J Clin Neurol.
2018 Jul;14(3):310-319. 10.3988/jcn.2018.14.3.310.
Sympathetic Overactivity Based on Heart-Rate Variability in Patients with Obstructive Sleep Apnea and Cerebral Small-Vessel Disease
- Affiliations
-
- 1Department of Neurology, Ewha Womans University School of Medicine and Ewha Medical Research Institute, Seoul, Korea. leeh@ewha.ac.kr
- 2Department of Medical Science, Ewha Womans University School of Medicine and Ewha Medical Research Institute, Seoul, Korea.
- 3Department of Neurology, Biomedical Research Institute, Seoul National University Hospital, Seoul, Korea.
- 4Department of Neurology, Heavenly Hospital, Goyang, Korea.
- KMID: 2415046
- DOI: http://doi.org/10.3988/jcn.2018.14.3.310
Abstract
- BACKGROUND AND PURPOSE
Obstructive sleep apnea (OSA) is associated with cerebral white-matter changes (WMC), but the underlying mechanisms are not completely understood. Our aim was to identify the cardiovascular autonomic characteristics during sleep that are associated with cerebral WMC in OSA patients.
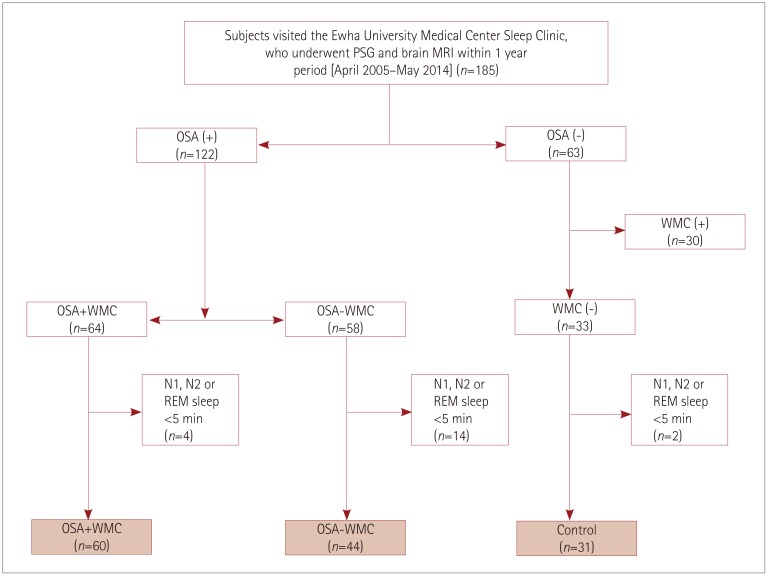
METHODS
We recruited subjects from our sleep-center database who underwent both polysomnography and brain MRI within a 1-year period. Sixty patients who had OSA with WMC (OSA+WMC), 44 patients who had OSA without WMC (OSA−WMC), and 31 control subjects who had neither OSA nor WMC were analyzed. Linear and nonlinear indices of heart-rate variability (HRV) were analyzed in each group according to different sleep stages and also over the entire sleeping period.
RESULTS
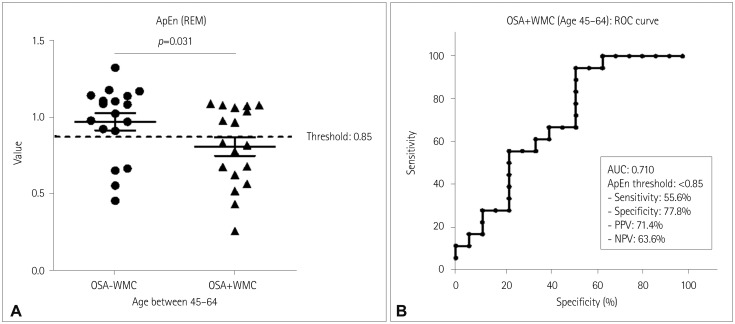
Among the nonlinear HRV indices, the Poincaré ratio (SD12) during the entire sleep period was significantly increased in the OSA+WMC group, even after age adjustment. Meanwhile, detrended fluctuation analysis 1 during non-rapid-eye-movement sleep tended to be lowest in the OSA+WMC group. These indices were altered regardless of the presence of hypertension or diabetes. In the subgroup analysis of middle-aged OSA patients, approximate entropy during rapid-eye-movement sleep was significantly lower in OSA+WMC patients than in OSA−WMC patients. Overall, the nonlinear HRV indices suggest that sympathetic activity was higher in the OSA+WMC group than in the OSA−WMC and control groups.
