Transl Clin Pharmacol.
2018 Jun;26(2):93-98. 10.12793/tcp.2018.26.2.93.
Population pharmacodynamics of cilostazol in healthy Korean subjects
- Affiliations
-
- 1Department of Pharmacology, Yonsei University College of Medicine, Seoul 03722, Korea. kspark@yuhs.ac
- 2Brain Korea 21 Plus Project for Medical Science, Yonsei University, Seoul 03722, Korea.
- KMID: 2413833
- DOI: http://doi.org/10.12793/tcp.2018.26.2.93
Abstract
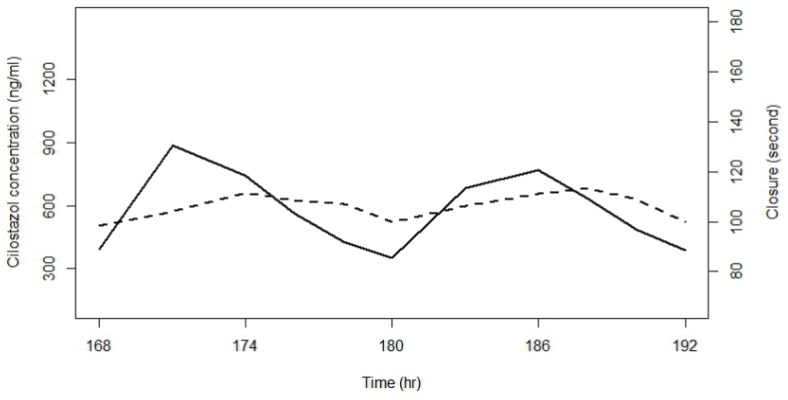
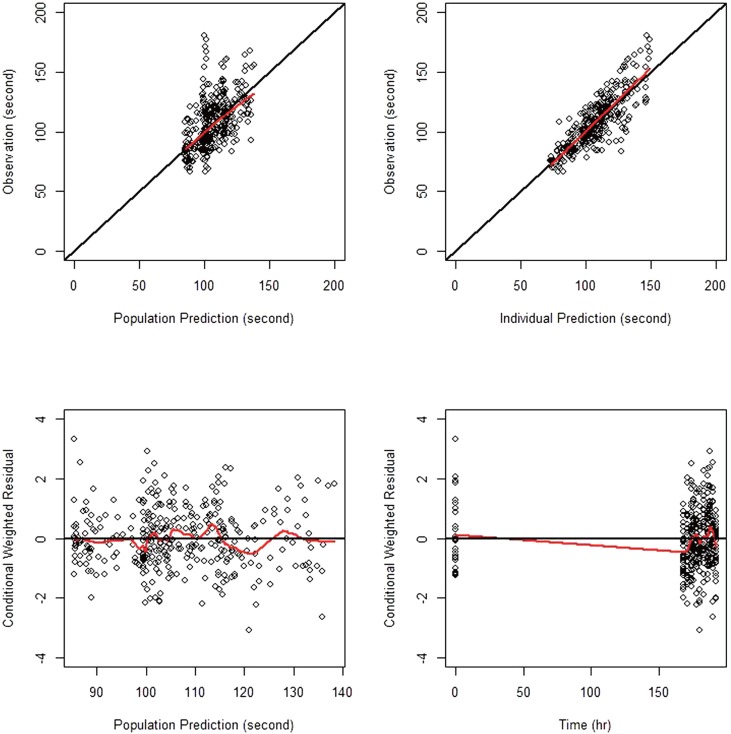
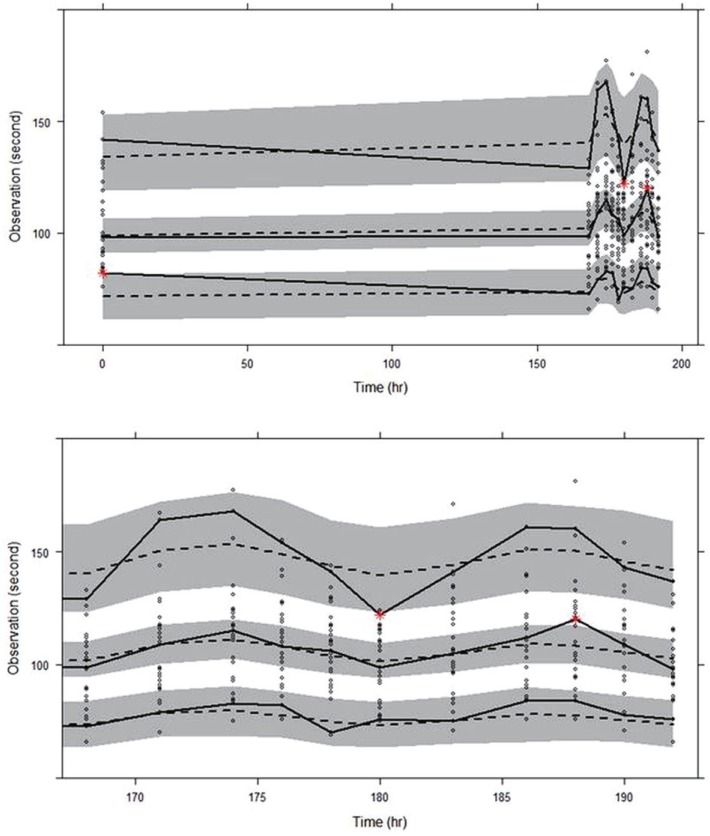
- Cilostazol is used for the treatment of intermittent claudication, ulceration and pain. This study was conducted to develop a population pharmacodynamic (PD) model for cilostazol's closure time (CT) prolongation effect in healthy Korean subjects based on a pharmacokinetic (PK) model previously developed. PD data were obtained from 29 healthy subjects who participated in a study conducted in 2009 at Severance Hospital. The PK model used was a two-compartment model with first order absorption. CT data were best described by a turnover model with a fractional turnover rate constant (K(out)) inhibited by drug effects (Eff), which were represented by a sigmoid E(max) model [Eff = E(max) · C(γ) / (ECâ‚…â‚€(γ)+C(γ))] with E(max) being maximum drug effect, ECâ‚…â‚€ drug plasma concentration at 50% of E(max), C drug plasma concentrations, and γ the Hill coefficient. For the selected PD model, parameter estimates were 0.613 hr⻹ for K(out), 0.192 for E(max), 730 ng/ml for ECâ‚…â‚€ and 5.137 for γ. Sex and caffeine drinking status significantly influenced the baseline CT, which was 85.36 seconds in male non-caffeine drinkers and increased by 15.5% and 16.4% in females and caffeine drinkers, respectively. The model adequately described the time course of CT. This was the first population PD study for cilostazol's CT prolongation effect in a Korean population.
Keyword
MeSH Terms
Figure
Reference
-
