Korean J Radiol.
2018 Aug;19(4):733-741. 10.3348/kjr.2018.19.4.733.
Yield of Repeat Targeted Direct in-Bore Magnetic Resonance-Guided Prostate Biopsy (MRGB) of the Same Lesions in Men Having a Prior Negative Targeted MRGB
- Affiliations
-
- 1Department of Radiology and Nuclear Medicine, Radboud University Medical Center, Nijmegen 6500, the Netherlands. Wulphert.Venderink@radboudumc.nl
- 2Department of Urology, Radboud University Medical Center, Nijmegen 6500, the Netherlands.
- 3Department of Radiology, Kawasaki Medical School, Kurashiki city, Okayama 701-0192, Japan.
- KMID: 2413702
- DOI: http://doi.org/10.3348/kjr.2018.19.4.733
Abstract
OBJECTIVE
This study's purposes were to determine the yield of repeat direct in-bore magnetic resonance-guided prostate biopsy (MRGB) (MRGB-2) after the first one was found to be negative (MRGB-1), to correlate with clinical parameters, and to present the subgroup analyses of patients with positive repeat biopsies, despite having a negative initial biopsies.
MATERIALS AND METHODS
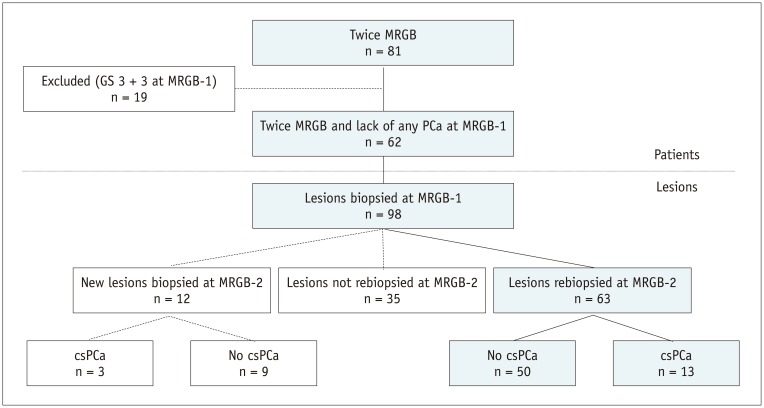
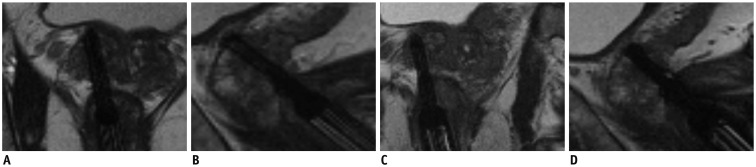
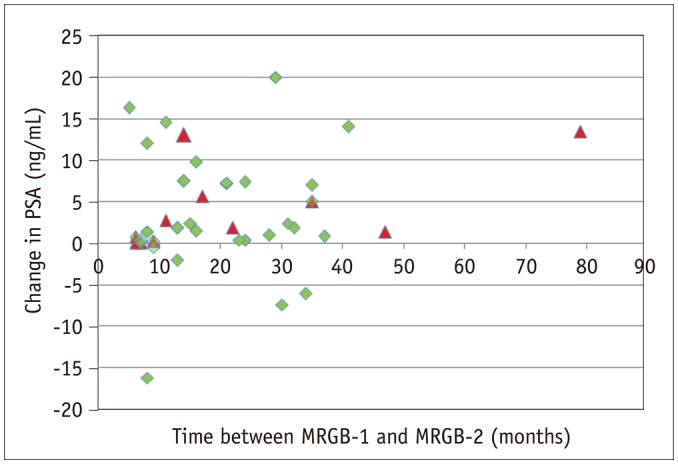
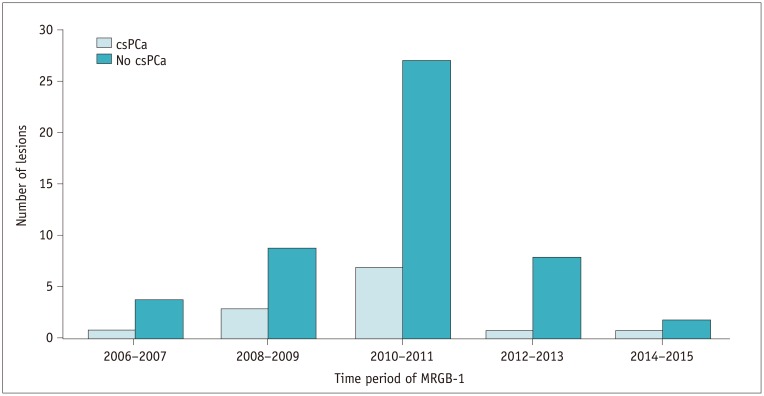
