Korean J Radiol.
2018 Aug;19(4):715-723. 10.3348/kjr.2018.19.4.715.
Association between Magnetic Resonance Imaging Findings of the Pelvic Floor and de novo Stress Urinary Incontinence after Vaginal Delivery
- Affiliations
-
- 1Department of Radiology, Tianjin Third Center Hospital, Tianjin 300070, China.
- 2Department of Radiology, Tianjin First Center Hospital, Tianjin 300192, China. shenwen66happy@163.com
- 3Department of Obstetrics and Gynecology, Tianjin First Center Hospital, Tianjin 300192, China.
- KMID: 2413700
- DOI: http://doi.org/10.3348/kjr.2018.19.4.715
Abstract
OBJECTIVE
The study aimed to evaluate the contributions of levator ani muscle (LAM) injury, vesical neck movement, urethral length and mobility, and urethral sphincter dysfunction observed on magnetic resonance imaging (MRI) towards stress urinary incontinence (SUI) after vaginal delivery.
MATERIALS AND METHODS
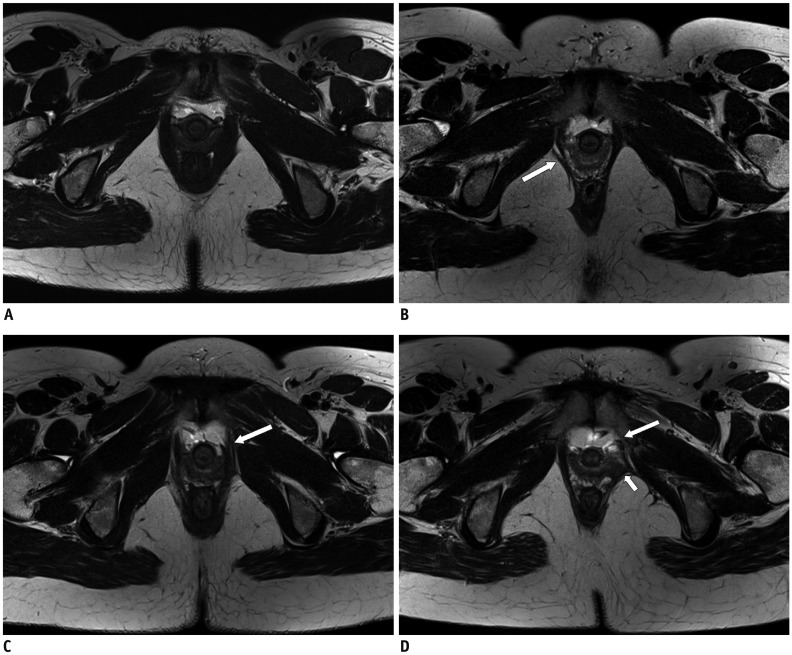
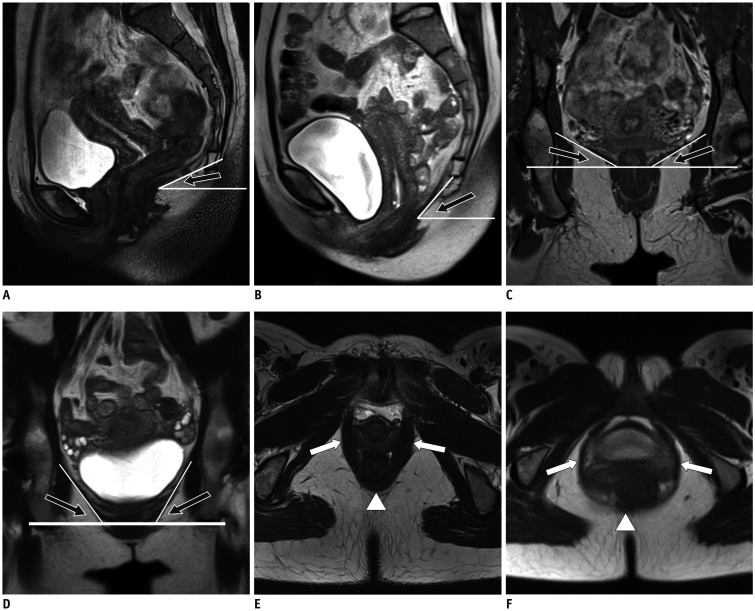
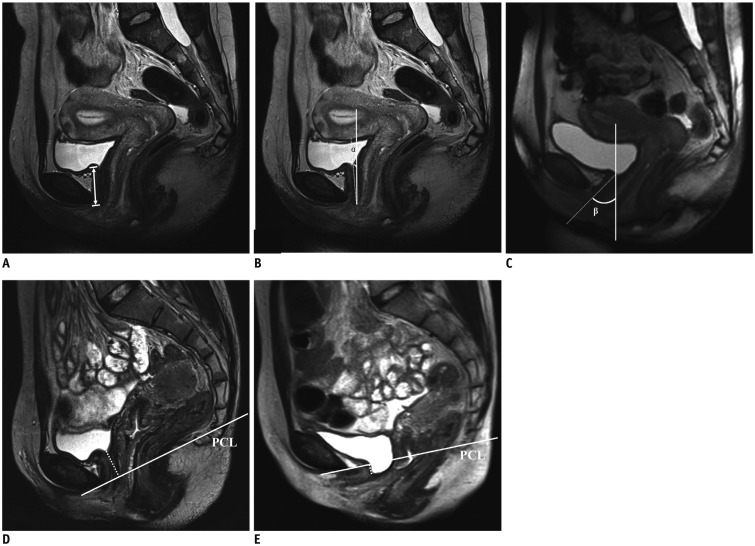
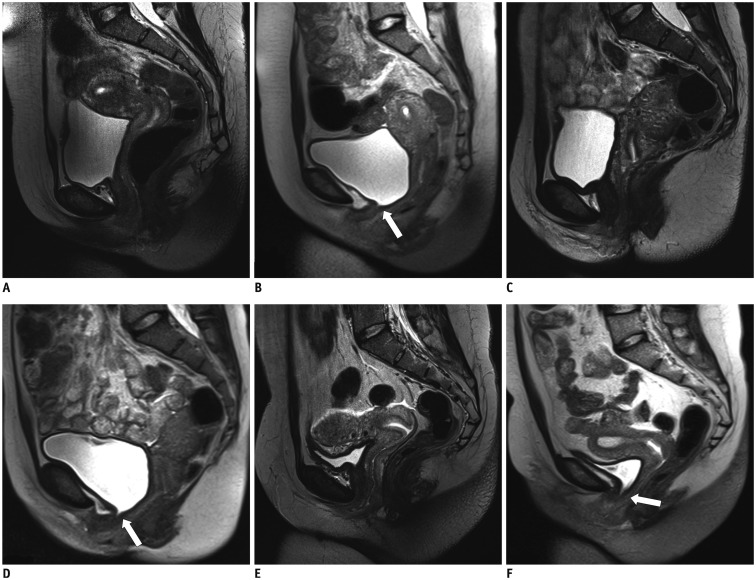
Fifty primiparous women after 6 months of delivery (15 with SUI and 35 without) and 35 nulliparous as continent controls underwent MRI at rest and Valsalva maneuver. A published levator ani scoring system was used to characterize morphological changes of LAM. The severity of the injury was divided into three categories as none, minor, and major. A series of common parameters including levator plate angle, iliococcygeal angle, and levator hiatus were used to describe the functional conditions of LAM. Urethral mobility was defined based on the rotation of the urethra between Valsalva and rest status. Vesical neck movement was evaluated by its distance to the pubococcygeal line. Urethral sphincter dysfunction was defined as the widening of the proximal urethra and/or funneling at the urethrovesical junction during Valsalva.
RESULTS
Primiparous incontinent (PI) women had additional major levator ani defects (33.3% vs. 17.1%) while less minor defects (0.7% vs. 31.4%) than primiparous continent (PC) women. Vesical neck downward movement in PI women was more obvious than PC women (28.5 mm vs. 24.2 mm, p = 0.006). Urethral mobility was more active in primiparous women than in nulliparous continent controls (57.4 vs. 52.4), whereas no difference was observed on urethral mobility in the primiparous group (p = 0.25). Urethral sphincter dysfunction and funneling were present in 80% of PI women versus 22.9% in PC women (p < 0.001).
