J Korean Ophthalmol Soc.
2018 Jun;59(6):582-588. 10.3341/jkos.2018.59.6.582.
Clinical Efficacy of Lacrimal Endoscopy Assisted Silicone Tube Intubation in Patients with Nasolacrimal Duct Obstruction
- Affiliations
-
- 1Department of Ophthalmology, CHA Bundang Medical Center, CHA University, Seongnam, Korea. eye@cha.ac.kr
- KMID: 2413823
- DOI: http://doi.org/10.3341/jkos.2018.59.6.582
Abstract
- PURPOSE
We evaluated the clinical efficacy of lacrimal endoscopy-assisted silicone tube intubation in patients with a nasolacrimal duct obstruction.
METHODS
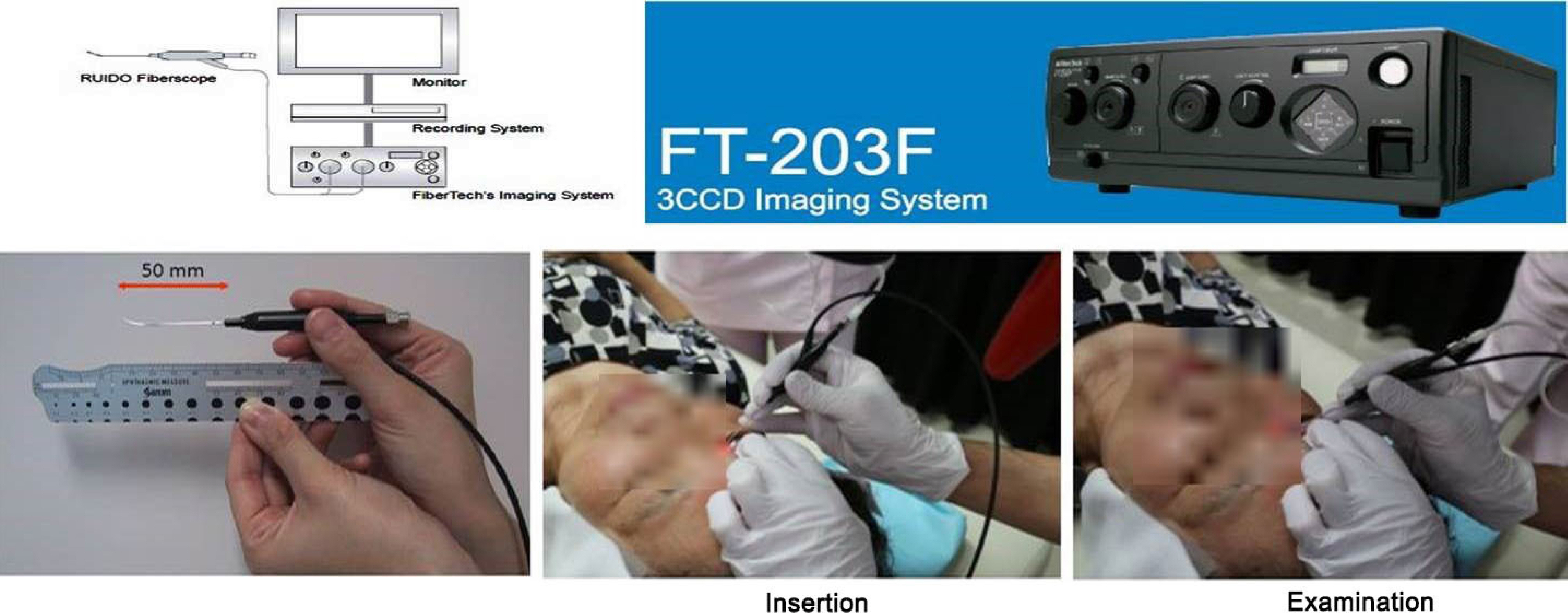
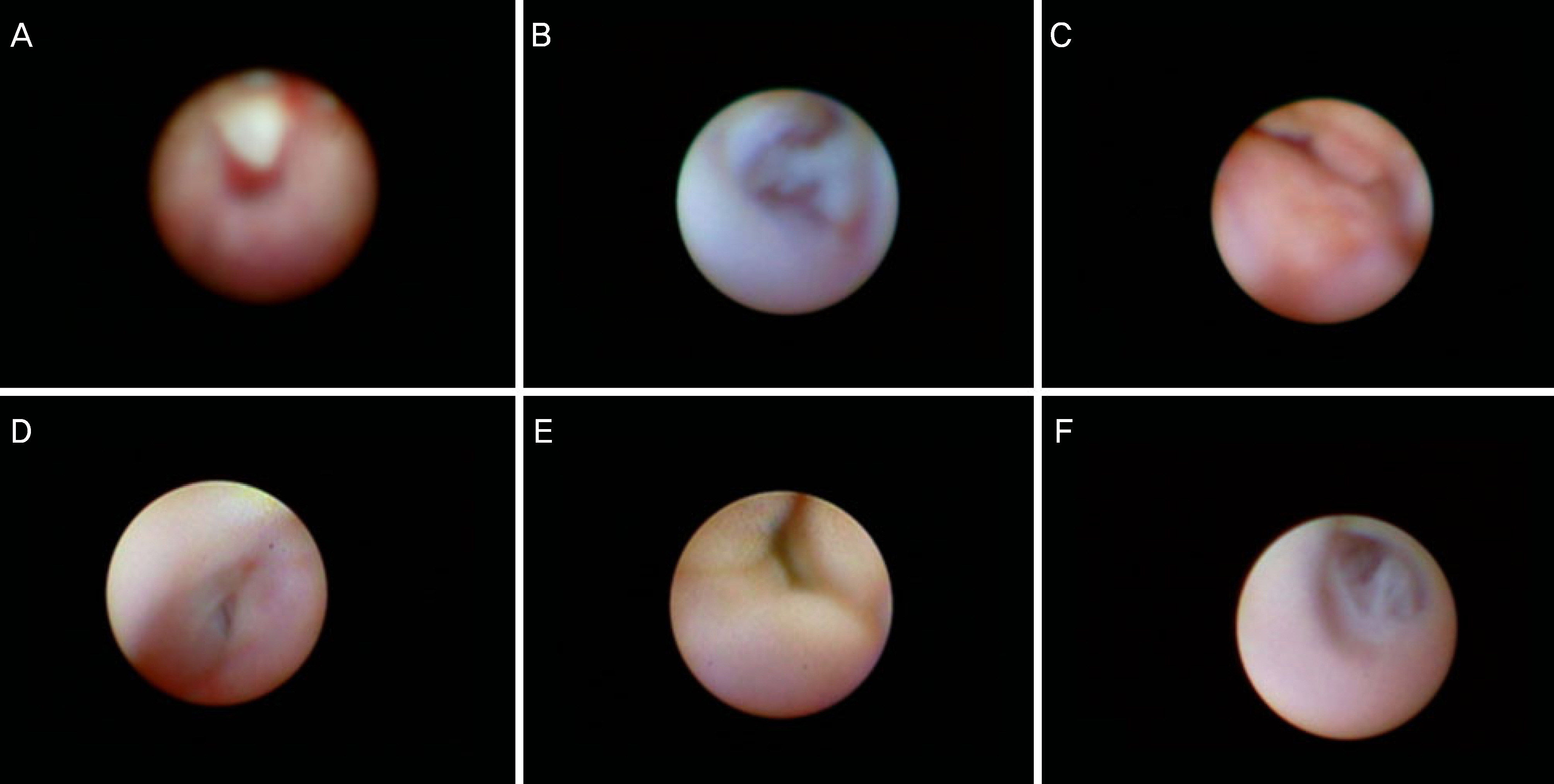
We conducted a retrospective chart review of 86 eyes of 67 patients who underwent lacrimal endoscopy (RUIDO fiberscope; Fibertechco, Tokyo, Japan)-assisted silicone tube intubation from December 2014 to March 2017. We compared clinical characteristics, irrigation test results, and dacryocystographic and lacrimal endoscopic findings, and analyzed factors related to surgical success.
