J Korean Med Sci.
2017 Jan;32(1):77-84. 10.3346/jkms.2017.32.1.77.
Is β-Lactam Plus Macrolide More Effective than β-Lactam Plus Fluoroquinolone among Patients with Severe Community-Acquired Pneumonia?: a Systemic Review and Meta-Analysis
- Affiliations
-
- 1Department of Internal Medicine, Jeju National University Hospital, Jeju, Korea.
- 2Institute for Evidence-based Medicine, Department of Preventive Medicine, Korea University College of Medicine, Seoul, Korea.
- 3Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Kyung Hee University Hospital at Gangdong, Seoul, Korea. yhkim2007@hotmail.co.kr
- KMID: 2417588
- DOI: http://doi.org/10.3346/jkms.2017.32.1.77
Abstract
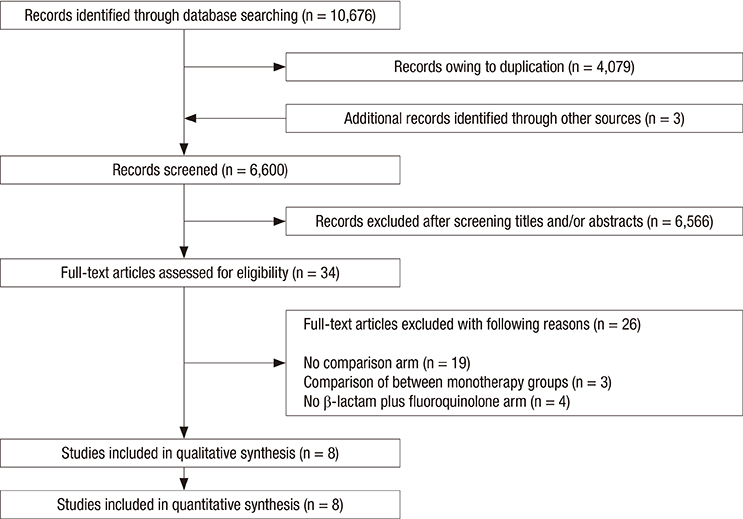
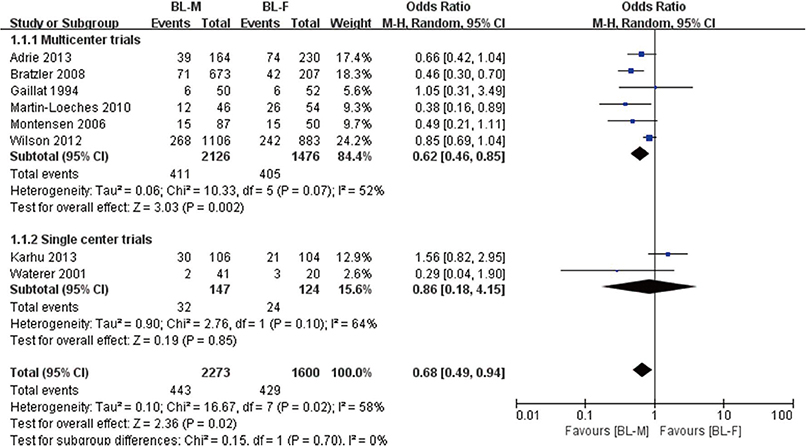
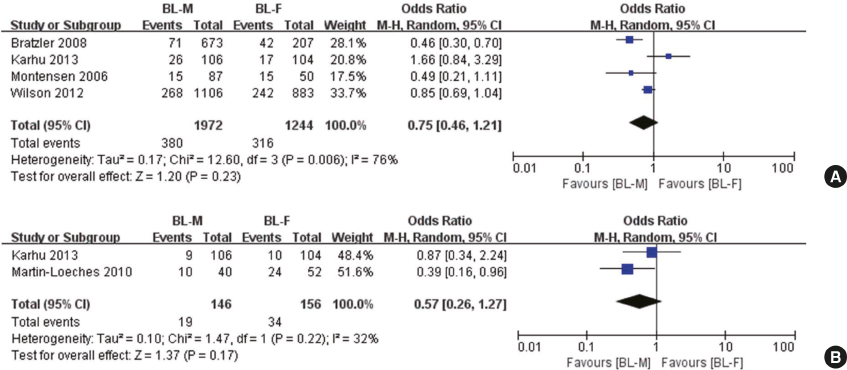
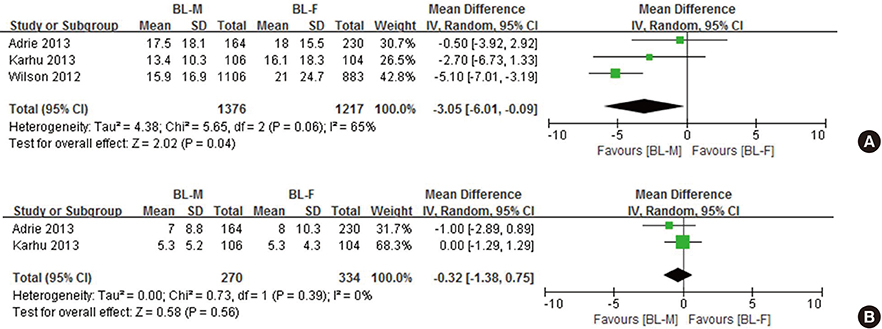
- Adding either macrolide or fluoroquinolone (FQ) to β-lactam has been recommended for patients with severe community-acquired pneumonia (CAP). However, due to the limited evidence available, there is a question as to the superiority of the two combination therapies. The MEDLINE, EMBASE, Cochrane Central Register, Scopus, and Web of Science databases were searched for systematic review and meta-analysis. A total of eight trials were analyzed. The total number of patients in the β-lactam plus macrolide (BL-M) and β-lactam plus fluoroquinolone (BL-F) groups was 2,273 and 1,600, respectively. Overall mortality of the BL-M group was lower than that of the BL-F group (19.4% vs. 26.8%), which showed statistical significance (odds ratio [OR], 0.68; 95% confidence interval [CI], 0.49 to 0.94; P = 0.02). Length of hospital stay was reduced in the BL-M group compared to the BL-F group (mean difference, −3.05 days; 95% CI, −6.01 to −0.09; P = 0.04). However, there was no significant difference in length of intensive care unit (ICU) stay between the two groups. Among patients with severe CAP, BL-M therapy may better reduce overall mortality and length of hospital stay than BL-F therapy. However, we could not elicit strong conclusions from the available trials due to high risk of bias and methodological limitations.
Keyword
MeSH Terms
Figure
Reference
-
1. Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001; 29:1303–1310.2. Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, Dowell SF, File TM Jr, Musher DM, Niederman MS, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007; 44:Suppl 2. S27–72.3. Rodríguez A, Mendia A, Sirvent JM, Barcenilla F, de la Torre-Prados MV, Solé-Violán J, Rello J; CAPUCI Study Group. Combination antibiotic therapy improves survival in patients with community-acquired pneumonia and shock. Crit Care Med. 2007; 35:1493–1498.4. Lee JH, Ryu YJ, Chun EM, Chang JH. Outcomes and prognostic factors for severe community-acquired pneumonia that requires mechanical ventilation. Korean