Korean Circ J.
2018 May;48(5):395-405. 10.4070/kcj.2017.0324.
Comparative Cardiovascular Risks of Dipeptidyl Peptidase-4 Inhibitors: Analyses of Real-world Data in Korea
- Affiliations
-
- 1Department of Endocrinology and Metabolism, Ajou University School of Medicine, Suwon, Korea. djkim@ajou.ac.kr
- 2Cardiovascular and Metabolic Disease Etiology Research Center, Ajou University School of Medicine, Suwon, Korea.
- 3Department of Statistics and Actuarial Science, Soongsil University, Seoul, Korea.
- 4Department of Biostatistics, Yonsei University College of Medicine, Seoul, Korea.
- 5Department of Preventive Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 6Cardiovascular and Metabolic Disease Etiology Research Center, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2414908
- DOI: http://doi.org/10.4070/kcj.2017.0324
Abstract
- BACKGROUND AND OBJECTIVES
To compare cardiovascular disease (CVD) risk associated with 5 different dipeptidyl peptidase-4 inhibitors (DPP-4is) in people with type 2 diabetes.
METHODS
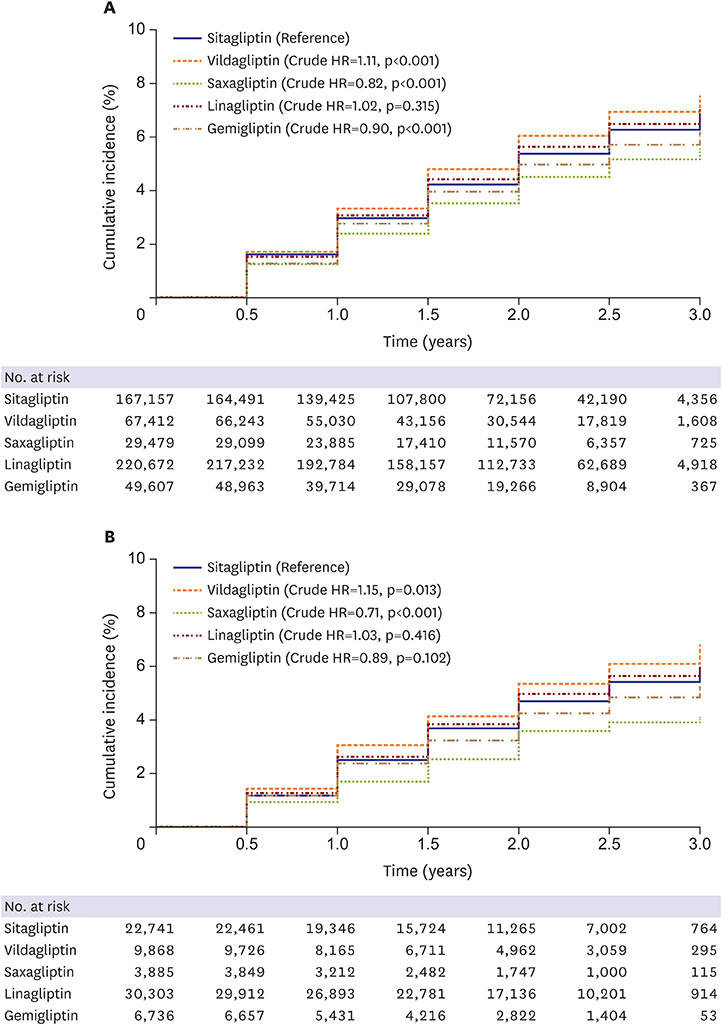
We identified 534,327 people who were newly prescribed sitagliptin (n=167,157), vildagliptin (n=67,412), saxagliptin (n=29,479), linagliptin (n=220,672), or gemigliptin (n=49,607) between January 2013 and June 2015 using the claims database of the Korean National Health Insurance System. A Cox proportional hazards model was used to estimate hazard ratios (HRs) for major CVD events (myocardial infarction, stroke, or death) among users of different DPP-4is. The model was adjusted for sex, age, duration of DPP-4i use, use of other glucose-lowering drugs, use of antiplatelet agents, hypertension, dyslipidemia, atrial fibrillation, chronic kidney disease, microvascular complications of diabetes, Charlson comorbidity index, and the calendar index year as potential confounders.
RESULTS
Compared to sitagliptin users, the fully adjusted HRs for CVD events were 0.97 (95% confidence interval [CI], 0.94-1.01; p=0.163) for vildagliptin, 0.76 (95% CI, 0.71-0.81; p < 0.001) for saxagliptin, 0.95 (95% CI, 0.92-0.98; p < 0.001) for linagliptin, and 0.84 (95% CI, 0.80-0.88; p < 0.001) for gemigliptin.