RESULTS
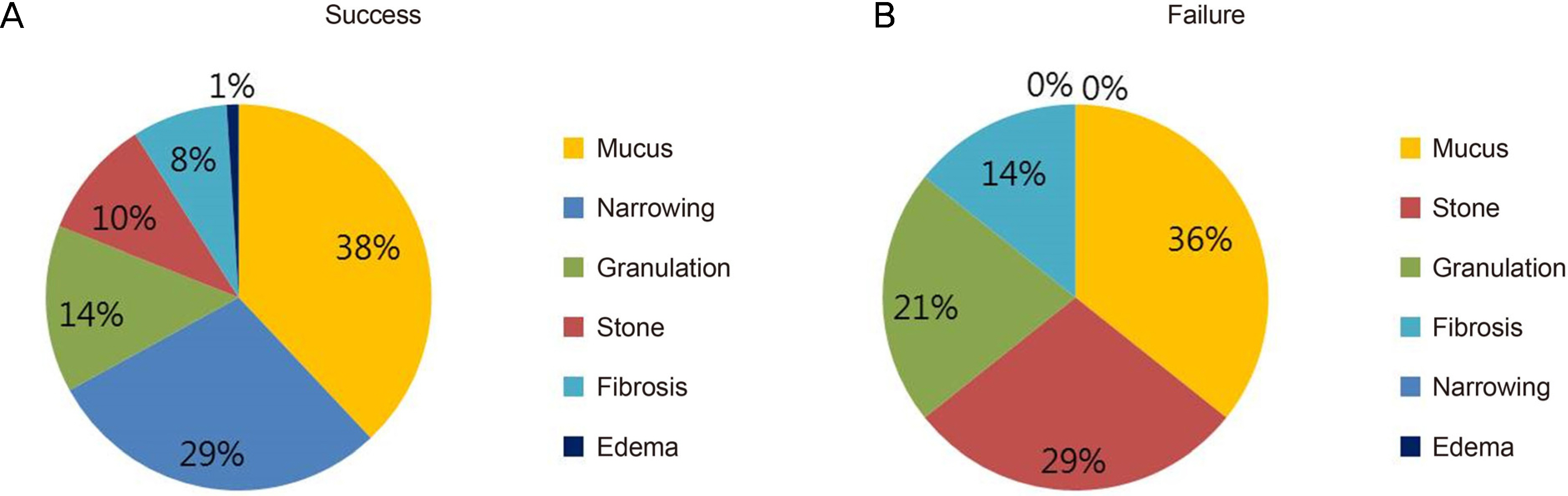
In total, 86 eyes of 67 patients underwent lacrimal endoscopy-assisted silicone tube intubation. The success rate was 87.2%. There was a significantly lower preoperative tear meniscus height (420.5 ± 198.1 µm vs. 639.0 ± 224.3 µm, p < 0.001). In the surgically successful group, narrowing was frequently observed (29.0% vs. 0%, p = 0.030). Dacryolith findings were associated with surgical failure (10% vs. 29%, p = 0.043).
CONCLUSIONS
Lacrimal endoscopy-assisted silicone tube intubation is considered an effective and successful operative procedure and enables the observation of real-time findings inside the lacrimal drainage passage for the treatment of pathological lesions. Narrowing observed during lacrimal endoscopy indicated successful treatment as opposed to dacryolith findings, which were associated with a failed outcome.
MeSH Terms
Figure
Cited by 1 articles
-
Comparison of Success Rates after Silicone Tube Intubation with or without Lacrimal Endoscopy for Epiphora
Min Gyu Choi, Jeong Kyu Lee
J Korean Ophthalmol Soc. 2018;59(11):1001-1008. doi: 10.3341/jkos.2018.59.11.1001.
Reference
-
References
1. Gibbs D. New probe for the intubation of lacrimal canaliculi with silicone rubber tubing. Br J Ophthalmol. 1967; 51:198.
