Korean J Ophthalmol.
2018 Aug;32(4):273-280. 10.3341/kjo.2017.0113.
Predicting Factor of Visual Outcome in Unilateral Idiopathic Cataract Surgery in Patients Aged 3 to 10 Years
- Affiliations
-
- 1Daesung Eye Clinic, Bucheon, Korea.
- 2Department of Cornea and Refractive Surgery, Kim's Eye Hospital, Myung-Gok Eye Research Institute, Konyang University College of Medicine, Seoul, Korea. kby@kimeye.com
- KMID: 2418147
- DOI: http://doi.org/10.3341/kjo.2017.0113
Abstract
- PURPOSE
To report the surgical results of unilateral pediatric cataracts from uncertain causes in relatively older children and to identify factors related to better visual outcomes.
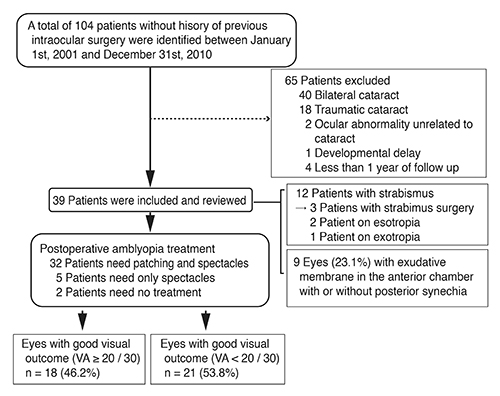
METHODS
We retrospectively evaluated the medical records of 39 patients who underwent surgery between the ages of 3 and 10 years for unilateral pediatric cataracts of no known cause. All patients underwent primary intraocular lens implantation and postoperative amblyopia treatment. A postoperative final visual acuity better than 20 / 30 was considered to be a good visual outcome.
RESULTS
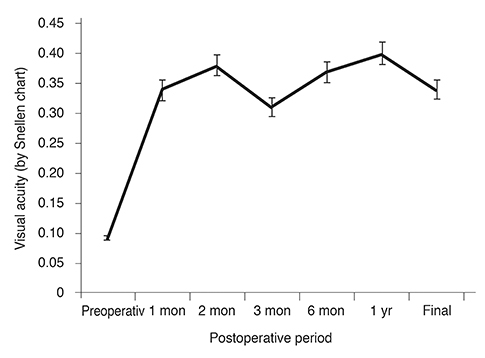
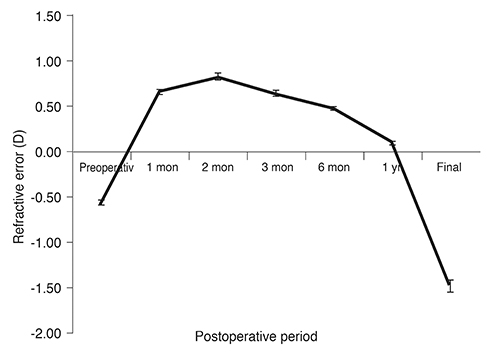
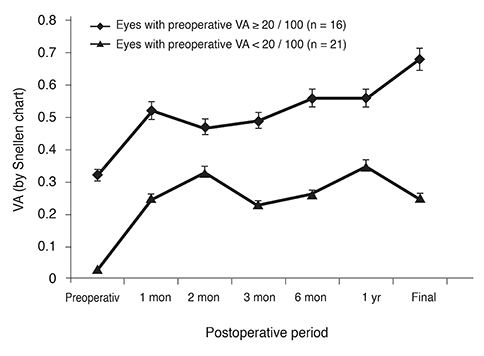
The mean age of patients was 6.0 ± 1.8 years at the time of surgery. The mean preoperative visual acuity was 1.07 ± 0.71 logarithm of the minimum angle of resolution (range, 0.15 to 3.00), while the mean final postoperative visual acuity was 0.47 ± 0.54 logarithm of the minimum angle of resolution (range, 0.00 to 2.00). Of 39 patients, 18 (46.2%) achieved a good visual outcome. Only the preoperative visual acuity maintained a significant association with a good visual outcome according to our multivariate analysis (p = 0.040). A preoperative visual acuity of 20 / 100 or better was found to increase the chance of achieving a good visual outcome by 13.79-fold (95% confidence interval, 1.13 to 167.58).
CONCLUSIONS
The visual outcome of unilateral pediatric cataract surgery for cataracts with no specific cause identified in patients after three years of age could be satisfactory, especially with a preoperative visual acuity of 20 / 100 or better.
