J Clin Neurol.
2018 Jul;14(3):333-338. 10.3988/jcn.2018.14.3.333.
Efficacy of Gaze Photographs in Diagnosing Ocular Myasthenia Gravis
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University College of Medicine, Seoul, Korea. hjm@snu.ac.kr
- 2Department of Ophthalmology, Seoul Metropolitan Government Seoul National University Boramae Medical Center, Seoul, Korea.
- 3Department of Neurology, Seoul National University College of Medicine, Seoul, Korea.
- 4Department of Neurology, Seoul National University Bundang Hospital, Seongnam, Korea.
- 5Department of Ophthalmology, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 2415049
- DOI: http://doi.org/10.3988/jcn.2018.14.3.333
Abstract
- BACKGROUND AND PURPOSE
The various tests that are routinely used to diagnose generalized myasthenia gravis, such as the edrophonium test, serum anti-acetylcholine-receptor antibodies (AChR-Ab), and repetitive nerve stimulation (RNS) tests, have lower diagnostic sensitivity in ocular myasthenia gravis (OMG). Diagnosing OMG becomes even more difficult when the clinical symptoms are subtle. There is no gold-standard diagnostic test available for OMG patients, and so this study compared the diagnostic sensitivity of gaze photographs with conventional tests in OMG.
METHODS
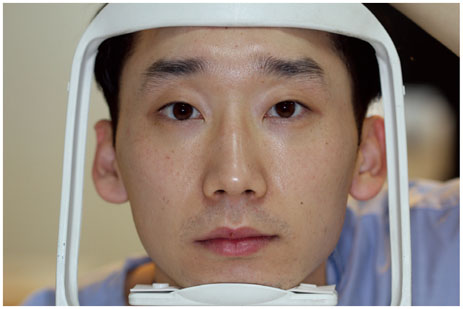
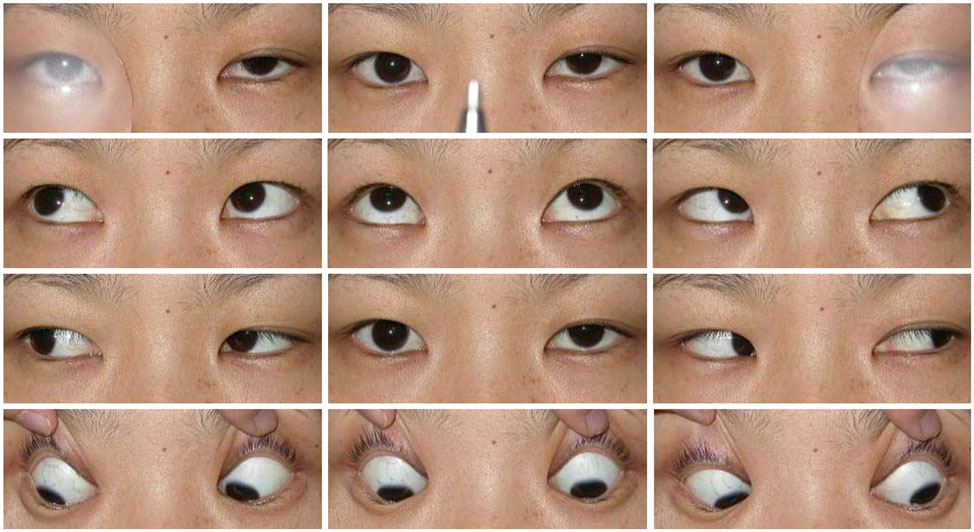
Records of gaze photographs were available for 25 of 31 consecutive patients diagnosed with OMG. Each patient underwent a neuro-ophthalmologic examination, serum AChR-Ab, RNS, edrophonium test, ice tests, and the acquisition of gaze photographs. The margin reflex distance 1 (MRD1) was measured on each of the gaze photographs, with MRD1 < 2 mm or an interlid MRD1 difference of ≥2 mm on any of the gaze photographs defined as a positive sign of OMG. The diagnostic sensitivities of the tests were assessed.
RESULTS
The mean age at onset was 38.5 years (range, 2-76 years), and 13 patients (52%) were men. The diagnostic sensitivities of the RNS test, AChR-Ab test, gaze photographs, and ice test were 56%, 64%, 80%, and 73%, respectively.
CONCLUSIONS
The diagnostic sensitivity was higher for gaze photographs than for the other tests applied to OMG patients.
