Investig Magn Reson Imaging.
2018 Jun;22(2):123-130. 10.13104/imri.2018.22.2.123.
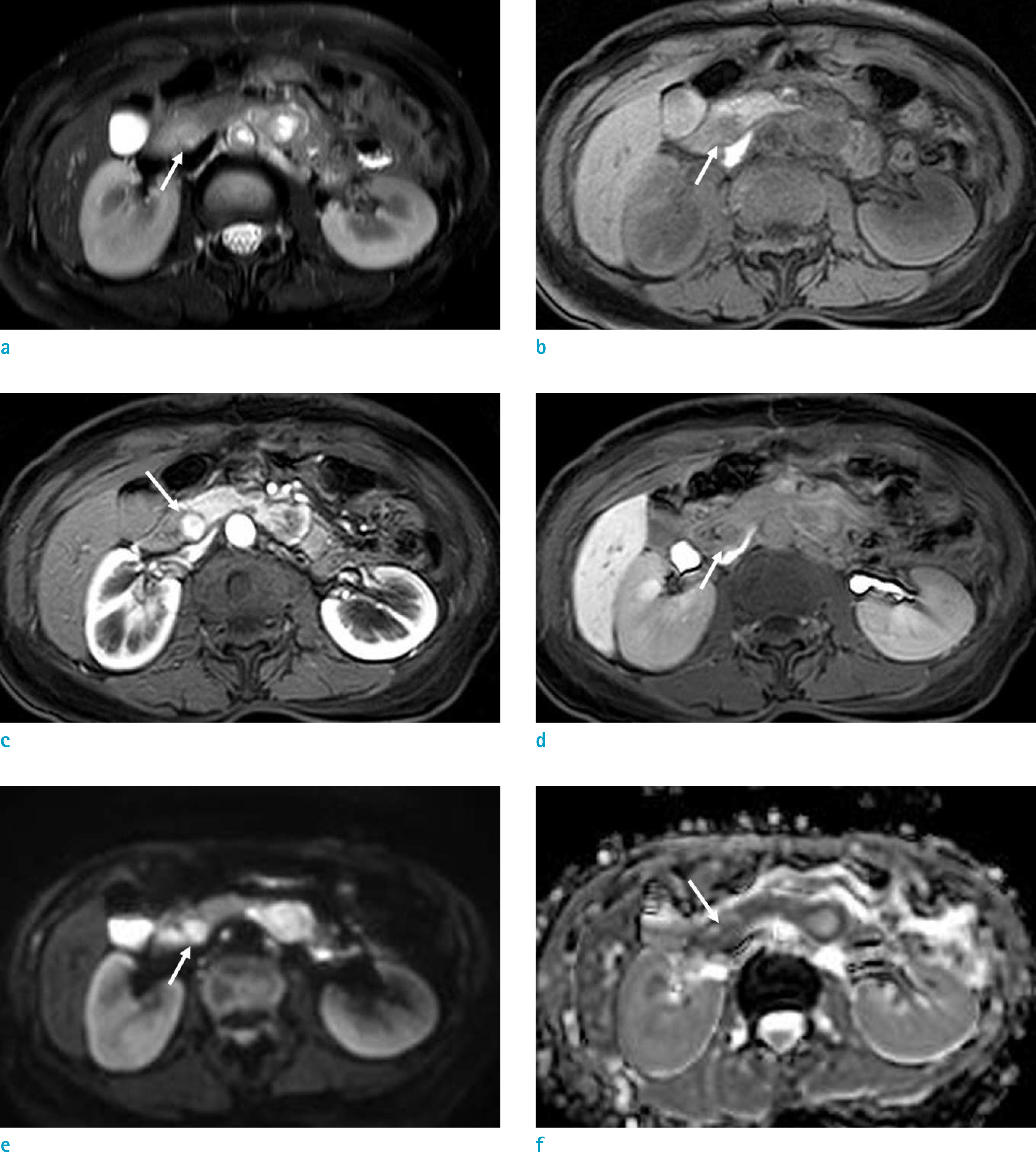
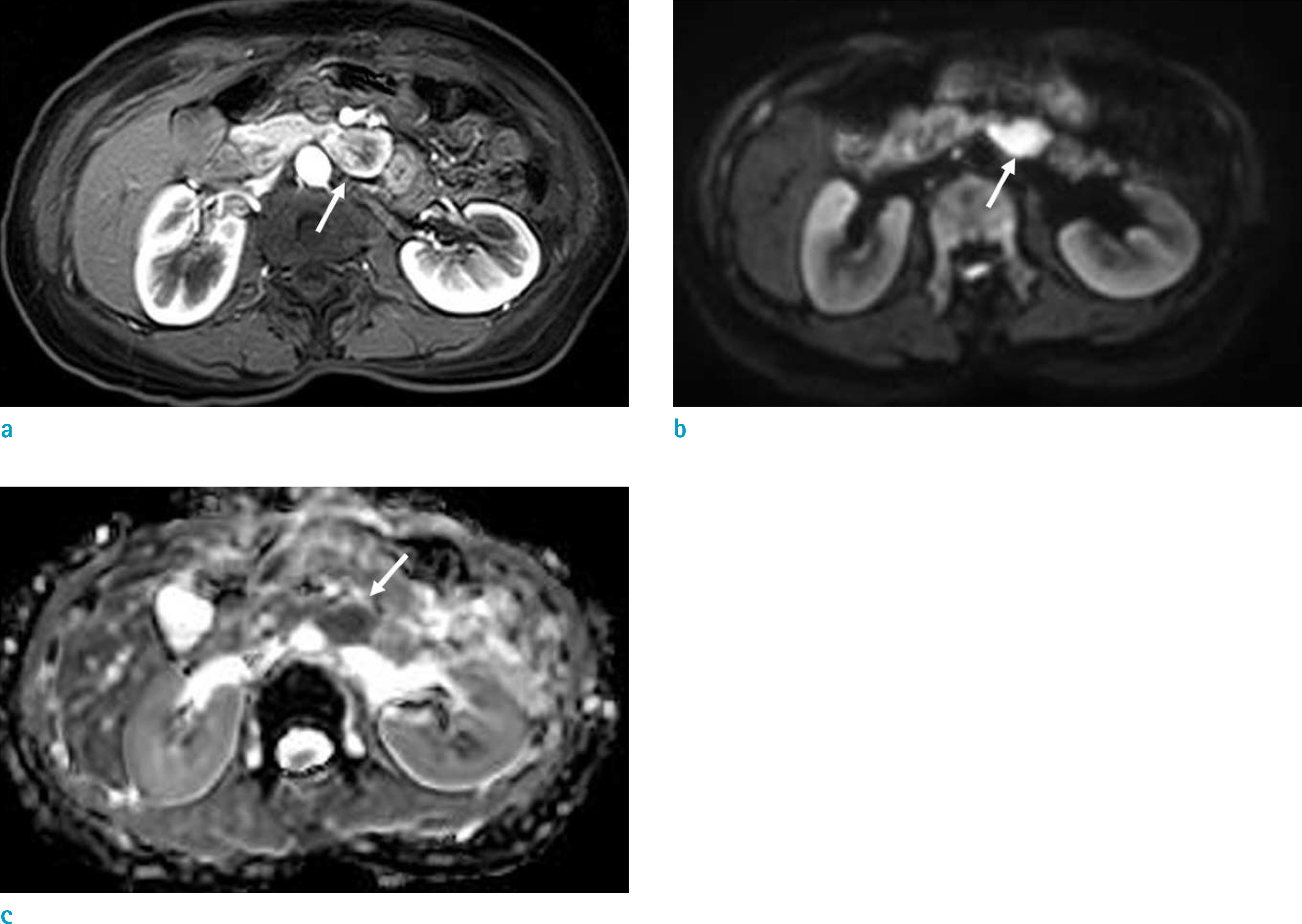
MRI Findings of an Ampulla of Vater Neuroendocrine Tumor with Liver and Lymph Node Metastasis: a Case Report
- Affiliations
-
- 1Department of Radiology, Dankook University Hospital, Dankook University School of Medicine, Cheonan, Korea. deepva@hanmail.net
- 2Department of Pathology, Dankook University Hospital, Dankook University School of Medicine, Cheonan, Korea.