CONCLUSIONS
Compared to sitagliptin therapy, saxagliptin, linagliptin, and gemigliptin therapies were all associated with a lower risk of cardiovascular events.
MeSH Terms
-
Atrial Fibrillation
Cardiovascular Diseases
Comorbidity
Diabetes Mellitus, Type 2
Dipeptidyl-Peptidase IV Inhibitors
Dyslipidemias
Hypertension
Infarction
Korea*
Linagliptin
National Health Programs
Platelet Aggregation Inhibitors
Proportional Hazards Models
Renal Insufficiency, Chronic
Sitagliptin Phosphate
Stroke
Dipeptidyl-Peptidase IV Inhibitors
Linagliptin
Platelet Aggregation Inhibitors
Sitagliptin Phosphate
Figure
Cited by 3 articles
-
Cardiovascular Research Using the Korean National Health Information Database
Eue-Keun Choi
Korean Circ J. 2020;50(9):754-772. doi: 10.4070/kcj.2020.0171.Effect of Dipeptidyl Peptidase-4 Inhibitors on Cardiovascular Outcome
Kwang-il Kim
Korean Circ J. 2018;48(5):430-432. doi: 10.4070/kcj.2018.0085.Effect of Teneligliptin versus Sulfonylurea on Major Adverse Cardiovascular Outcomes in People with Type 2 Diabetes Mellitus: A Real-World Study in Korea
Da Hea Seo, Kyoung Hwa Ha, So Hun Kim, Dae Jung Kim
Endocrinol Metab. 2021;36(1):70-80. doi: 10.3803/EnM.2020.777.
Reference
-
1. Kim JH, Kim DJ, Jang HC, Choi SH. Epidemiology of micro- and macrovascular complications of type 2 diabetes in Korea. Diabetes Metab J. 2011; 35:571–577.
Article2. Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2015; 38:140–149.3. Monami M, Ahrén B, Dicembrini I, Mannucci E. Dipeptidyl peptidase-4 inhibitors and cardiovascular risk: a meta-analysis of randomized clinical trials. Diabetes Obes Metab. 2013; 15:112–120.4. Morgan CL, Mukherjee J, Jenkins-Jones S, Holden SE, Currie CJ. Combination therapy with metformin plus sulphonylureas versus metformin plus DPP-4 inhibitors: association with major adverse cardiovascular events and all-cause mortality. Diabetes Obes Metab. 2014; 16:977–983.
Article5. Ou HT, Chang KC, Li CY, Wu JS. Comparative cardiovascular risks of dipeptidyl peptidase 4 inhibitors with other second- and third-line antidiabetic drugs in patients with type 2 diabetes. Br J Clin Pharmacol. 2017; 83:1556–1570.
Article6. Ha KH, Kim B, Choi H, Kim DJ, Kim HC. Cardiovascular events associated with second-line anti-diabetes treatments: analysis of real-world Korean data. Diabet Med. 2017; 34:1235–1243.
Article7. Deacon CF. Dipeptidyl peptidase-4 inhibitors in the treatment of type 2 diabetes: a comparative review. Diabetes Obes Metab. 2011; 13:7–18.
Article8. Green JB, Bethel MA, Armstrong PW, et al. Effect of sitagliptin on cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2015; 373:232–242.
Article9. Zannad F, Cannon CP, Cushman WC, et al. Heart failure and mortality outcomes in patients with type 2 diabetes taking alogliptin versus placebo in EXAMINE: a multicentre, randomised, double-blind trial. Lancet. 2015; 385:2067–2076.
Article10. Scirica BM, Bhatt DL, Braunwald E, et al. Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N Engl J Med. 2013; 369:1317–1326.
Article11. Fu AZ, Johnston SS, Ghannam A, et al. Association between hospitalization for heart failure and dipeptidyl peptidase 4 inhibitors in patients with type 2 diabetes: an observational study. Diabetes Care. 2016; 39:726–734.
Article12. Suh S, Seo GH, Jung CH, et al. Increased risk of hospitalization for heart failure with newly prescribed dipeptidyl peptidase-4 inhibitors and pioglitazone using the Korean Health Insurance Claims Database. Diabetes Metab J. 2015; 39:247–252.
Article13. Toh S, Hampp C, Reichman ME, et al. Risk for hospitalized heart failure among new users of saxagliptin, sitagliptin, and other antihyperglycemic drugs: a retrospective cohort study. Ann Intern Med. 2016; 164:705–714.14. Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005; 43:1130–1139.
