Imaging Sci Dent.
2018 Jun;48(2):139-145. 10.5624/isd.2018.48.2.139.
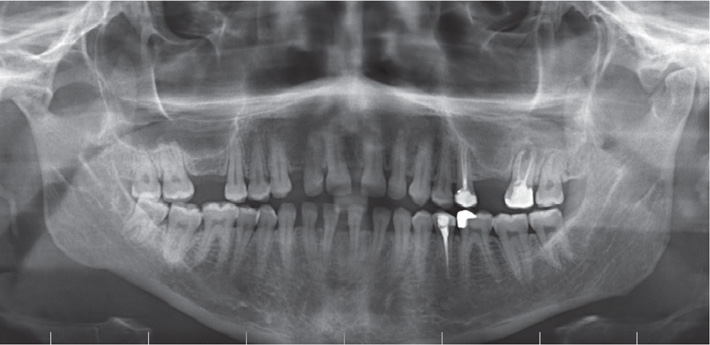
Maxillary sinus aspergilloma of odontogenic origin: Report of 2 cases with cone-beam computed tomographic findings and review of the literature
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Ondokuz Mayis University, Samsun, Turkey. ezgiyuceer@hotmail.com
- 2Department of Pathology, Faculty of Medicine, Ondokuz Mayis University, Samsun, Turkey.
- KMID: 2413926
- DOI: http://doi.org/10.5624/isd.2018.48.2.139
Abstract
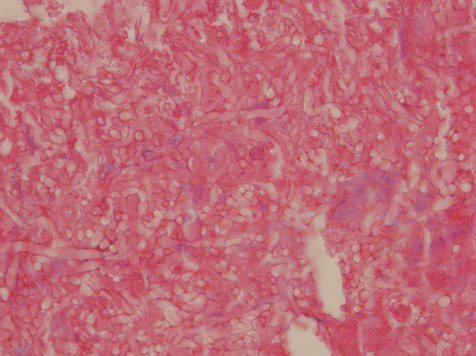
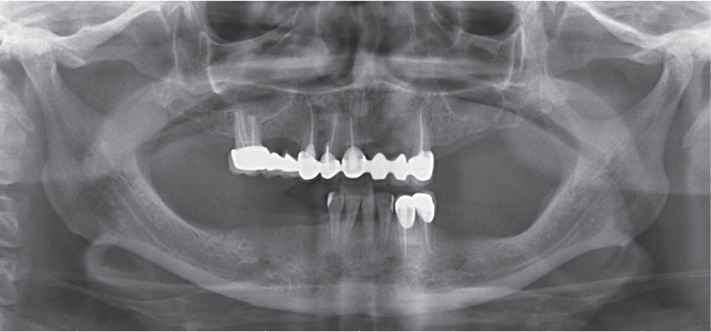
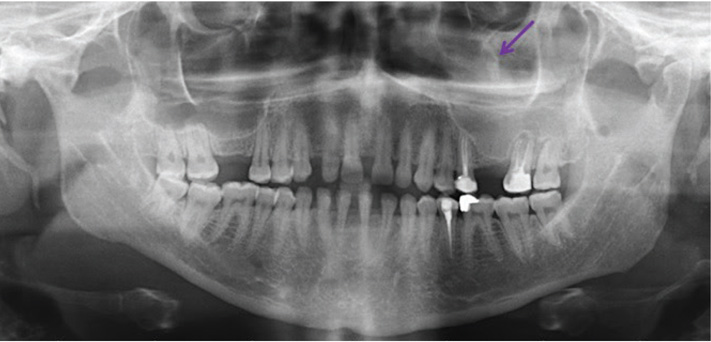
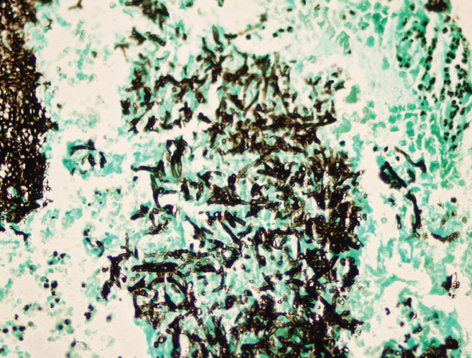
- Aspergilloma of the maxillary sinus is considered rare in immunocompetent patients, but a considerable increase has recently been seen in the incidence of reported cases. Dental procedures involving the antral region are thought to predispose individuals to this form of aspergillosis. Because aspergilloma shares similar clinical features with other sinus pathologies, its diagnosis may be delayed. Thus, an early diagnosis confirmed by a histopathological examination plays a crucial role in the adequate management of aspergilloma. This article provides a concise review of the reported cases of aspergilloma associated with dental procedures and reports 2 new cases of aspergilloma in middle-aged female patients, with a presentation of their cone-beam computed tomographic findings.
MeSH Terms
Figure
Reference
-
1. Falworth MS, Herold J. Aspergillosis of the paranasal sinuses. A case report and radiographic review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996; 81:255–260.2. Martinez D, Burgueno M, Forteza G, Martin M, Sierra I. Invasive maxillary aspergillosis after dental extraction. Case report and review of the literature. Oral Surg Oral Med Oral Pathol. 1992; 74:466–468.3. Urs AB, Singh H, Nunia K, Mohanty S, Gupta S. Post endodontic Aspergillosis in an immunocompetent individual. J Clin Exp Dent. 2015; 7:e535–e539.