1. Horie N, Kaminogo M, lzumo T, Hayashi K, Tsujino A, Nagata I. Cilostazol may prevent cardioembolic stroke in patients undergoing antiplatelet therapy. Neurol Res. 2015; 37:619–623. DOI: 10.1179/1743132815Y.0000000021. PMID: 25798683.
Article2. Falconer TM, Eikelboom JW, Hankey GJ, Norman PE. Management of peripheral arterial disease in the elderly: focus on cilostazol. Clin Interv Aging. 2008; 3:17–23. PMID: 18488875.3. Chi YW, lavie CJ, Milani RV, White CJ. Safety and efficacy of cilostazol in the management of intermittent claudication. Vasc health Risk Manag. 2008; 4:1197–1203. PMID: 19337533.
Article4. O'Donnell ME, Badger SA, Sharif MA, Young IS, Lee B, Soong CV. The vascular and biochemical effects of cilostazol in patients with peripheral arterial disease. J Vasc Surg. 2009; 49:1226–1234. DOI: 10.1016/j.jvs.2008.11.098. PMID: 19217745.5. Ikeda U, Ikeda M, Kano S, Kanbe T, Shimada K. Effect of cilostazol, a cAMP phosphodiesterase inhibitor, on nitric oxide production by vascular smooth muscle cells. Eur J Pharmacol. 1996; 314:197–202. PMID: 8957237.
Article6. Yoo HD, Cho HY, Lee YB. Population pharmacokinetic analysis of cilostazol in healthy subjects with genetic polymorphisms of CYP3A5, CYP2C19 and ABCB1. Br J Clin Pharmacol. 2010; 69:27–37. DOI: 10.1111/j.1365-2125.2009.03558.x. PMID: 20078610.7. Shao JS, Zhong FL, Hua TC, Fan DZ. Cardiovascular effects and simultaneous pharmacokinetic and pharmacodynamic modeling of cilostazol in healthy subjects. Asian J Drug Metab Pharmacokinet. 2005; 5:301–308.8. Lee D, Son H, Lim LA, Park K. Population pharmacokinetic analysis of diurnal and seasonal variations of plasma concentrations of cilostazol in healthy volunteers. Ther Drug Monit. 2014; 36:771–780. DOI: 10.1097/FTD.0000000000000077. PMID: 24739664.
Article9. Suri A, Forbes WP, Bramer SL. Pharmacokinetics of multiple-dose oral cilostazol in middle-age and elderly men and women. J Clin Pharmacol. 1998; 38:144–150. PMID: 9549645.