MeSH Terms
Figure
Reference
-
1. Drummond GT, Scott WE, Keech RV. Management of monocular congenital cataracts. Arch Ophthalmol. 1989; 107:45–51.
Article2. Birch EE, Stager DR. The critical period for surgical treatment of dense congenital unilateral cataract. Invest Ophthalmol Vis Sci. 1996; 37:1532–1538.
Article3. Lundvall A, Kugelberg U. Outcome after treatment of congenital unilateral cataract. Acta Ophthalmol Scand. 2002; 80:588–592.
Article4. Allen RJ, Speedwell L, Russell-Eggitt I. Long-term visual outcome after extraction of unilateral congenital cataracts. Eye (Lond). 2010; 24:1263–1267.
Article5. Parks MM, Johnson DA, Reed GW. Long-term visual results and complications in children with aphakia. A function of cataract type. Ophthalmology. 1993; 100:826–840.6. You C, Wu X, Zhang Y, et al. Visual impairment and delay in presentation for surgery in chinese pediatric patients with cataract. Ophthalmology. 2011; 118:17–23.
Article7. Zwaan J, Mullaney PB, Awad A, et al. Pediatric intraocular lens implantation. Surgical results and complications in more than 300 patients. Ophthalmology. 1998; 105:112–118.8. Crouch ER Jr, Pressman SH, Crouch ER. Posterior chamber intraocular lenses: long-term results in pediatric cataract patients. J Pediatr Ophthalmol Strabismus. 1995; 32:210–218.
Article9. Crouch ER, Crouch ER Jr, Pressman SH. Prospective analysis of pediatric pseudophakia: myopic shift and postoperative outcomes. J AAPOS. 2002; 6:277–282.
Article10. Ledoux DM, Trivedi RH, Wilson ME Jr, Payne JF. Pediatric cataract extraction with intraocular lens implantation: visual acuity outcome when measured at age four years and older. J AAPOS. 2007; 11:218–224.
Article11. Weisberg OL, Sprunger DT, Plager DA, et al. Strabismus in pediatric pseudophakia. Ophthalmology. 2005; 112:1625–1628.
Article12. Lambert SR, Lynn M, Drews-Botsch C, et al. A comparison of grating visual acuity, strabismus, and reoperation outcomes among children with aphakia and pseudophakia after unilateral cataract surgery during the first six months of life. J AAPOS. 2001; 5:70–75.
Article13. Gochnauer AC, Trivedi RH, Hill EG, Wilson ME. Interocular axial length difference as a predictor of postoperative visual acuity after unilateral pediatric cataract extraction with primary IOL implantation. J AAPOS. 2010; 14:20–24.
Article14. Lal G, Trivedi RH, Wilson ME Jr, et al. Interocular axial length difference in eyes with pediatric cataracts. J AAPOS. 2005; 9:358–362.
Article15. Congdon NG, Ruiz S, Suzuki M, Herrera V. Determinants of pediatric cataract program outcomes and follow-up in a large series in Mexico. J Cataract Refract Surg. 2007; 33:1775–1780.
Article16. Greenwald MJ, Glaser SR. Visual outcomes after surgery for unilateral cataract in children more than two years old: posterior chamber intraocular lens implantation versus contact lens correction of aphakia. J AAPOS. 1998; 2:168–176.
Article17. McClatchey SK, Dahan E, Maselli E, et al. A comparison of the rate of refractive growth in pediatric aphakic and pseudophakic eyes. Ophthalmology. 2000; 107:118–122.18. Superstein R, Archer SM, Del Monte MA. Minimal myopic shift in pseudophakic versus aphakic pediatric cataract patients. J AAPOS. 2002; 6:271–276.
Article19. Asrani S, Freedman S, Hasselblad V, et al. Does primary intraocular lens implantation prevent “aphakic” glaucoma in children? J AAPOS. 2000; 4:33–39.
Article20. Trivedi RH, Wilson ME. Biometry data from caucasian and african-american cataractous pediatric eyes. Invest Ophthalmol Vis Sci. 2007; 48:4671–4678.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Long-term Outcomes after Surgery for Congenital Unilateral Cataract
- Postoperative Visual Outcome of Congenital Cataract with Possibility of Conservation of Vision
- Clinical Study of Cataract Surgery in Patients Over 80 Years of Age
- A Relative Afferent Pupillary Defect in the Contralateral Eye of a Unilateral Cataract
- A Comparison of Clinical Results in Unilateral and Bilateral Cataract Surgerys