Healthc Inform Res.
2018 Apr;24(2):109-117. 10.4258/hir.2018.24.2.109.
Predicting Length of Stay in Intensive Care Units after Cardiac Surgery: Comparison of Artificial Neural Networks and Adaptive Neuro-fuzzy System
- Affiliations
-
- 1Department of Health Services Management, School of Management and Medical Information Sciences, Shiraz University of Medical Sciences, Shiraz, Iran. ra_ravangard@yahoo.com
- 2Student Research Committee, Shiraz University of Medical Sciences, Shiraz, Iran.
- 3Department of Health Information Management, School of Allied Medical Sciences, Tehran University of Medical Sciences, Tehran, Iran.
- 4Shiraz Anesthesiology and Critical Care Research Center, Shiraz University of Medical Sciences, Shiraz, Iran.
- 5Health Human Resources Research Centre, School of Management and Medical Information Sciences, Shiraz University of Medical Sciences, Shiraz, Iran.
- KMID: 2418179
- DOI: http://doi.org/10.4258/hir.2018.24.2.109
Abstract
OBJECTIVES
Accurate prediction of patients' length of stay is highly important. This study compared the performance of artificial neural network and adaptive neuro-fuzzy system algorithms to predict patients' length of stay in intensive care units (ICU) after cardiac surgery.
METHODS
A cross-sectional, analytical, and applied study was conducted. The required data were collected from 311 cardiac patients admitted to intensive care units after surgery at three hospitals of Shiraz, Iran, through a non-random convenience sampling method during the second quarter of 2016. Following the initial processing of influential factors, models were created and evaluated.
RESULTS
The results showed that the adaptive neuro-fuzzy algorithm (with mean squared error [MSE] = 7 and R = 0.88) resulted in the creation of a more precise model than the artificial neural network (with MSE = 21 and R = 0.60).
CONCLUSIONS
The adaptive neuro-fuzzy algorithm produces a more accurate model as it applies both the capabilities of a neural network architecture and experts' knowledge as a hybrid algorithm. It identifies nonlinear components, yielding remarkable results for prediction the length of stay, which is a useful calculation output to support ICU management, enabling higher quality of administration and cost reduction.
Keyword
MeSH Terms
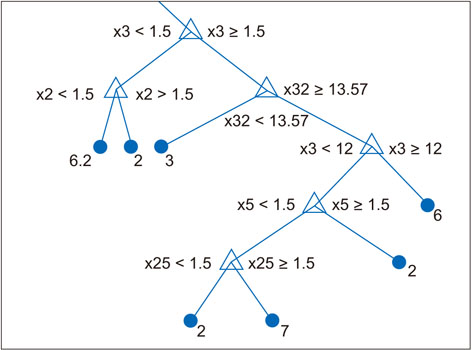
Figure
Reference
-
1. Noorizad S, Tabesh H, Mahdian M, Akbari H, Taghadosi M. Causes of mortality and morbidity in a neurosurgery ICU in Kashan 1999-2001. FEYZ. 2005; 9(2):15–20.2. University of California San Francisco. ICU outcome [Internet]. San Francisco (CA): University of California;c2018. cited at 2018 Apr 1. Available from: https://healthpolicy.ucsf.edu/icu-outcomes.3. Verburg IW, de Keizer NF, de Jonge E, Peek N. Comparison of regression methods for modeling intensive care length of stay. PLoS One. 2014; 9(10):e109684.
Article4. Ghoreishi Nejad S. Agent simulation in healthcare. Ottawa, Canada: University of Regina;2008.5. Widyastuti Y, Stenseth R, Wahba A, Pleym H, Videm V. Length of intensive care unit stay following cardiac surgery: is it impossible to find a universal prediction model. Interact Cardiovasc Thorac Surg. 2012; 15(5):825–832.
Article6. Hachesu PR, Ahmadi M, Alizadeh S, Sadoughi F. Use of data mining techniques to determine and predict length of stay of cardiac patients. Healthc Inform Res. 2013; 19(2):121–129.