Article10. Lee D, Lim LA, Jang SB, Lee YJ, Chung JY, Choi JR, et al. Pharmacokinetic comparison of sustained- and immediate-release oral formulations of cilostazol in healthy Korean subjects: a randomized, open-label, 3-part, sequential, 2-period, crossover, single-dose, food-effect, and multiple-dose study. Clin Ther. 2011; 33:2038–2053. DOI: 10.1016/j.clinthera.2011.10.024. PMID: 22129569.
Article11. Woo SK, Kang WK, Kwon KI. Pharmacokinetic and pharmacodynamic modeling of the antiplatelet and cardiovascular effects of cilostazol in healthy humans. Clin Pharmacol Ther. 2002; 71:246–252. PMID: 11956507.
Article12. Yun HY, Kang W, Lee BY, Park S, Yoon YR, Yeul Ma J, et al. Semi-mechanistic modeling and simulation of inhibition of platelet aggregation by antiplatelet agents. Basic Clin Pharmacol Toxicol. 2014; 115:352–359. DOI: 10.1111/bcpt.12222. PMID: 24612881.13. Paniccia R, Priora R, Liotta AA, Abbate R. Platelet function tests: a comparative review. Vasc Health Risk Manag. 2015; 11:133–148. DOI: 10.2147/VHRM.S44469. PMID: 25733843.
Article14. Karger R, Donner-Banzhoff N, Müller HH, Kretschmer V, Hunink M. Diagnostic performance of the platelet function analyzer (PFA-100) for the detection of disorders of primary haemostasis in patients with a bleeding history–a systematic review and meta-analysis. Platelets. 2007; 18:249–260. PMID: 17538845.
Article15. Felmlee MA, Morris ME, Mager DE. Mechanism-based pharmacodynamic modeling. Methods Mol Biol. 2012; 929:583–600. PMID: 23007443.
Article16. Mould DR, Upton RN. Basic Concepts in Population Modeling, Simulation, and Model-Based Drug Development: part 3-Introduction to Pharmacodynamic Modeling Methods. CPT Pharmacometrics Syst Pharmacol. 2014; 3:e88. DOI: 10.1038/psp.2013.71. PMID: 24384783.17. Cho YU, Chi HS, Jang S, Park CJ. Reconfirmation of preanalytical variables and establishment of reference intervals of platelet function analyzer-100 closure times in Korean adults. Korean J Lab Med. 2007; 27:318–323. PMID: 18094595.
Article18. Kim YS, Lee IO, Park HY, Park JH, Lim BG, Kim H. Platelet function assay to determine the optimal preoperative cessation period of aspirin. Anesth Pain Med. 2014; 9:31–35.19. Varani K, Portaluppi F, Gessi S, Merighi S, Ongini E, Belardinelli L, et al. Dose and Time Effects of Caffeine Intake on Human Platelet Adenosine A_2A Receptors. Circulation. 2000; 102:285–289. PMID: 10899090.20. Natella F, Nardini M, Belelli F, Pignatelli P, Di Santo S, Ghiselli A, et al. Effect of coffee drinking on platelets: inhibition of aggregation and phenols incorporation. Br J Nutr. 2008; 100:1276–1282. DOI: 10.1017/S0007114508981459. PMID: 18439332.
Article21. Becker DM, Segal J, Vaidya D, Yanek LR, Herrera-Galeano JE, Bray PF, et al. Sex differences in platelet reactivity and response to low-dose aspirin therapy. JAMA. 2006; 295:1420–1427. PMID: 16551714.
Article22. Miller CH, Rice AS, Garrett K, Stein SF. Gender, race and diet affect platelet function tests in normal subjects, contributing to a high rate of abnormal results. Br J Haematol. 2014; 165:842–853. DOI: 10.1111/bjh.12827. PMID: 24617520.
Article23. Hobson AR, Qureshi Z, Banks P, Curzen N. Gender and responses to aspirin and clopidogrel: insights using short thrombelastography. Cardiovasc Ther. 2009; 27:246–252. DOI: 10.1111/j.1755-5922.2009.00106.x. PMID: 19903188.
Article24. Chae D, Son M, Kim Y, Son H, Park K. Mechanistic model for blood pressure and heart rate changes produced by telmisartan in human beings. Basic Clin Pharmacol Toxicol. 2018; 122:139–148. DOI: 10.1111/bcpt.12856. PMID: 28805311.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pharmacokinetics and pharmacodynamics of drugs for sedation
- Monitoring the Antiplatelet Effect of Cilostazol with Light Transmission Aggregometer: Two Cases of Possible Cilostazol Resistance
- Influence of Oxygen to Population Pharmacokinetics/Pharmacodynamics of Alcohol in Healthy Volunteers
- Pharmacokinetic characteristics of cilostazol 200 mg controlled-release tablet compared with two cilostazol 100 mg immediate-release tablets (Pletal) after single oral dose in healthy Korean male volunteers
- Association Between Carotid Artery Stiffness and Headache Following Cilostazol Use in Cerebral Infarction Patients