CONCLUSIONS
Our findings suggest that dysregulation of HRV, especially overactivation of sympathetic tone, could be a pathophysiologic mechanism underlying the development of WMC in OSA patients.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Interarm Blood Pressure Difference has Various Associations with the Presence and Burden of Cerebral Small-Vessel Diseases in Noncardioembolic Stroke Patients
Yoonkyung Chang, Seung Ah Lee, Sue Hyun Lee, Eun Hye Lee, Yong-Jae Kim, Tae-Jin Song
J Clin Neurol. 2019;15(2):159-167. doi: 10.3988/jcn.2019.15.2.159.
Reference
-
1. Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005; 353:2034–2041. PMID: 16282178.
Article2. Gonzaga C, Bertolami A, Bertolami M, Amodeo C, Calhoun D. Obstructive sleep apnea, hypertension and cardiovascular diseases. J Hum Hypertens. 2015; 29:705–712. PMID: 25761667.
Article3. Khoo MC, Kim TS, Berry RB. Spectral indices of cardiac autonomic function in obstructive sleep apnea. Sleep. 1999; 22:443–451. PMID: 10389220.
Article4. Palma JA, Urrestarazu E, Lopez-Azcarate J, Alegre M, Fernandez S, Artieda J, et al. Increased sympathetic and decreased parasympathetic cardiac tone in patients with sleep related alveolar hypoventilation. Sleep. 2013; 36:933–940. PMID: 23729937.
Article5. Eguchi K, Kario K, Hoshide S, Ishikawa J, Morinari M, Shimada K. Nocturnal hypoxia is associated with silent cerebrovascular disease in a high-risk Japanese community-dwelling population. Am J Hypertens. 2005; 18:1489–1495. PMID: 16280287.
Article6. Song TJ, Park JH, Choi KH, Chang Y, Moon J, Kim JH, et al. Moderate-to-severe obstructive sleep apnea is associated with cerebral small vessel disease. Sleep Med. 2017; 30:36–42. PMID: 28215260.
Article7. Nishibayashi M, Miyamoto M, Miyamoto T, Suzuki K, Hirata K. Correlation between severity of obstructive sleep apnea and prevalence of silent cerebrovascular lesions. J Clin Sleep Med. 2008; 4:242–247. PMID: 18595437.
Article8. Kamba M, Inoue Y, Higami S, Suto Y, Ogawa T, Chen W. Cerebral metabolic impairment in patients with obstructive sleep apnoea: an independent association of obstructive sleep apnoea with white matter change. J Neurol Neurosurg Psychiatry. 2001; 71:334–339. PMID: 11511706.
Article9. Kim H, Yun CH, Thomas RJ, Lee SH, Seo HS, Cho ER, et al. Obstructive sleep apnea as a risk factor for cerebral white matter change in a middle-aged and older general population. Sleep. 2013; 36:709B–715B. PMID: 23633753.
Article10. Pantoni L. Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol. 2010; 9:689–701. PMID: 20610345.
Article11. Tobaldini E, Nobili L, Strada S, Casali KR, Braghiroli A, Montano N. Heart rate variability in normal and pathological sleep. Front Physiol. 2013; 4:294. PMID: 24137133.
Article12. Tarvainen MP, Niskanen JP, Lipponen JA, Ranta-Aho PO, Karjalainen PA. Kubios HRV--heart rate variability analysis software. Comput Methods Programs Biomed. 2014; 113:210–220. PMID: 24054542.13. Bonnet MH, Arand DL. Heart rate variability: sleep stage, time of night, and arousal influences. Electroencephalogr Clin Neurophysiol. 1997; 102:390–396. PMID: 9191582.