Article4. Khongkhunthian P, Reichart PA. Aspergillosis of the maxillary sinus as a complication of overfilling root canal material into the sinus: report of two cases. J Endod. 2001; 27:476–478.
Article5. Harada T, Isomura ET, Uchihashi T, Kogo M. Aspergillosis associated with migration of a dental implant into the maxillary sinus: a case report. J Oral Maxillofac Surg Med Pathol. 2017; 29:448–451.
Article6. Sato FR, Sawazaki R, Berretta D, Moreira RW, Vargas PA, de Almeida OP. Aspergillosis of the maxillary sinus associated with a zygomatic implant. J Am Dent Assoc. 2010; 141:1231–1235.
Article7. Sohn DS, Lee JK, Shin HI, Choi BJ, An KM. Fungal infection as a complication of sinus bone grafting and implants: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 107:375–380.
Article8. Burnham R, Bridle C. Aspergillosis of the maxillary sinus secondary to a foreign body (amalgam) in the maxillary antrum. Br J Oral Maxillofac Surg. 2009; 47:313–315.
Article9. Tomazic PV, Dostal E, Magyar M, Lang-Loidolt D, Wolf A, Koele W, et al. Potential correlations of dentogenic factors to the development of clinically verified fungus balls: a retrospective computed tomography-based analysis. Laryngoscope. 2016; 126:39–43.
Article10. De Foer C, Fossion E, Vaillant JM. Sinus aspergillosis. J Craniomaxillofac Surg. 1990; 18:33–40.
Article11. Matjaz R, Jernej P, Mirela KR. Sinus maxillaris mycetoma of odontogenic origin: case report. Braz Dent J. 2004; 15:248–250.12. Guivarc'h M, Ordioni U, Catherine JH, Campana F, Camps J, Bukiet F. Implications of endodontic-related sinus aspergillosis in a patient treated by infliximab: a case report. J Endod. 2015; 41:125–129.13. Legent F, Billet J, Beauvillain C, Bonnet J, Miegeville M. The role of dental canal fillings in the development of Aspergillus sinusitis. A report of 85 cases. Arch Otorhinolaryngol. 1989; 246:318–320.14. Fanucci E, Nezzo M, Neroni L, Montesani L Jr, Ottria L, Gargari M. Diagnosis and treatment of paranasal sinus fungus ball of odontogenic origin: case report. Oral Implantol (Rome). 2014; 6:63–66.
Article15. Giardino L, Pontieri F, Savoldi E, Tallarigo F. Aspergillus mycetoma of the maxillary sinus secondary to overfilling of a root canal. J Endod. 2006; 32:692–694.16. Vinciguerra A, Saibene AM, Lozza P, Maccari A. Unusual case of bilateral maxillary fungus ball. BMJ Case Rep. 2016; 2016:bcr2016217930.
Article17. Ogata Y, Okinaka Y, Takahashi M. Antrolith associated with aspergillosis of the maxillary sinus: report of a case. J Oral Maxillofac Surg. 1997; 55:1339–1341.
Article18. Axelsson H, Carlsöö B, Weibring J, Winblad B. Aspergillosis of the maxillary sinus: clinical and histopathological features of 4 cases and a review of the literature. Acta Otolaryngol. 1978; 86:303–308.
Article19. Kawana T, Yamamoto H, Izumi H. A case of aspergillosis of the maxillary sinus. J Nihon Univ Sch Dent. 1987; 29:298–302.
Article20. Kobayashi A. Asymptomatic aspergillosis of the maxillary sinus associated with foreign body of endodontic origin. Report of a case. Int J Oral Maxillofac Surg. 1995; 24:243–244.21. Horré R, Schumacher G, Marklein G, Krömer B, Wardelmann E, Gilges S, et al. Case report. Maxillary sinus infection due to Emericella nidulans. Mycoses. 2002; 45:402–405.22. Martins WD, Ribeiro Rosa EA. Aspergillosis of the maxillary sinus: review and case report. Scand J Infect Dis. 2004; 36:758–761.
Article23. Bosi GR, de Braga GL, de Almeida TS, de Carli A. Fungus ball of the paranasal sinuses: report of two cases and literature review. Int Arch Otorhinolaryngol. 2012; 16:286–290.
Article24. Cansiz E, Akbas E, Isler SC. Aspergillosis associated with surgically assisted rapid maxillary expansion. Natl J Maxillofac Surg. 2016; 7:105–107.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cone-beam computed tomographic imaging of silent sinus syndrome: A case series and a literature review
- Aspergilloma of the maxillary sinus: report of a case
- Maxillary sinus pneumatization after maxillary molar extraction assessed with cone beam computed tomography
- Comparison of panoramic radiography and cone beam computed tomography for assessing the relationship between the maxillary sinus floor and maxillary molars
- Incidental finding of metastatic malignancy involving the sphenoid sinus on a cone-beam computed tomographic scan: A case report