We retrospectively included patients with MRGB-2 after a negative MRGB-1 both between January 2006 and August 2016. This study included 62 patients (median age, 63 years; interquartile range [IQR], 58-66 years) with 75 sampled lesions during MRGB-2 left for analysis, and 63 lesions were resampled and 12 new lesions were sampled. Included patients had a prostate specific antigen (PSA) at MRGB-1 of 13 ng/mL (IQR, 5.8-20.0) and a PSA at MRGB-2 of 15 ng/mL (IQR, 9.0-22.5). All anonymized magnetic resonance imaging (MRI) data were retrospectively reassessed according to Prostate Imaging-Reporting and Data System version 2 by two radiologists. Images of MRGB were compared to determine whether the same prostate lesion was biopsied during MRGB-1 and MRGB-2. Descriptive statistics were utilized to determine the yield of clinically significant prostate cancer (csPCa) at MRGB-2. Gleason score of ≥ 3 + 4 was considered csPCa.
RESULTS
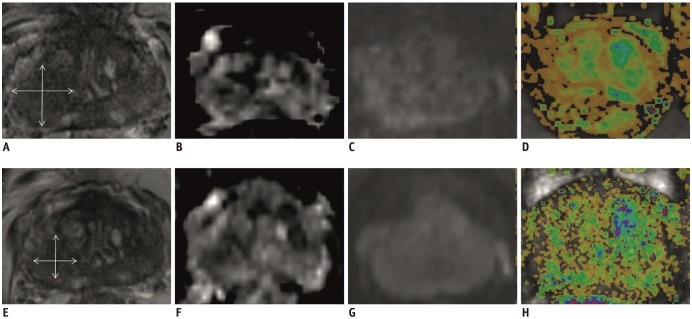
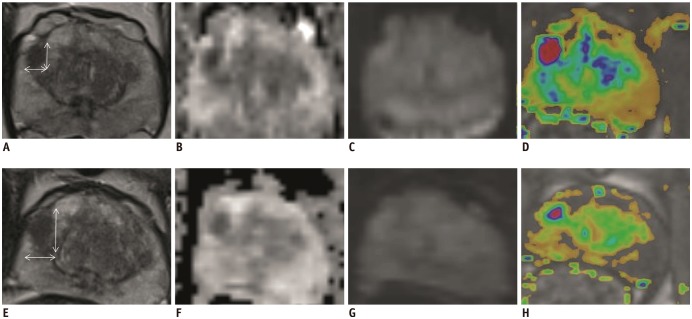
In 16/75 (21%) lesions csPCa was detected during MRGB-2. Of 63 resampled lesions, 13 (21%) harbored csPCa at MRGB-2. In two patients, csPCa was detected on repeat biopsy, while the volume of the lesion decreased between MRGB-1 and MRGB-2.
CONCLUSION
Patients could benefit from repeat biopsy after negative initial MRGB, especially in the case of increasing PSA values and persisting PCa suspicion in MRI. Further research is needed to establish predictors for positive repeat targeted biopsies.