Article14. Narkiewicz K, Pesek CA, Kato M, Phillips BG, Davison DE, Somers VK. Baroreflex control of sympathetic nerve activity and heart rate in obstructive sleep apnea. Hypertension. 1998; 32:1039–1043. PMID: 9856970.
Article15. Stein PK, Domitrovich PP, Huikuri HV, Kleiger RE. Cast Investigators. Traditional and nonlinear heart rate variability are each independently associated with mortality after myocardial infarction. J Cardiovasc Electrophysiol. 2005; 16:13–20. PMID: 15673380.
Article16. Khan AA, Mumtahina U, Yeasmin N. Heart rate variability analysis using approximate entropy and detrended fluctuation for monitoring heart condition. Piscataway (NJ): IEEE;2013.17. Epstein LJ, Kristo D, Strollo PJ Jr, Friedman N, Malhotra A, Patil SP, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009; 5:263–276. PMID: 19960649.18. Song TJ, Park JH, Choi KH, Kim JH, Choi Y, Chang Y, et al. Is obstructive sleep apnea associated with the presence of intracranial cerebral atherosclerosis? Sleep Breath. 2017; 21:639–646. PMID: 28168435.
Article19. Song TJ, Cho HJ, Chang Y, Youn M, Shin MJ, Jo I, et al. Low-density-lipoprotein particle size predicts a poor outcome in patients with atherothrombotic stroke. J Clin Neurol. 2015; 11:80–86. PMID: 25628741.
Article20. Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA. MR signal abnormalities at 1.5 T in Alzheimer's dementia and normal aging. AJR Am J Roentgenol. 1987; 149:351–356. PMID: 3496763.
Article21. Berry RB, Brooks R, Gamaldo CE, Harding SM, Lioyd RM, Marcus CL, et al. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications, Version 2.1. Darien (IL): American Academy of Sleep Medicine;2014.22. Hoshi RA, Pastre CM, Vanderlei LC, Godoy MF. Poincaré plot indexes of heart rate variability: relationships with other nonlinear variables. Auton Neurosci. 2013; 177:271–274. PMID: 23755947.
Article23. Penzel T, Kantelhardt JW, Grote L, Peter JH, Bunde A. Comparison of detrended fluctuation analysis and spectral analysis for heart rate variability in sleep and sleep apnea. IEEE Trans Biomed Eng. 2003; 50:1143–1151. PMID: 14560767.
Article24. Palma JA, Iriarte J, Fernandez S, Valencia M, Alegre M, Artieda J, et al. Characterizing the phenotypes of obstructive sleep apnea: clinical, sleep, and autonomic features of obstructive sleep apnea with and without hypoxia. Clin Neurophysiol. 2014; 125:1783–1791. PMID: 24631013.
Article25. Fleisher LA, Pincus SM, Rosenbaum SH. Approximate entropy of heart rate as a correlate of postoperative ventricular dysfunction. Anesthesiology. 1993; 78:683–692. PMID: 8466069.
Article26. Beckers F, Verheyden B, Aubert AE. Aging and nonlinear heart rate control in a healthy population. Am J Physiol Heart Circ Physiol. 2006; 290:H2560–H2570. PMID: 16373585.
Article27. Antelmi I, de Paula RS, Shinzato AR, Peres CA, Mansur AJ, Grupi CJ. Influence of age, gender, body mass index, and functional capacity on heart rate variability in a cohort of subjects without heart disease. Am J Cardiol. 2004; 93:381–385. PMID: 14759400.
Article28. Smith EE, Saposnik G, Biessels GJ, Doubal FN, Fornage M, Gorelick PB, et al. Prevention of stroke in patients with silent cerebrovascular disease: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2017; 48:e44–e71. PMID: 27980126.