- KMID: 2415892
- DOI: http://doi.org/10.13104/imri.2018.22.2.123
Abstract
- An ampulla of Vater neuroendocrine tumor (AOV-NET) is a rare subset of gastroenteropancreatic neuroendocrine tumors (GEP-NETs). Very few studies have been undertaken regarding MRI findings of an AOV-NET. We report on a case of a 59-year-old woman diagnosed with an AOV-NET with liver and lymph node metastasis, with an emphasis on the MRI findings. This case shows rare and precious typical MRI findings of an AOV-NET. The MRI visualized the AOV-NET very well and is helpful for the differentiation of an AOV-NET from other tumors in the ampullary area as well as with treatment planning.
MeSH Terms
Figure
Reference
-
References
1. Sahani DV, Bonaffini PA, Fernandez-Del Castillo C, Blake MA. Gastroenteropancreatic neuroendocrine tumors: role of imaging in diagnosis and management. Radiology. 2013; 266:38–61.
Article2. Jayant M, Punia R, Kaushik R, et al. Neuroendocrine tumors of the ampulla of vater: presentation, pathology and prognosis. JOP. 2012; 13:263–267.3. Carter JT, Grenert JP, Rubenstein L, Stewart L, Way LW. Neuroendocrine tumors of the ampulla of Vater: biological behavior and surgical management. Arch Surg. 2009; 144:527–531.4. Dumitrascu T, Dima S, Herlea V, Tomulescu V, Ionescu M, Popescu I. Neuroendocrine tumours of the ampulla of Vater: clinicopathological features, surgical approach and assessment of prognosis. Langenbecks Arch Surg. 2012; 397:933–943.
Article5. Yang K, Yun SP, Kim S, Shin N, Park DY, Seo HI. Clinicopathological features and surgical outcomes of neuroendocrine tumors of ampulla of Vater. BMC Gastroenterol. 2017; 17:70.
Article6. Raman SP, Fishman EK. Abnormalities of the distal common bile duct and ampulla: diagnostic approach and differential diagnosis using multiplanar reformations and 3D imaging. AJR Am J Roentgenol. 2014; 203:17–28.
Article7. Lewis RB, Lattin GE Jr, Paal E. Pancreatic endocrine tumors: radiologic-clinicopathologic correlation. Radiographics. 2010; 30:1445–1464.
Article8. Tsukagoshi M, Hosouchi Y, Araki K, et al. Neuroendocrine tumor of the ampulla of Vater with distant cystic lymph node metastasis: a case report. Surg Case Rep. 2016; 2:73.
Article9. Saeed A, Buell JF, Kandil E. Surgical treatment of liver metastases in patients with neuroendocrine tumors. Ann Transl Med. 2013; 1:6.10. Dromain C, de Baere T, Baudin E, et al. MR imaging of hepatic metastases caused by neuroendocrine tumors: comparing four techniques. AJR Am J Roentgenol. 2003; 180:121–128.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of a Collision Tumor in the Ampulla of Vater with an Adenocarcinoma and a Large Cell Neuroendocrine Carcinoma
- Prognostic value of the lymph node metastasis in patients with ampulla of Vater cancer after surgical resection
- Collision tumor of the ampulla of Vater - Coexistence of neuroendocrine carcinoma and adenocarcinoma: report of a case
- Computed Tomographic Findings of the Carcinoma of the Ampulla of Vater
- Carcinoid of the Ampulla of Vater: A Case Report