Article7. Kotsiantis SB, Zaharakis I, Pintelas P. Supervised machine learning: a review of classification techniques. Emerg Artif Intell Appl Comput Eng. 2007; 160:3–24.8. Niakan Kalhori SR, Zeng XJ. Evaluation and comparison of different machine learning methods to predict outcome of tuberculosis treatment course. J Intell Learn Syst Appl. 2013; 5(3):184–193.9. Fallah M, Niakan Kalhori SR. Systematic review of data mining applications in patient-centered mobile-based information systems. Healthc Inform Res. 2017; 23(4):262–270.
Article10. Nabovati E, Azizi AA, Abbasi E, Vakili-Arki H, Zarei J, Razavi AR. Using data mining to predict outcome in burn patients: a comparison between several algorithms. Health Inf Manag. 2014; 10(6):789–799.11. Akbarian M, Paydar K, Kalhori SR, Sheikhtaheri A. Designing an artificial neural network for prediction of pregnancy outcomes in women with systemic lupus erythematosus in Iran. Tehran Univ Med J. 2015; 73(4):251–259.12. Jung E, Kim J, Choi SH, Kim M, Rhee H, Shin JM, et al. Artificial neural network study on organ-targeting peptides. J Comput Aided Mol Des. 2010; 24(1):49–56.
Article13. Jang JS. ANFIS: adaptive-network-based fuzzy inference system. IEEE Trans Syst Man Cybern. 1993; 23(3):665–685.
Article14. Sadeghi M, Yavarmanesh M, Shahidi Nojhabi M. Prediction of milk components impact on recovery and extraction of enteric viruses genome using artificial neural networks and adaptive nero fuzzy inference system (ANFIS). Res Iran Sci Technol. 2014; 10(2):156–164.15. Buyukbingol E, Sisman A, Akyildiz M, Alparslan FN, Adejare A. Adaptive neuro-fuzzy inference system (ANFIS): a new approach to predictive modeling in QSAR applications: a study of neuro-fuzzy modeling of PCPbased NMDA receptor antagonists. Bioorg Med Chem. 2007; 15(12):4265–4282.
Article16. Goodarzi M, Freitas MP. MIA-QSAR coupled to principal component analysis-adaptive neuro-fuzzy inference systems (PCA-ANFIS) for the modeling of the anti-HIV reverse transcriptase activities of TIBO derivatives. Eur J Med Chem. 2010; 45(4):1352–1358.
Article17. Polat K, Yosunkaya S, Gunes S. Pairwise ANFIS approach to determining the disorder degree of obstructive sleep apnea syndrome. J Med Syst. 2008; 32(5):379–387.
Article18. Riahi-Madvar H, Ayyoubzadeh SA, Khadangi E, Ebadzadeh MM. An expert system for predicting longitudinal dispersion coefficient in natural streams by using ANFIS. Expert Syst Appl. 2009; 36(4):8589–8596.
Article19. Carter EM, Potts HW. Predicting length of stay from an electronic patient record system: a primary total knee replacement example. BMC Med Inform Decis Mak. 2014; 14:26.
Article20. Sung SF, Hsieh CY, Kao Yang YH, Lin HJ, Chen CH, Chen YW, et al. Developing a stroke severity index based on administrative data was feasible using data mining techniques. J Clin Epidemiol. 2015; 68(11):1292–1300.
Article21. LaFaro RJ, Pothula S, Kubal KP, Inchiosa ME, Pothula VM, Yuan SC, et al. Neural network prediction of ICU length of stay following cardiac surgery based on preincision variables. PLoS One. 2015; 10(12):e0145395.
Article22. Sharma SK. Creating knowledge-based healthcare organizations. Hershey (PA): IGI Global;2005.23. Atoui R, Ma F, Langlois Y, Morin JF. Risk factors for prolonged stay in the intensive care unit and on the ward after cardiac surgery. J Card Surg. 2008; 23(2):99–106.