Article29. Wiklund U, Olofsson BO, Franklin K, Blom H, Bjerle P, Niklasson U. Autonomic cardiovascular regulation in patients with obstructive sleep apnoea: a study based on spectral analysis of heart rate variability. Clin Physiol. 2000; 20:234–241. PMID: 10792417.
Article30. Gula LJ, Krahn AD, Skanes A, Ferguson KA, George C, Yee R, et al. Heart rate variability in obstructive sleep apnea: a prospective study and frequency domain analysis. Ann Noninvasive Electrocardiol. 2003; 8:144–149. PMID: 12848796.
Article31. Lado MJ, Méndez AJ, Rodríguez-Liñares L, Otero A, Vila XA. Nocturnal evolution of heart rate variability indices in sleep apnea. Comput Biol Med. 2012; 42:1179–1185. PMID: 23084286.
Article32. Busek P, Vanková J, Opavský J, Salinger J, Nevsímalová S. Spectral analysis of heart rate variability in sleep. Physiol Res. 2005; 54:369–376. PMID: 15588154.33. Mäkikallio TH, Tapanainen JM, Tulppo MP, Huikuri HV. Clinical applicability of heart rate variability analysis by methods based on nonlinear dynamics. Card Electrophysiol Rev. 2002; 6:250–255. PMID: 12114847.34. Jons C, Raatikainen P, Gang UJ, Huikuri HV, Joergensen RM, Johannesen A, et al. Autonomic dysfunction and new-onset atrial fibrillation in patients with left ventricular systolic dysfunction after acute myocardial infarction: a CARISMA substudy. J Cardiovasc Electrophysiol. 2010; 21:983–990. PMID: 20487120.
Article35. Tulppo MP, Mäkikallio TH, Seppänen T, Airaksinen JK, Huikuri HV. Heart rate dynamics during accentuated sympathovagal interaction. Am J Physiol. 1998; 274:H810–H816. PMID: 9530192.36. Tulppo MP, Mäkikallio TH, Seppänen T, Shoemaker K, Tutungi E, Hughson RL, et al. Effects of pharmacological adrenergic and vagal modulation on fractal heart rate dynamics. Clin Physiol. 2001; 21:515–523. PMID: 11576151.
Article37. Kato M, Roberts-Thomson P, Phillips BG, Haynes WG, Winnicki M, Accurso V, et al. Impairment of endothelium-dependent vasodilation of resistance vessels in patients with obstructive sleep apnea. Circulation. 2000; 102:2607–2610. PMID: 11085964.
Article38. Hoth KF, Tate DF, Poppas A, Forman DE, Gunstad J, Moser DJ, et al. Endothelial function and white matter hyperintensities in older adults with cardiovascular disease. Stroke. 2007; 38:308–312. PMID: 17204686.
Article39. Oka N, Akiguchi I, Matsubayashi K, Kameyama M, Maeda T, Kawamura J. Density of sympathetic nerve terminals in human superficial temporal arteries: potassium permanganate fixation and monoamine oxidase histochemistry. Stroke. 1987; 18:229–233. PMID: 2433818.
Article40. Peppiatt CM, Howarth C, Mobbs P, Attwell D. Bidirectional control of CNS capillary diameter by pericytes. Nature. 2006; 443:700–704. PMID: 17036005.
Article41. Limphanudom P, Chierakul N, Pinyopattarakul N, Nana A, Naruman C, Tangchityongsiva S, et al. Recovery of heart rate variability in patients with moderate to severe obstructive sleep apnea after 6-month continuous positive airway pressure treatment. J Med Assoc Thai. 2007; 90:1530–1535. PMID: 17926981.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Complications of Obstructive Sleep Apnea
- A Classifying Model of Obstructive Sleep Apnea Based on Heart Rate Variability in a Large Korean Population
- The Effect of Aging and Severity of Sleep Apnea on Heart Rate Variability Indices in Obstructive Sleep Apnea Syndrome
- Renal Denervation for Chronic Heart Failure: Background and Pathophysiological Rationale
- Surgical Treatment of Adult Obstructive Sleep Apnea