Korean J Ophthalmol.
2018 Aug;32(4):281-289. 10.3341/kjo.2017.0144.
Association of Central Serous Chorioretinopathy with Psychosocial Factors is Dependent on Its Phase and Subtype
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. sejoon1@snu.ac.kr
- 2Department of Ophthalmology, Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea.
- 3Department of Neuropsychiatry, Seoul National University Bundang Hospital, Seongnam, Korea. kwkimmd@snu.ac.kr
- 4Department of Psychiatry, Seoul National University College of Medicine, Seoul, Korea.
- 5Department of Brain and Cognitive Science, Seoul National University College of Natural Sciences, Seoul, Korea.
- KMID: 2418148
- DOI: http://doi.org/10.3341/kjo.2017.0144
Abstract
- PURPOSE
To analyze the psychosocial factors associated with central serous chorioretinopathy (CSC) according to its phases and subtypes and to correlate the factors with the extent of choroidal hyperpermeability.
METHODS
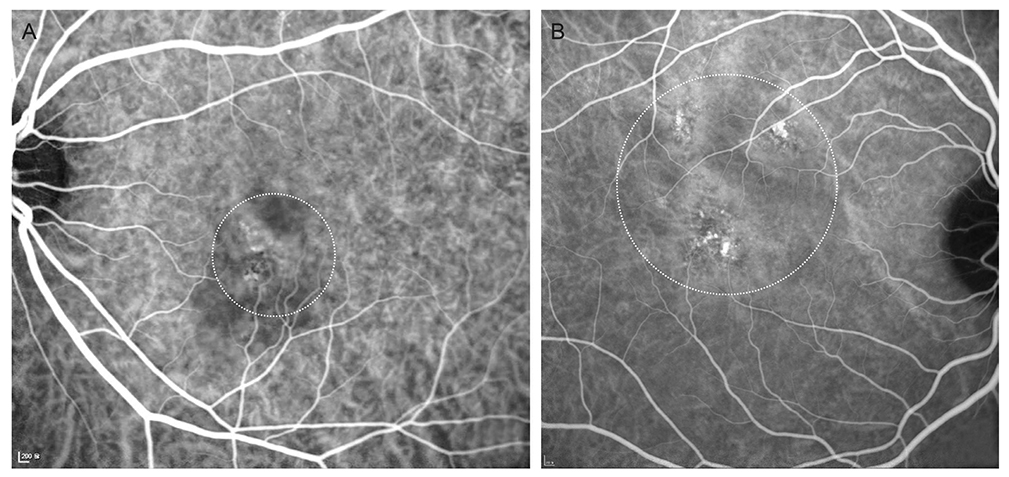
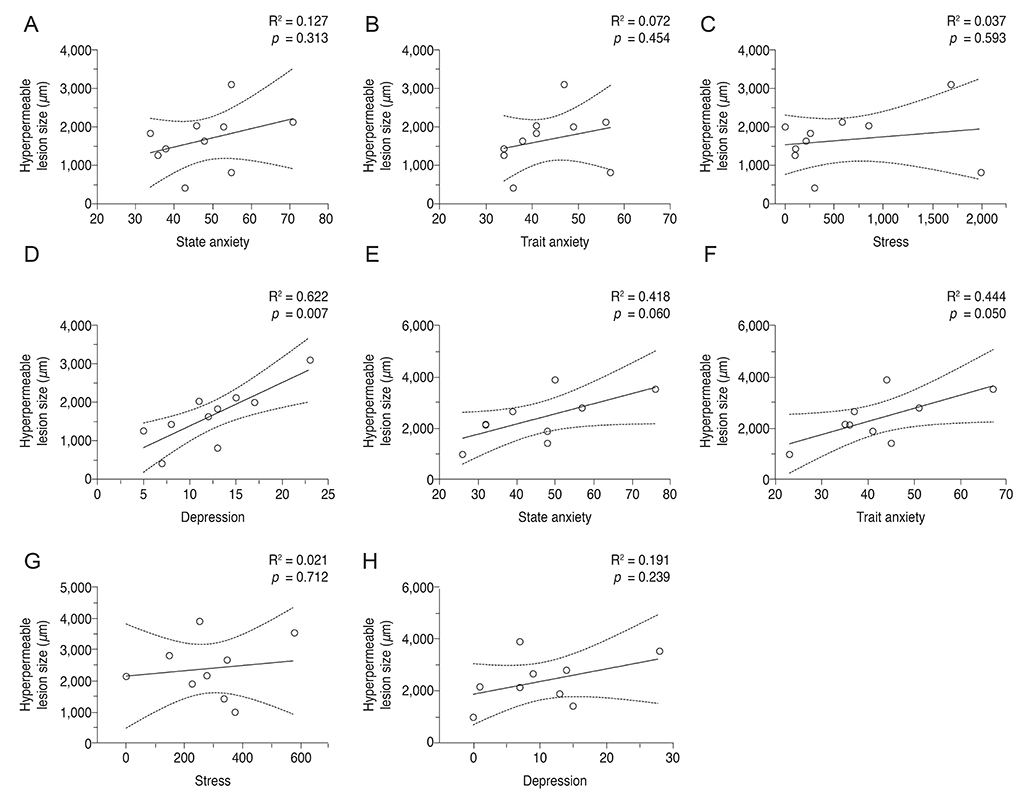
Age- and sex-matched CSC patients and controls (n = 37 in each group) were enrolled, and their psychosocial factors were compared. CSC was divided into two phases (active and inactive), and active CSC was further divided into two subtypes (acute and chronic). The correlations between the size of the hyperpermeable choroidal lesion identified on indocyanine green angiography and psychosocial factors were examined.
RESULTS
Active CSC patients experienced more stressful events (p = 0.030), were more depressive (p = 0.037), and felt less emotional (p = 0.014) and informational (p = 0.014) support than the matched controls, whereas inactive CSC patients were comparable to the matched controls in all psychosocial factors. Among the active CSC patients, acute patients were more depressive (p = 0.029), while chronic patients experienced more stressful events (p = 0.024) than their matched controls. The size of the hyperpermeable choroidal lesion was correlated with the severity of depression in acute patients.
CONCLUSIONS