Article15. Eurich DT, Simpson S, Senthilselvan A, Asche CV, Sandhu-Minhas JK, McAlister FA. Comparative safety and effectiveness of sitagliptin in patients with type 2 diabetes: retrospective population based cohort study. BMJ. 2013; 346:f2267.
Article16. Kim JH, Kim SS, Baek HS, et al. Comparison of vildagliptin and pioglitazone in Korean patients with type 2 diabetes inadequately controlled with metformin. Diabetes Metab J. 2016; 40:230–239.
Article17. Williams R, de Vries F, Kothny W, et al. Cardiovascular safety of vildagliptin in patients with type 2 diabetes: a European multi-database, non-interventional post-authorization safety study. Diabetes Obes Metab. 2017; 19:1473–1478.
Article18. Gallwitz B, Rosenstock J, Rauch T, et al. 2-year efficacy and safety of linagliptin compared with glimepiride in patients with type 2 diabetes inadequately controlled on metformin: a randomised, double-blind, non-inferiority trial. Lancet. 2012; 380:475–483.
Article19. Kim SH, Yoo JH, Lee WJ, Park CY. Gemigliptin: an update of its clinical use in the management of type 2 diabetes mellitus. Diabetes Metab J. 2016; 40:339–353.
Article20. Cobble ME, Frederich R. Saxagliptin for the treatment of type 2 diabetes mellitus: assessing cardiovascular data. Cardiovasc Diabetol. 2012; 11:6.
Article21. Engel SS, Golm GT, Shapiro D, Davies MJ, Kaufman KD, Goldstein BJ. Cardiovascular safety of sitagliptin in patients with type 2 diabetes mellitus: a pooled analysis. Cardiovasc Diabetol. 2013; 12:3.
Article22. Ferrannini E, DeFronzo RA. Impact of glucose-lowering drugs on cardiovascular disease in type 2 diabetes. Eur Heart J. 2015; 36:2288–2296.
Article23. Johansen OE, Neubacher D, von Eynatten M, Patel S, Woerle HJ. Cardiovascular safety with linagliptin in patients with type 2 diabetes mellitus: a pre-specified, prospective, and adjudicated meta-analysis of a phase 3 programme. Cardiovasc Diabetol. 2012; 11:3.
Article24. Schweizer A, Dejager S, Foley JE, Couturier A, Ligueros-Saylan M, Kothny W. Assessing the cardio-cerebrovascular safety of vildagliptin: meta-analysis of adjudicated events from a large Phase III type 2 diabetes population. Diabetes Obes Metab. 2010; 12:485–494.
Article25. Vanderheyden M, Bartunek J, Goethals M, et al. Dipeptidyl-peptidase IV and B-type natriuretic peptide. From bench to bedside. Clin Chem Lab Med. 2009; 47:248–252.
Article26. Anagnostis P, Athyros VG, Adamidou F, et al. Glucagon-like peptide-1-based therapies and cardiovascular disease: looking beyond glycaemic control. Diabetes Obes Metab. 2011; 13:302–312.
Article27. Saraiva FK, Sposito AC. Cardiovascular effects of glucagon-like peptide 1 (GLP-1) receptor agonists. Cardiovasc Diabetol. 2014; 13:142.
Article28. Scirica BM. The safety of dipeptidyl peptidase 4 Inhibitors and the risk for heart failure. JAMA Cardiol. 2016; 1:123–125.
Article29. Kimm H, Yun JE, Lee SH, Jang Y, Jee SH. Validity of the diagnosis of acute myocardial infarction in Korean National Medical Health Insurance claims data: the Korean heart study (1). Korean Circ J. 2012; 42:10–15.
Article30. Park JK, Kim KS, Kim CB, et al. The accuracy of ICD codes for cerebrovascular diseases in medical insurance claims. Korean J Prev Med. 2000; 33:76–82.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Dipeptidyl Peptidase-4 Inhibitors on Cardiovascular Outcome
- Emerging Safety Issues of Dipeptidyl Peptidase-4 Inhibitors and Sodium Glucose Cotransporter 2 Inhibitors: How to Interpret and Apply in Clinical Practice
- Effect of DPP-4 Inhibitors on the Cardiovascular System, Cancer and Pancreatitis
- Dipeptidyl Peptidase 4 Inhibitor, an Update
- Effect of Sodium-Glucose Cotransporter-2 Inhibitors versus Dipeptidyl Peptidase 4 Inhibitors on Cardiovascular Function in Patients with Type 2 Diabetes Mellitus and Coronary Artery Disease