Ann Surg Treat Res.
2018 Jul;95(1):7-15. 10.4174/astr.2018.95.1.7.
Meta-analysis of randomized controlled trials on the efficacy of daikenchuto on improving intestinal dysfunction after abdominal surgery
- Affiliations
-
- 1Guangdong Provincial Key Laboratory of Malignant Tumor Epigenetics and Gene Regulation and Department of Biliary-Pancreatic Surgery, Sun Yat-sen Memorial Hospital, Sun Yat-sen University, Guangzhou, China. leiboxumd@163.com
- 2Department of Hepatic Surgery, The Third Affiliated Hospital, Sun Yat-sen University, Guangzhou, China.
- 3Department of Orthopaedics, The Fifth Affiliated Hospital of Sun Yat-Sen University, Guangzhou, China.
- 4Laboratory Animal Center, Sun Yat-sen University, Guangzhou, China.
- 5International Pacific Research Center, University of Hawaii at Manoa, Honolulu, HI, USA.
- KMID: 2414447
- DOI: http://doi.org/10.4174/astr.2018.95.1.7
Abstract
- PURPOSE
Intestinal dysfunction is one of the most common complications in patients after abdominal surgery. Daikenchuto (DKT), a traditional herbal medicine, is recently employed to improve postoperative intestinal dysfunction. The aim of this meta-analysis was to assess the efficacy of DKT in improving intestinal dysfunction after abdominal surgery.
METHODS
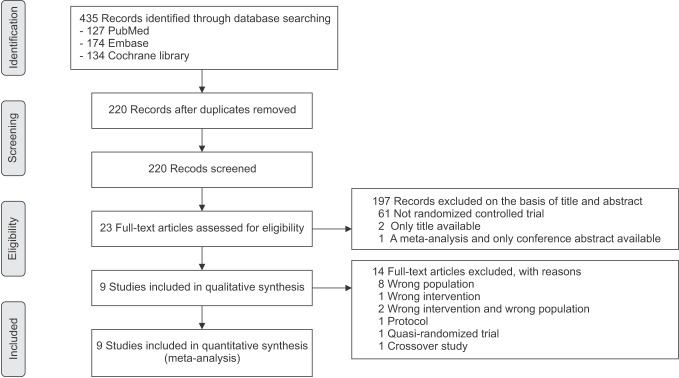
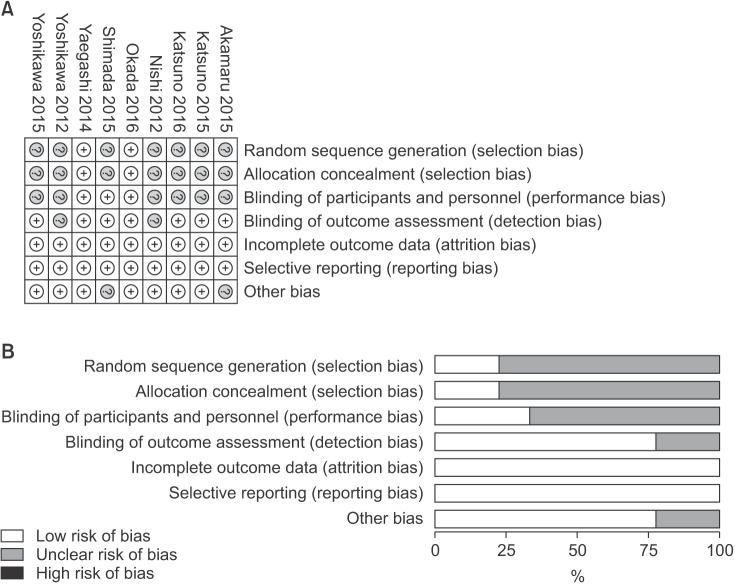
PubMed, Embase, and the Cochrane library were systematically searched to identify randomized controlled trails (RCTs) in adult patients undergoing abdominal surgery, who were randomly distributed to administrate DKT and placebo. The primary outcomes included the time to first postoperative flatus or bowel movement. We used random-effects models to calculate summary mean differences (MDs) with 95% confidence intervals (CIs).