Keyword
MeSH Terms
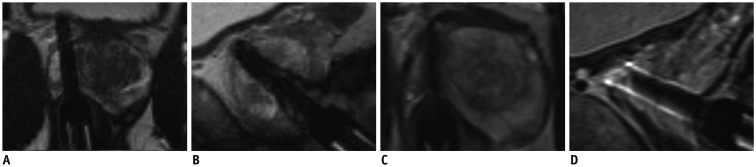
Figure
Reference
-
1. Siddiqui MM, Rais-Bahrami S, Turkbey B, George AK, Rothwax J, Shakir N, et al. Comparison of MR/ultrasound fusion-guided biopsy with ultrasound-guided biopsy for the diagnosis of prostate cancer. JAMA. 2015; 313:390–397. PMID: 25626035.
Article2. Hambrock T, Somford DM, Hoeks C, Bouwense SA, Huisman H, Yakar D, et al. Magnetic resonance imaging guided prostate biopsy in men with repeat negative biopsies and increased prostate specific antigen. J Urol. 2010; 183:520–527. PMID: 20006859.
Article3. Fütterer JJ. Multiparametric MRI in the detection of clinically significant prostate cancer. Korean J Radiol. 2017; 18:597–606. PMID: 28670154.
Article4. Meng X, Rosenkrantz AB, Mendhiratta N, Fenstermaker M, Huang R, Wysock JS, et al. Relationship between prebiopsy multiparametric magnetic resonance imaging (MRI), biopsy indication, and MRI-ultrasound fusion-targeted prostate biopsy outcomes. Eur Urol. 2016; 69:512–517. PMID: 26112001.
Article5. Baco E, Rud E, Eri LM, Moen G, Vlatkovic L, Svindland A, et al. A randomized controlled trial to assess and compare the outcomes of two-core prostate biopsy guided by fused magnetic resonance and transrectal ultrasound images and traditional 12-core systematic biopsy. Eur Urol. 2016; 69:149–156. PMID: 25862143.
Article6. Venderink W, van Luijtelaar A, Bomers JG, van der Leest M, Hulsbergen-van de Kaa C, Barentsz JO, et al. Results of targeted biopsy in men with magnetic resonance imaging lesions classified equivocal, likely or highly likely to be clinically significant prostate cancer. Eur Urol. 2017; 2. 28. [Epub]. DOI: 10.1016/j.eururo.2017.02.021.
Article7. Wegelin O, van Melick HHE, Hooft L, Bosch JLHR, Reitsma HB, Barentsz JO, et al. Comparing three different techniques for magnetic resonance imaging-targeted prostate biopsies: a systematic review of in-bore versus magnetic resonance imaging-transrectal ultrasound fusion versus cognitive registration. Is there a preferred technique? Eur Urol. 2017; 71:517–531. PMID: 27568655.
Article8. Arsov C, Rabenalt R, Blondin D, Quentin M, Hiester A, Godehardt E, et al. Prospective randomized trial comparing magnetic resonance imaging (MRI)-guided in-bore biopsy to MRI-ultrasound fusion and transrectal ultrasound-guided prostate biopsy in patients with prior negative biopsies. Eur Urol. 2015; 68:713–720. PMID: 26116294.
Article9. Ahmed HU, El-Shater Bosaily A, Brown LC, Gabe R, Kaplan R, Parmar MK, et al. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet. 2017; 389:815–822. PMID: 28110982.
Article10. Delongchamps NB, Peyromaure M, Schull A, Beuvon F, Bouazza N, Flam T, et al. Prebiopsy magnetic resonance imaging and prostate cancer detection: comparison of random and targeted biopsies. J Urol. 2013; 189:493–499. PMID: 22982424.
Article11. Sonn GA, Natarajan S, Margolis DJ, MacAiran M, Lieu P, Huang J, et al. Targeted biopsy in the detection of prostate cancer using an office based magnetic resonance ultrasound fusion device. J Urol. 2013; 189:86–91. PMID: 23158413.
Article12. Chelluri R, Kilchevsky A, George AK, Sidana A, Frye TP, Su D, et al. Prostate cancer diagnosis on repeat magnetic resonance imaging-transrectal ultrasound fusion biopsy of benign lesions: recommendations for repeat sampling. J Urol. 2016; 196:62–67. PMID: 26880408.
