the presence of small nodules, tree-in-bud pattern, and bronchiectasis. However, lobar volume decrease (p=0.001), nodule (p=0.018), airspace consolidation (p=0.047) and thin-walled cavity (p=0.009) were more frequently observed in MAC infection. The upper lobe cavitary form was more frequent in the MAC (19 of 51 patients, 37%) group than M. abscessus (5 of 36, 14%) (p=0.029), whereas the nodular bronchiectatic form was more frequent in the M. abscessus group ([29 of 36, 81%] vs. [27 of 51, 53%] in MAC) (p=0.012). In conclusion, there is considerable overlap in common CT findings of MAC and M. abscessus pulmonary infection; however, lobar volume loss, nodule, airspace consolidation, and thin-walled cavity are more frequently seen in MAC than M. abscessus infection.
Keyword
MeSH Terms
-
Adult
Aged
Aged, 80 and over
Anatomy, Cross-Sectional/methods
Diagnosis, Differential
Female
Humans
Lung Diseases/*microbiology/*radiography
Male
Middle Aged
Mycobacterium Infections, Atypical/microbiology/radiography
Mycobacterium avium-intracellulare Infection/microbiology/*radiography
Research Support, Non-U.S. Gov't
Retrospective Studies
Tomography, Spiral Computed/*methods
Tuberculosis, Pulmonary/radiography
Figure
Cited by 4 articles
-
Diagnosis and Treatment of Nontuberculous Mycobacterial Pulmonary Diseases: A Korean Perspective
Won-Jung Koh, O Jung Kwon, Kyung Soo Lee
J Korean Med Sci. 2005;20(6):913-925. doi: 10.3346/jkms.2005.20.6.913.Comparison of Clinical and Radiographic Characteristics between Nodular Bronchiectatic Form of Nontuberculous Mycobacterial Lung Disease and Diffuse Panbronchiolitis
Hye Yun Park, Gee Young Suh, Man Pyo Chung, Hojoong Kim, O Jung Kwon, Myung Jin Chung, Tae Sung Kim, Kyung Soo Lee, Won-Jung Koh
J Korean Med Sci. 2009;24(3):427-432. doi: 10.3346/jkms.2009.24.3.427.Standardized Combination Antibiotic Treatment of Mycobacterium avium Complex Lung Disease
Yun Su Sim, Hye Yun Park, Kyeongman Jeon, Gee Young Suh, O Jung Kwon, Won-Jung Koh
Yonsei Med J. 2010;51(6):888-894. doi: 10.3349/ymj.2010.51.6.888.Nontuberculous Mycobacterial Lung Disease
Won-Jung Koh, O Jung Kwon
J Korean Med Assoc. 2006;49(9):806-816. doi: 10.5124/jkma.2006.49.9.806.
Reference
-
1. Marras TK, Daley CL. Epidemiology of human pulmonary infection with nontuberculous mycobacteria. Clin Chest Med. 2002. 23:553–567.2. American Thoracic Society. Diagnosis and treatment of disease caused by nontuberculous mycobacteria. Am J Respir Crit Care Med. 1997. 156:S1–S25.3. O'Brien RJ, Geiter LJ, Snider DE Jr. The epidemiology of nontuberculous mycobacterial disease in the United States: results from a national survey. Am Rev Respir Dis. 1987. 135:1007–1014.4. Brown-Elliott BA, Wallace RJ Jr. Clinical and taxonomic status of pathogenic nonpigmented or late-pigmented rapidly growing mycobacteria. Clin Microbiol Rev. 2002. 15:716–746.5. Griffith DE, Girard WM, Wallace RJ Jr. Clinical features of pulmonary disease caused by rapidly growing mycobacteria: an analysis of 154 patients. Am Rev Respir Dis. 1993. 147:1271–1278.