Article24. Gomes C, Almada-Lobo B, Borges J, Soares C. Integrating data mining and optimization techniques on surgery scheduling. In : Zhou S, Zhang S, Karypis G, editors. International conference on advanced data mining and applications. Heidelberg: Springer;2012. p. 589–602.25. Abrahamyan L, Demirchyan A, Thompson ME, Hovaguimian H. Determinants of morbidity and intensive care unit stay after coronary surgery. Asian Cardiovasc Thorac Ann. 2006; 14(2):114–118.
Article26. Tu JV, Mazer CD, Levinton C, Armstrong PW, Naylor CD. A predictive index for length of stay in the intensive care unit following cardiac surgery. CMAJ. 1994; 151(2):177–185.
Article27. Tu JV, Mazer CD. Can clinicians predict ICU length of stay following cardiac surgery. Can J Anaesth. 1996; 43(8):789–794.
Article28. Wong DT, Cheng DC, Kustra R, Tibshirani R, Karski J, Carroll-Munro J, et al. Risk factors of delayed extubation, prolonged length of stay in the intensive care unit, and mortality in patients undergoing coronary artery bypass graft with fast-track cardiac anesthesia: a new cardiac risk score. Anesthesiology. 1999; 91(4):936–944.
Article29. Bashour CA, Yared JP, Ryan TA, Rady MY, Mascha E, Leventhal MJ, et al. Long-term survival and functional capacity in cardiac surgery patients after prolonged intensive care. Crit Care Med. 2000; 28(12):3847–3853.
Article30. Bucerius J, Gummert JF, Walther T, Doll N, Falk V, Schmitt DV, et al. Predictors of prolonged ICU stay after on-pump versus off-pump coronary artery bypass grafting. Intensive Care Med. 2004; 30(1):88–95.
Article31. Ghotkar SV, Grayson AD, Fabri BM, Dihmis WC, Pullan DM. Preoperative calculation of risk for prolonged intensive care unit stay following coronary artery bypass grafting. J Cardiothorac Surg. 2006; 1:14.
Article32. Xu J, Ge Y, Hu S, Song Y, Sun H, Liu P. A simple predictive model of prolonged intensive care unit stay after surgery for acquired heart valve disease. J Heart Valve Dis. 2007; 16(2):109–115.33. Janssen DP, Noyez L, Wouters C, Brouwer RM. Preoperative prediction of prolonged stay in the intensive care unit for coronary bypass surgery. Eur J Cardiothorac Surg. 2004; 25(2):203–207.
Article34. Hein OV, Birnbaum J, Wernecke K, England M, Konertz W, Spies C. Prolonged intensive care unit stay in cardiac surgery: risk factors and long-term-survival. Ann Thorac Surg. 2006; 81(3):880–885.
Article35. Christakis GT, Fremes SE, Naylor CD, Chen E, Rao V, Goldman BS. Impact of preoperative risk and perioperative morbidity on ICU stay following coronary bypass surgery. Cardiovasc Surg. 1996; 4(1):29–35.
Article36. Rosenfeld R, Smith JM, Woods SE, Engel AM. Predictors and outcomes of extended intensive care unit length of stay in patients undergoing coronary artery bypass graft surgery. J Card Surg. 2006; 21(2):146–150.
Article37. Belderrar A, Hazzab A. Hierarchical genetic algorithm and fuzzy radial basis function networks for factors influencing hospital length of stay outliers. Healthc Inform Res. 2017; 23(3):226–232.
Article38. Kwon YD, Yoon SS, Chang H. Knowledge extraction from hospital information system: using the integrated database of electronic medical record and patient management system. J Korean Soc Med Inform. 2007; 13(2):115–122.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A study on Recognition of Bronchogenic Cancer Cell using Fuzzy Neural Networks
- Hierarchical Genetic Algorithm and Fuzzy Radial Basis Function Networks for Factors Influencing Hospital Length of Stay Outliers
- Cardiac Complications in Patients Admitted to the Neuro-Intensive Care Unit
- Are frailty scales better than anesthesia or surgical scales to determine risk in cardiac surgery?
- Evaluation of the Clinical Effect of Intravenous Glutamine on Intensive Care Unit Patients