J Intern Med. 2007; 22:157–163.5. Sligl WI, Marrie TJ. Severe community-acquired pneumonia. Crit Care Clin. 2013; 29:563–601.6. Postma DF, van Werkhoven CH, van Elden LJ, Thijsen SF, Hoepelman AI, Kluytmans JA, Boersma WG, Compaijen CJ, van der Wall E, Prins JM, et al. Antibiotic treatment strategies for community-acquired pneumonia in adults. N Engl J Med. 2015; 372:1312–1323.7. Garin N, Genné D, Carballo S, Chuard C, Eich G, Hugli O, Lamy O, Nendaz M, Petignat PA, Perneger T, et al. β-lactam monotherapy vs β-lactam-macrolide combination treatment in moderately severe community-acquired pneumonia: a randomized noninferiority trial. JAMA Intern Med. 2014; 174:1894–1901.8. Emmet O’Brien M, Restrepo MI, Martin-Loeches I. Update on the combination effect of macrolide antibiotics in community-acquired pneumonia. Respir Investig. 2015; 53:201–209.9. Asadi L, Sligl WI, Eurich DT, Colmers IN, Tjosvold L, Marrie TJ, Majumdar SR. Macrolide-based regimens and mortality in hospitalized patients with community-acquired pneumonia: a systematic review and meta-analysis. Clin Infect Dis. 2012; 55:371–380.10. Sligl WI, Asadi L, Eurich DT, Tjosvold L, Marrie TJ, Majumdar SR. Macrolides and mortality in critically ill patients with community-acquired pneumonia: a systematic review and meta-analysis. Crit Care Med. 2014; 42:420–432.11. Lim WS, Baudouin SV, George RC, Hill AT, Jamieson C, Le Jeune I, Macfarlane JT, Read RC, Roberts HJ, Levy ML, et al. BTS guidelines for the management of community acquired pneumonia in adults: update 2009. Thorax. 2009; 64:Suppl 3. iii1–55.12. Song JH, Jung KS, Kang MW, Kim DJ, Pai H, Suh GY, Shim TS, Ahn JH, Ahn CM, Woo JH, et al. Treatment guidelines for community-acquired pneumonia in Korea: an evidence-based approach to appropriate antimicrobial therapy. Tuberc Respir Dis (Seoul). 2009; 67:281–302.13. Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses [Internet]. accessed on 27 December 2015. Available at http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.14. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011; 343:d5928.15. Adrie C, Schwebel C, Garrouste-Orgeas M, Vignoud L, Planquette B, Azoulay E, Kallel H, Darmon M, Souweine B, Dinh-Xuan AT, et al. Initial use of one or two antibiotics for critically ill patients with community-acquired pneumonia: impact on survival and bacterial resistance. Crit Care. 2013; 17:R265.16. Bratzler DW, Ma A, Nsa W. Initial antibiotic selection and patient outcomes: observations from the National Pneumonia Project. Clin Infect Dis. 2008; 47:Suppl 3. S193–201.17. Karhu J, Ala-Kokko TI, Ohtonen P, Syrjälä H. Severe community-acquired pneumonia treated with beta-lactam-respiratory quinolone vs. beta-lactam-macrolide combination. Acta Anaesthesiol Scand. 