Article13. Costa DN, Kay FU, Pedrosa I, Kolski L, Lotan Y, Roehrborn CG, et al. An initial negative round of targeted biopsies in men with highly suspicious multiparametric magnetic resonance findings does not exclude clinically significant prostate cancer-preliminary experience. Urol Oncol. 2017; 35:149.e15–149.e21.
Article14. Schimmöller L, Blondin D, Arsov C, Rabenalt R, Albers P, Antoch G, et al. MRI-guided in-bore biopsy: differences between prostate cancer detection and localization in primary and secondary biopsy settings. AJR Am J Roentgenol. 2016; 206:92–99. PMID: 26700339.
Article15. Penzkofer T, Tuncali K, Fedorov A, Song SE, Tokuda J, Fennessy FM, et al. Transperineal in-bore 3-T MR imaging-guided prostate biopsy: a prospective clinical observational study. Radiology. 2015; 274:170–180. PMID: 25222067.
Article16. Weinreb JC, Barentsz JO, Choyke PL, Cornud F, Haider MA, Macura KJ, et al. PI-RADS prostate imaging - reporting and data system: 2015, version 2. Eur Urol. 2016; 69:16–40. PMID: 26427566.
Article17. Roethke MC, Kuru TH, Schultze S, Tichy D, Kopp-Schneider A, Fenchel M, et al. Evaluation of the ESUR PI-RADS scoring system for multiparametric MRI of the prostate with targeted MR/TRUS fusion-guided biopsy at 3.0 Tesla. Eur Radiol. 2014; 24:344–352. PMID: 24196383.
Article18. Osses DF, van Asten JJ, Kieft GJ, Tijsterman JD. Prostate cancer detection rates of magnetic resonance imaging-guided prostate biopsy related to Prostate Imaging Reporting and Data System Score. World J Urol. 2017; 35:207–212. PMID: 27287889.
Article19. Felker ER, Lee-Felker SA, Feller J, Margolis DJ, Lu DS, Princenthal R, et al. In-bore magnetic resonance-guided transrectal biopsy for the detection of clinically significant prostate cancer. Abdom Radiol (NY). 2016; 41:954–962. PMID: 27118268.
Article20. Pokorny MR, de Rooij M, Duncan E, Schröder FH, Parkinson R, Barentsz JO, et al. Prospective study of diagnostic accuracy comparing prostate cancer detection by transrectal ultrasound-guided biopsy versus magnetic resonance (MR) imaging with subsequent MR-guided biopsy in men without previous prostate biopsies. Eur Urol. 2014; 66:22–29. PMID: 24666839.
Article21. Le Nobin J, Orczyk C, Deng FM, Melamed J, Rusinek H, Taneja SS, et al. Prostate tumour volumes: evaluation of the agreement between magnetic resonance imaging and histology using novel co-registration software. BJU Int. 2014; 114(6b):E105–E112. PMID: 24673731.
Article22. Fütterer JJ, Briganti A, De Visschere P, Emberton M, Giannarini G, Kirkham A, et al. Can clinically significant prostate cancer be detected with multiparametric magnetic resonance imaging? A systematic review of the literature. Eur Urol. 2015; 68:1045–1053. PMID: 25656808.
Article23. Abd-Alazeez M, Kirkham A, Ahmed HU, Arya M, Anastasiadis E, Charman SC, et al. Performance of multiparametric MRI in men at risk of prostate cancer before the first biopsy: a paired validating cohort study using template prostate mapping biopsies as the reference standard. Prostate Cancer Prostatic Dis. 2014; 17:40–46. PMID: 24126797.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Magnetic Resonance Imaging-Guided Prostate Biopsy: Present and Future
- MRI-Targeted Prostate Biopsy: What Radiologists Should Know
- MR-Guided Targeted Prostate Biopsy from Radiologists’ Perspective
- The Role of Magnetic Resonance Imaging (MRI) and MRI-Targeted Biopsy for Active Surveillance
- Magnetic resonance imaging-transrectal ultrasound fusion image-guided prostate biopsy: Current status of the cancer detection and the prospects of tailor-made medicine of the prostate cancer