RESULTS
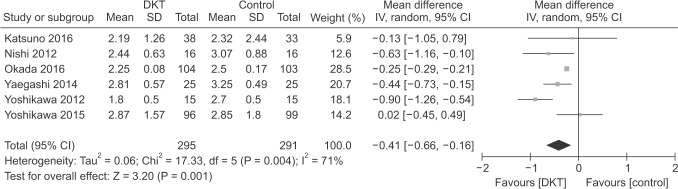
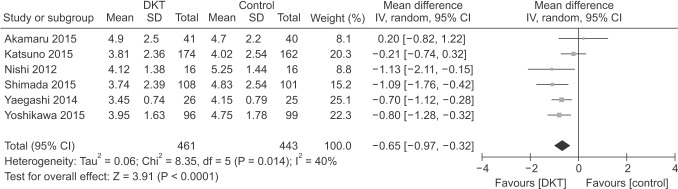
Nine RCTs totaling 1,212 patients (618 in DKT, 594 in control group) were included in our study. Compared with control group, DKT can effectively improve postoperative intestinal dysfunction by shortening the time to first postoperative flatus (MD, −0.41; 95% confidence interval [CI], −0.66 to −0.16; P = 0.001) with significant heterogeneity (I2 = 71%, P = 0.004), and bowel movement (MD, −0.65; 95% CI, −0.97 to −0.32; P < 0.001) without significant heterogeneity (I2 = 40%, P = 0.14). Sensitivity analyses by indication of surgery and type of surgery yielded similar results.
CONCLUSION
These data provide limited evidence that DKT shows efficacy on improving intestinal dysfunction after abdominal surgery. However, the results should be interpreted cautiously, due to the heterogeneity of the studies included. Thus, the efficacy of DKT on improving postoperative intestinal dysfunction warrants further investigation.
Keyword
Figure
Reference
-
1. Asgeirsson T, El-Badawi KI, Mahmood A, Barletta J, Luchtefeld M, Senagore AJ. Postoperative ileus: it costs more than you expect. J Am Coll Surg. 2010; 210:228–231. PMID: 20113944.
Article2. Kehlet H. Surgery: Fast-track colonic surgery and the ‘knowing-doing’ gap. Nat Rev Gastroenterol Hepatol. 2011; 8:539–540. PMID: 21894195.3. Kono T, Shimada M, Yamamoto M, Kaneko A, Oomiya Y, Kubota K, et al. Complementary and synergistic therapeutic effects of compounds found in Kampo medicine: analysis of daikenchuto. Front Pharmacol. 2015; 6:159. PMID: 26300774.
Article4. Mochiki E, Yanai M, Ohno T, Kuwano H. The effect of traditional Japanese medicine (Kampo) on gastrointestinal function. Surg Today. 2010; 40:1105–1111. PMID: 21110152.
Article5. Kono T, Omiya Y, Hira Y, Kaneko A, Chiba S, Suzuki T, et al. Daikenchuto (TU-100) ameliorates colon microvascular dysfunction via endogenous adrenomedullin in Crohn's disease rat model. J Gastroenterol. 2011; 46:1187–1196. PMID: 21808981.
Article6. Takayama S, Seki T, Watanabe M, Takashima S, Sugita N, Konno S, et al. The effect of warming of the abdomen and of herbal medicine on superior mesenteric artery blood flow - a pilot study. Forsch Komplementmed. 2010; 17:195–201. PMID: 20829597.
Article7. Nishi M, Shimada M, Uchiyama H, Ikegami T, Arakawa Y, Hanaoka J, et al. The beneficial effects of Kampo medicine Dai-ken-chu-to after hepatic resection: a prospective randomized control study. Hepatogastroenterology. 2012; 59:2290–2294. PMID: 23435143.8. Yoshikawa K, Shimada M, Nishioka M, Kurita N, Iwata T, Morimoto S, et al. The effects of the Kampo medicine (Japanese herbal medicine) “Daikenchuto” on the surgical inflammatory response following laparoscopic colorectal resection. Surg Today. 2012; 42:646–651. PMID: 22202972.
Article9. Yaegashi M, Otsuka K, Itabashi T, Kimura T, Kato K, Fujii H, et al. Daikenchuto stimulates colonic motility after laparoscopic-assisted colectomy. Hepatogastroenterology. 2014; 61:85–89. PMID: 24895799.10. Akamaru Y, Takahashi T, Nishida T, Omori T, Nishikawa K, Mikata S, et al. Effects of daikenchuto, a Japanese herb, on intestinal motility after total gastrectomy: a prospective randomized trial. J Gastrointest Surg. 2015; 19:467–472. PMID: 25564322.
Article11. Katsuno H, Maeda K, Kaiho T, Kunieda K, Funahashi K, Sakamoto J, et al. Clinical efficacy of Daikenchuto for gastrointestinal dysfunction following colon surgery: a randomized, double-blind, multicenter, placebo-controlled study (JFMC39-0902). Jpn J Clin Oncol. 2015; 45:650–656. PMID: 25972515.