Article6. Lew WJ, Ahn DI, Yoon YJ, Cho JS, Kwon DW, Kim SJ, Hong YP. Clinical experience on mycobacterial diseases other than tuberculosis. Tuberc Respir Dis. 1992. 39:425–432.7. Bai GH, Park KS, Kim SJ. Clinically isolated mycobacteria other than Mycobacterium tuberculosis from 1980 to 1990 in Korea. J Korean Soc Microbiol. 1993. 28:1–5.8. Korean Academy of Tuberculosis and Respiratory Disease. National survey of mycobacterial diseases other than tuberculosis in Korea. Tuberc Respir Dis. 1995. 42:277–294.9. Koh WJ, Kwon OJ, Ham HS, Suh GY, Chung MP, Kim H, Han D, Kim TS, Lee KS, Lee NY, Park EM, Park YK, Bai GH. Clinical significance of nontuberculous mycobacteria isolated from respiratory specimens. Korean J Intern Med. 2003. 65:10–21.10. Koh WJ, Kwon OJ, Suh GY, Chung MP, Kim H, Lee NY, Kim TS, Lee KS, Park EM, Park YK, Bai GH. A case report of three patients with nontuberculous mycobacterial pulmonary disease caused by Mycobacterium kansasii. Tuberc Respir Dis. 2003. 54:459–466.11. Moore EH. Atypical mycobacterial infection in the lung: CT appearance. Radiology. 1993. 187:777–782.
Article12. Primack SL, Logan PM, Hartman TE, Lee KS, Muller NL. Pulmonary tuberculosis and Mycobacterium avium-intracellulare: a comparison of CT findings. Radiology. 1995. 194:413–417.
Article13. Lynch DA, Simone PM, Fox MA, Bucher BL, Heinig MJ. CT features of pulmonary Mycobacterium avium complex infection. J Comput Assist Tomogr. 1995. 19:353–360.
Article14. Obayashi Y, Fujita J, Suemitsu I, Kamei T, Nii M, Takahara J. Successive follow-up of chest computed tomography in patients with Mycobacterium avium-intracellulare complex. Respir Med. 1999. 93:11–15.
Article15. Han D, Lee KS, Koh WJ, Yi CA, Kim TS, Kwon OJ. Radiographic and CT findings of nontuberculous mycobacterial pulmonary infection caused by Mycobacterium abscessus. AJR Am J Roentgenol. 2003. 181:513–517.
Article16. Jeong YJ, Lee KS, Koh WJ, Han J, Kim TS, Kwon OJ. Nontuberculous mycobacterial pulmonary infection in immunocompetent patients: comparison of thin-section CT and histopathologic findings. Radiology. 2004. 231:880–886.
Article17. Prince DS, Peterson DD, Steiner RM, Gottlieb JE, Scott R, Israel HL, Figueroa WG, Fish JE. Infection with Mycobacterium avium complex in patients without predisposing condition. N Engl J Med. 1989. 321:863–868.18. Reich JM, Johnson RE. Mycobacterium avium complex pulmonary disease presenting as an isolated lingular or middle lobe pattern. Chest. 1992. 101:1605–1609.
Article19. Hollings NP, Wells AU, Wilson R, Hansell DM. Comparative appearances of non-tuberculous mycobacteria species: a CT study. Eur Radiol. 2002. 12:2211–2217.
Article20. Fujiuchi S, Matsumoto H, Yamazaki Y, Nakao S, Takahashi M, Satoh K, Takeda A, Okamoto K, Fujita Y, Fujikane T, Shimizu T. Analysis of chest CT in patients with Mycobacterium avium complex pulmonary disease. Respiration. 2003. 70:76–81.21. Wittram C, Weisbrod GL. Mycobacterium avium complex lung disease in immunocompetent patients: radiography-CT correlation. Br J Radiol. 2002. 75:340–344.22. Koh WJ, Lee KS, Kwon OJ, Jeong YJ, Kwak SH, Kim TS. Bilateral bronchiectasis and bronchiolitis at thin-section CT: diagnostic implications in nontuberculous mycobacterial pulmonary infection. Radiology. 2005. 235:282–288.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Mycobacterium abscessus Lung Disease in a Patient with Cystic Fibrosis
- Mycobacterium intracellulare pulmonary infection accompanied with pleural effusion
- Diagnosis and treatment of nontuberculous mycobacterial lung disease
- Vertebral Osteomyelitis due to Mycobacterium intracellulare in an Immunocompetent Elderly Patient After Vertebroplasty
- Respiratory Review of 2009: Nontuberculous Mycobacterium