MeSH Terms
Figure
Cited by 1 articles
-
Pattern of Extraocular Muscle Involvements in Miller Fisher Syndrome
Won Yeol Ryu, Yoo Hwan Kim, Byeol-A Yoon, Hwan Tae Park, Jong Seok Bae, Jong Kuk Kim
J Clin Neurol. 2019;15(3):308-312. doi: 10.3988/jcn.2019.15.3.308.
Reference
-
1. Weinberg DA, Lesser RL, Vollmer TL. Ocular myasthenia: a protean disorder. Surv Ophthalmol. 1994; 39:169–210.
Article2. Kusner LL, Puwanant A, Kaminski HJ. Ocular myasthenia: diagnosis, treatment, and pathogenesis. Neurologist. 2006; 12:231–239.3. Palace J, Vincent A, Beeson D. Myasthenia gravis: diagnostic and management dilemmas. Curr Opin Neurol. 2001; 14:583–589.
Article4. Luchanok U, Kaminski HJ. Ocular myasthenia: diagnostic and treatment recommendations and the evidence base. Curr Opin Neurol. 2008; 21:8–15.
Article5. Benatar M. A systematic review of diagnostic studies in myasthenia gravis. Neuromuscul Disord. 2006; 16:459–467.
Article6. Padua L, Stalberg E, LoMonaco M, Evoli A, Batocchi A, Tonali P. SFEMG in ocular myasthenia gravis diagnosis. Clin Neurophysiol. 2000; 111:1203–1207.
Article7. Barton JJ, Fouladvand M. Ocular aspects of myasthenia gravis. Semin Neurol. 2000; 20:7–20.
Article8. Park JY, Yang HK, Hwang JM. Diagnostic value of repeated ice tests in the evaluation of ptosis in myasthenia gravis. PLoS One. 2017; 12:e0177078.
Article9. Kim JH, Hwang JM, Hwang YS, Kim KJ, Chae J. Childhood ocular myasthenia gravis. Ophthalmology. 2003; 110:1458–1462.
Article10. Oh SJ. Electromyography: Neuromuscular Transmission Studies. Baltimore: Williams & Wilkins;1988. p. 1–304.11. Putterman AM. Margin reflex distance (MRD) 1, 2, and 3. Ophthalmic Plast Reconstr Surg. 2012; 28:308–311.
Article12. Jun AK, Ahn CS. [MA statistical evaluation of the average value of margin reflex distance I and margin limbal distance in Koreans]. J Korean Ophthalmol Soc. 1990; 31:1243–1248.13. Boboridis K, Assi A, Indar A, Bunce C, Tyers AG. Repeatability and reproducibility of upper eyelid measurements. Br J Ophthalmol. 2001; 85:99–101.
Article14. Small RG, Sabates NR, Burrows D. The measurement and definition of ptosis. Ophthalmic Plast Reconstr Surg. 1989; 5:171–175.
Article15. Parmar DN, Rose GE. Fundamentals of oculoplastic surgery. In : Chen WP, editor. Oculoplastic Surgery: the Essentials. 1st ed. New York: Thieme;2001. p. 512.16. Cruz AA, Lucchezi MC. Quantification of palpebral fissure shape in severe congenital blepharoptosis. Ophthalmic Plast Reconstr Surg. 1999; 15:232–235.
Article17. Cruz AA, Coelho RP, Baccega A, Lucchezi MC, Souza AD, Ruiz EE. Digital image processing measurement of the upper eyelid contour in Graves disease and congenital blepharoptosis. Ophthalmology. 1998; 105:913–918.
Article18. Flowers RS, Flowers SS. Diagnosing photographic distortion. decoding true postoperative contour after eyelid surgery. Clin Plast Surg. 1993; 20:387–392.19. Choi CJ, Chou JC, Lefebvre DR, Yoon MK. Margin reflex distance: differences based on camera and flash positions. Ophthalmic Plast Reconstr Surg. 2016; 32:199–203.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Severe Ocular Myasthenia Gravis that Developed Total External Ophthalmoplegia
- A case of Graves' disease associated with ocular myasthenia gravis
- Fecal Incontinence as a Symptom of Myasthenia Gravis
- A Case of Ocular Myasthenia Gravis Presenting as Double Depressor Palsy
- A Case of Ocular Myasthenia Associated with Graves's disease