Article12. Shimada M, Morine Y, Nagano H, Hatano E, Kaiho T, Miyazaki M, et al. Effect of TU-100, a traditional Japanese medicine, administered after hepatic resection in patients with liver cancer: a multi-center, phase III trial (JFMC40-1001). Int J Clin Oncol. 2015; 20:95–104. PMID: 24595550.
Article13. Yoshikawa K, Shimada M, Wakabayashi G, Ishida K, Kaiho T, Kitagawa Y, et al. Effect of Daikenchuto, a traditional Japanese herbal medicine, after total gastrectomy for gastric cancer: a multicenter, randomized, double-blind, placebo-controlled, phase II trial. J Am Coll Surg. 2015; 221:571–578. PMID: 26141466.
Article14. Katsuno H, Maeda K, Ohya M, Yoshioka K, Tsunoda A, Koda K, et al. Clinical pharmacology of daikenchuto assessed by transit analysis using radiopaque markers in patients with colon cancer undergoing open surgery: a multicenter double-blind randomized placebo-controlled study (JFMC39-0902 additional study). J Gastroenterol. 2016; 51:222–229. PMID: 26162646.
Article15. Okada K, Kawai M, Hirono S, Fujii T, Kodera Y, Sho M, et al. Evaluation of the efficacy of daikenchuto (TJ -100) for the prevention of paralytic ileus after pancreaticoduodenectomy: A multicenter, double-blind, randomized, placebo-controlled trial. Surgery. 2016; 159:1333–1341. PMID: 26747224.
Article16. Higgins J, Green S, editors. Cochrane handbook for systematic reviews of interventions. version 5.1.0 [Internet]. Oxford (UK): The Cochrane Collaboration;2011. uptated 2011 Mar. cited 2017 Feb 10. Available from: http://handbook-5-1.cochrane.org/.17. Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009; 339:b2535. PMID: 19622551.
Article18. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011; 343:d5928. PMID: 22008217.
Article19. Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007; 8:16. PMID: 17555582.
Article20. Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med. 1998; 17:2815–2834. PMID: 9921604.
Article21. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 327:557–560. PMID: 12958120.
Article22. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994; 50:1088–1101. PMID: 7786990.
Article23. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997; 315:629–634. PMID: 9310563.
Article24. van Bree SH, Nemethova A, Cailotto C, Gomez-Pinilla PJ, Matteoli G, Boeckxstaens GE. New therapeutic strategies for postoperative ileus. Nat Rev Gastroenterol Hepatol. 2012; 9:675–683. PMID: 22801725.
Article25. Sheng QS, Pan Z, Chai J, Cheng XB, Liu FL, Wang JH, et al. Complete mesocolic excision in right hemicolectomy: comparison between hand-assisted laparoscopic and open approaches. Ann Surg Treat Res. 2017; 92:90–96. PMID: 28203556.
Article26. Satoh K, Kase Y, Yuzurihara M, Mizoguchi K, Kurauchi K, Ishige A. Effect of Daikenchu-to (Da-Jian-Zhong-Tang) on the delayed intestinal propulsion induced by chlorpromazine in mice. J Ethnopharmacol. 2003; 86:37–44. PMID: 12686439.
Article27. Endo M, Hori M, Ozaki H, Oikawa T, Hanawa T. Daikenchuto, a traditional Japanese herbal medicine, ameliorates postoperative ileus by anti-inflammatory action through nicotinic acetylcholine receptors. J Gastroenterol. 2014; 49:1026–1039. PMID: 23846546.
Article28. Hayakawa T, Kase Y, Saito K, Hashimoto K, Ishige A, Komatsu Y, et al. Effects of Dai-kenchu-to on intestinal obstruction following laparotomy. J Smooth Muscle Res. 1999; 35:47–54. PMID: 10463435.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prophylactic efficacy of probiotics on travelers' diarrhea: an adaptive meta-analysis of randomized controlled trials
- The Efficacy of Hypnotherapy in the Treatment of Irritable Bowel Syndrome: A Systematic Review and Meta-analysis
- Antioxidant Supplementation for Erectile Dysfunction: Systematic Review and Meta-Analysis of Double-Blind, Randomized, Placebo-Controlled Trials
- Efficacy of Vitamin C Supplements in Prevention of Cancer: A Meta-Analysis of Randomized Controlled Trials
- Effects of Anti-Obesity Strategies on Bone Mineral Density: A Comprehensive Meta-Analysis of Randomized Controlled Trials