Association of CSC with psychosocial factors was dependent on the phase and subtype of CSC. Psychosocial factors were associated with CSC in the active phase, and severity of depression was correlated with the size of the choroidal pathology in acute active CSC. Further prospective studies to investigate if psychosocial factors can trigger CSC are warranted.
MeSH Terms
Figure
Reference
-
1. Spaide RF, Campeas L, Haas A, et al. Central serous chorioretinopathy in younger and older adults. Ophthalmology. 1996; 103:2070–2079.
Article2. Tittl MK, Spaide RF, Wong D, et al. Systemic findings associated with central serous chorioretinopathy. Am J Ophthalmol. 1999; 128:63–68.
Article3. Yannuzzi LA. Type-A behavior and central serous chorioretinopathy. Retina. 1987; 7:111–131.
Article4. Tsai DC, Chen SJ, Huang CC, et al. Epidemiology of idiopathic central serous chorioretinopathy in Taiwan, 2001–2006: a population-based study. PLoS One. 2013; 8:e66858.
Article5. Conrad R, Geiser F, Kleiman A, et al. Temperament and character personality profile and illness-related stress in central serous chorioretinopathy. ScientificWorldJournal. 2014; 2014:631687.
Article6. Piskunowicz M, Jaracz M, Lesiewska H, et al. Temperament profile in patients with central serous chorioretinopathy: a case-control study. Eur J Ophthalmol. 2014; 24:392–395.
Article7. Sahin A, Bez Y, Kaya MC, et al. Psychological distress and poor quality of life in patients with central serous chorioretinopathy. Semin Ophthalmol. 2014; 29:73–76.8. Bazzazi N, Ahmadpanah M, Akbarzadeh S, et al. In patients suffering from idiopathic central serous chorioretinopathy, anxiety scores are higher than in healthy controls, but do not vary according to sex or repeated central serous chorioretinopathy. Neuropsychiatr Dis Treat. 2015; 11:1131–1136.9. Caccavale A, Romanazzi F, Imparato M, et al. Central serous chorioretinopathy: a pathogenetic model. Clin Ophthalmol. 2011; 5:239–243.
Article10. Conrad R, Bodeewes I, Schilling G, et al. Central serous chorioretinopathy and psychological stress. Ophthalmologe. 2000; 97:527–531.11. Conrad R, Weber NF, Lehnert M, et al. Alexithymia and emotional distress in patients with central serous chorioretinopathy. Psychosomatics. 2007; 48:489–495.