2013; 57:587–593.18. Martin-Loeches I, Lisboa T, Rodriguez A, Putensen C, Annane D, Garnacho-Montero J, Restrepo MI, Rello J. Combination antibiotic therapy with macrolides improves survival in intubated patients with community-acquired pneumonia. Intensive Care Med. 2010; 36:612–620.19. Mortensen EM, Restrepo MI, Anzueto A, Pugh J. The impact of empiric antimicrobial therapy with a beta-lactam and fluoroquinolone on mortality for patients hospitalized with severe pneumonia. Crit Care. 2005; 10:R8.20. Waterer GW, Somes GW, Wunderink RG. Monotherapy may be suboptimal for severe bacteremic pneumococcal pneumonia. Arch Intern Med. 2001; 161:1837–1842.21. Wilson BZ, Anzueto A, Restrepo MI, Pugh MJ, Mortensen EM. Comparison of two guideline-concordant antimicrobial combinations in elderly patients hospitalized with severe community-acquired pneumonia. Crit Care Med. 2012; 40:2310–2314.22. Gaillat J, Bru JP, Sedallian A. Penicillin G/ofloxacin versus erythromycin/amoxicillin-clavulanate in the treatment of severe community-acquired pneumonia. Eur J Clin Microbiol Infect Dis. 1994; 13:639–644.23. Metersky ML, Ma A, Houck PM, Bratzler DW. Antibiotics for bacteremic pneumonia: Improved outcomes with macrolides but not fluoroquinolones. Chest. 2007; 131:466–473.24. Arnold FW, Summersgill JT, Lajoie AS, Peyrani P, Marrie TJ, Rossi P, Blasi F, Fernandez P, File TM Jr, Rello J, et al. A worldwide perspective of atypical pathogens in community-acquired pneumonia. Am J Respir Crit Care Med. 2007; 175:1086–1093.25. Afshar M, Foster CL, Layden JE, Burnham EL. Azithromycin use and outcomes in severe sepsis patients with and without pneumonia. J Crit Care. 2016; 32:120–125.26. Ginsburg AS, Grosset JH, Bishai WR. Fluoroquinolones, tuberculosis, and resistance. Lancet Infect Dis. 2003; 3:432–442.27. Long R, Chong H, Hoeppner V, Shanmuganathan H, Kowalewska-Grochowska K, Shandro C, Manfreda J, Senthilselvan A, Elzainy A, Marrie T. Empirical treatment of community-acquired pneumonia and the development of fluoroquinolone-resistant tuberculosis. Clin Infect Dis. 2009; 48:1354–1360.28. Cheng YJ, Nie XY, Chen XM, Lin XX, Tang K, Zeng WT, Mei WY, Liu LJ, Long M, Yao FJ, et al. The role of macrolide antibiotics in increasing cardiovascular risk. J Am Coll Cardiol. 2015; 66:2173–2184.29. Hong KB, Choi EH, Lee HJ, Lee SY, Cho EY, Choi JH, Kang HM, Lee J, Ahn YM, Kang YH, et al. Macrolide resistance of Mycoplasma pneumoniae, South Korea, 2000-2011. Emerg Infect Dis. 2013; 19:1281–1284.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Community Acquired Pneumonia
- Current perspectives on atypical pneumonia in children
- The Etiologies and Initial Antimicrobial Therapy Outcomes in One Tertiary Hospital ICU-admitted Patient with Severe Community- acquired Pneumonia
- Prolonged versus Intermittent Infusion of β-Lactams for the Treatment of Nosocomial Pneumonia: A Meta-Analysis
- Antibiotic Resistance and Treatment Update of Community-Acquired Pneumonia