Article2. Kwon YH, Lee YJ. abdominal results of silicone tube intubation in incomplete nasolacrimal duct obstruction (NLDO). J Korean Ophthalmol Soc. 2008; 49:190–4.3. Salari AM, Tokhmehchi MR. A simplified method for abdominal silicon intubation. Acta ophthalmol. 2008; 86:230.4. Cohen S, Prescott R, Sherman M, et al. Dacryoscopy. Ophthalmic Surg. 1979; 10:57–63.5. Sasaki T, Nagata Y, Sugiyama K. Nasolacrimal duct obstruction classified by dacryoendoscopy and treated with inferior meatal dacryorhinotomy. Part I: Positional diagnosis of primary nasolacrimal duct obstruction with dacryoendoscope. Am J Ophthalmol. 2005; 140:1065–9.
Article6. Fujimoto M, Ogino K, Matsuyama H, Miyazaki C. Success rates of dacryoendoscopy-guided probing for recalcitrant congenital abdominal duct obstruction. Jpn J Ophthalmol. 2016; 60:274–9.7. Lim SW, Sung YJ, Lew H. Clinical efficacy of lacrimal endoscopy in patients with epiphora. J Korean Ophthalmol Soc. 2017; 58:495–502.
Article8. Soll DB. Silicone intubation: an alternative to dacryocystorhinostomy. Ophthalmology. 1978; 85:1259–66.
Article9. Pashby RC, Rathbun JE. Silicone tube intubation of the lacrimal drainage system. Arch Ophthalmol. 1979; 97:1318–22.
Article10. Anderson RL, Edwards JJ. Indications, complications and results with silicone stents. Ophthalmology. 1979; 86:1474–87.
Article11. Lee SH, Kim SD, Kim JD. Silicone intubation for nasolacrimal duct obstruction in adult. J Korean Ophthalmol Soc. 1997; 38:185–9.12. Sohn HY, Hur J, Chung EH, Won IG. Clinical observation on abdominal intubation in obstruction of lacrimal drainage system. J Korean Ophthalmol Soc. 1990; 31:135–40.13. Yazici B, Akarsu C, Salkaya M. Silicone intubation with the Ritleng method in children with congenital nasolacrimal duct obstruction. J AAPOS. 2006; 10:328–32.14. Han JS, Park IK, Shin JH. Success rate of silicone intubation abdominal nasolacrimal duct obstruction and stenosis according to dacryocystography. J Korean Ophthalmol Soc. 2013; 54:845–9.15. Kim YR, Ahn M. Long term effect of double silicone tube abdominal for acquired nasolacrimal duct obstruction. J Korean Ophthalmol Soc. 2012; 53:1554–8.16. Baek JS, Lee S, Lee JH, et al. Predictors of silicone tube intubation success in patients with lacrimal drainage system stenosis. Korean J Ophthalmol. 2016; 30:157–62.
Article17. Haefliger IO, Piffaretti JM. Lacrimal drainage system endoscopic examination and surgery through the lacrimal punctum. Klin Monbl Augenheilkd. 2001; 218:384–7.
Article18. Sasaki H, Takano T, Murakami A. Direct endoscopic probing for congenital lacrimal duct obstruction. Clin Exp Ophthalmol. 2013; 41:729–34.
Article19. Yazici B, Hammad AM, Meyer DR. Lacrimal sac dacryoliths: abdominal factors and clinical characteristics. Ophthalmology. 2001; 108:1308–12.20. Komínek P, Č ervenka S, Zeleník K, et al. Lacrimal sac dacryolith (76 cases): a predictive factor for successful endonasal abdominal? Eur Arch Otorhinolaryngol. 2014; 271:1595–9.21. Choi SW, Park JS, Kwon AY, Lew H. Clinicopathological study of lacrimal sac dacryolith in patients treated for nasolacrimal duct obstruction. J Korean Ophthalmol Soc. 2016; 57:6–13.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Analysis of the Success Rate of Silicone Tube Intubation According to Lacrimal Endoscopy Findings
- Effect of Lacrimal Endoscopy on Operation Time in Silicone Tube Intubation for Nasolacrimal Duct Obstruction
- Treatment of Congenital Nasolacrimal Duct Obstruction Using Silicone Intubation Set
- Result of Partial Nasolacrimal Duct Obstruction After Silicone Tube Intubation
- Silicone Intubation in Children with Nasolacrimal Duct Obstruction