Article12. Piccolino FC, Borgia L. Central serous chorioretinopathy and indocyanine green angiography. Retina. 1994; 14:231–242.
Article13. Spaide RF, Hall L, Haas A, et al. Indocyanine green videoangiography of older patients with central serous chorioretinopathy. Retina. 1996; 16:203–213.
Article14. Spielberger CD, Gorsuch RL, Lushene R, et al. Manual for the State-Trait Anxiety Inventory. Palo Alto: Consulting Psychologists Press;1983.15. Hahn DW, Lee CH, Chon KK. Korean adaptation of Spielberger's STAI (K-STAI). Korean J Health Psychol. 1996; 1:1–14.16. Beck AT, Ward CH, Mendelson M, et al. An inventory for measuring depression. Arch Gen Psychiatry. 1961; 4:561–571.
Article17. Holmes TH, Rahe RH. The social readjustment rating scale. J Psychosom Res. 1967; 11:213–218.
Article18. Endler NS, Parker JD. Multidimensional assessment of coping: a critical evaluation. J Pers Soc Psychol. 1990; 58:844–854.
Article19. Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991; 32:705–714.
Article20. Spahn C, Wiek J, Burger T, Hansen L. Psychosomatic aspects in patients with central serous chorioretinopathy. Br J Ophthalmol. 2003; 87:704–708.
Article21. Franke GH, Esser J, Stacker KH, et al. “Filtered normality”: psychological causes and sequelae of specific retinal diseases. Psychother Psychosom Med Psychol. 1996; 46:159–168.22. Lahousen T, Painold A, Luxenberger W, et al. Psychological factors associated with acute and chronic central serous chorioretinopathy. Nord J Psychiatry. 2016; 70:24–30.
Article23. Zhao M, Celerier I, Bousquet E, et al. Mineralocorticoid receptor is involved in rat and human ocular chorioretinopathy. J Clin Invest. 2012; 122:2672–2679.
Article24. Daruich A, Matet A, Dirani A, et al. Central serous chorioretinopathy: recent findings and new physiopathology hypothesis. Prog Retin Eye Res. 2015; 48:82–118.
Article25. Bousquet E, Beydoun T, Rothschild PR, et al. Spironolactone for nonresolving central serous chorioretinopathy: a randomized controlled crossover study. Retina. 2015; 35:2505–2515.26. Daruich A, Matet A, Dirani A, et al. Oral mineralocorticoid-receptor antagonists: real-life experience in clinical subtypes of nonresolving central serous chorioretinopathy with chronic epitheliopathy. Transl Vis Sci Technol. 2016; 5:2.
Article27. Ghadiali Q, Jung JJ, Yu S, et al. Central serous chorioretinopathy treated with mineralocorticoid antagonists: a one-year pilot study. Retina. 2016; 36:611–618.28. Young EA, Lopez JF, Murphy-Weinberg V, Watson SJ, Akil H. Mineralocorticoid receptor function in major depression. Arch Gen Psychiatry. 2003; 60:24–28.
Article29. Chen J, Wang ZZ, Zhang S, Zuo W, Chen NH. Does mineralocorticoid receptor play a vital role in the development of depressive disorder? Life Sci. 2016; 152:76–81.
Article30. Tsai DC, Chen SJ, Huang CC, et al. Risk of central serous chorioretinopathy in adults prescribed oral corticosteroids: a population-based study in Taiwan. Retina. 2014; 34:1867–1874.31. Warrow DJ, Hoang QV, Freund KB. Pachychoroid pigment epitheliopathy. Retina. 2013; 33:1659–1672.
Article32. Pang CE, Freund KB. Pachychoroid neovasculopathy. Retina. 2015; 35:1–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of Atypical Central Serous Chorioretinopathy with Bullous Retinal Detachment
- A Case of Central Serous Chorioretinopathy Following Systemic Corticosteroid Therapy
- Electronmicroscopic Study of the Effect of Hexamethonium on Serous Choriretinopathy in Rabbits
- Stellate Ganglion Block for Treatment of Central Serous Chorioretinopathy
- A Seasonal Variation of Central Serous Chorioretinopathy