CONCLUSION
The MRI findings revealed that de novo SUI was associated with major LAM injury, vesical neck downward movement as well as urethral sphincter dysfunction. Vesical neck funneling on sagittal images can be treated as a valuable predictor for SUI. The intervention for the PI should focus on the elevation of vesical neck, rehabilitation of LAM as well as recovery of the urethral sphincter muscle.
Keyword
MeSH Terms
Figure
Reference
-
1. Lukacz ES, Lawrence JM, Contreras R, Nager CW, Luber KM. Parity, mode of delivery, and pelvic floor disorders. Obstet Gynecol. 2006; 107:1253–1260. PMID: 16738149.
Article2. Rortveit G, Daltveit AK, Hannestad YS, Hunskaar S. Norwegian EPINCONT Study. Urinary incontinence after vaginal delivery or cesarean section. N Engl J Med. 2003; 348:900–907. PMID: 12621134.
Article3. Ashton-Miller JA, Howard D, DeLancey JO. The functional anatomy of the female pelvic floor and stress continence control system. Scand J Urol Nephrol Suppl. 2001; (207):1–7. discussion 106-125.4. Macura KJ, Genadry RR, Bluemke DA. MR imaging of the female urethra and supporting ligaments in assessment of urinary incontinence: spectrum of abnormalities. Radiographics. 2006; 26:1135–1149. PMID: 16844938.
Article5. Tunn R, Goldammer K, Neymeyer J, Gauruder-Burmester A, Hamm B, Beyersdorff D. MRI morphology of the levator ani muscle, endopelvic fascia, and urethra in women with stress urinary incontinence. Eur J Obstet Gynecol Reprod Biol. 2006; 126:239–245. PMID: 16298035.
Article6. Peschers U, Schaer G, Anthuber C, Delancey JO, Schuessler B. Changes in vesical neck mobility following vaginal delivery. Obstet Gynecol. 1996; 88:1001–1006. PMID: 8942842.
Article7. Dietz HP, Bennett MJ. The effect of childbirth on pelvic organ mobility. Obstet Gynecol. 2003; 102:223–228. PMID: 12907092.
Article8. DeLancey JO, Miller JM, Kearney R, Howard D, Reddy P, Umek W, et al. Vaginal birth and de novo stress incontinence: relative contributions of urethral dysfunction and mobility. Obstet Gynecol. 2007; 110(2 Pt 1):354–362. PMID: 17666611.9. Bergman A, McCarthy TA, Ballard CA, Yanai J. Role of the Q-tip test in evaluating stress urinary incontinence. J Reprod Med. 1987; 32:273–275. PMID: 3585870.10. DeLancey JO, Kearney R, Chou Q, Speights S, Binno S. The appearance of levator ani muscle abnormalities in magnetic resonance images after vaginal delivery. Obstet Gynecol. 2003; 101:46–53. PMID: 12517644.
Article11. Mostwin JL, Genadry R, Sanders R, Yang A. Anatomic goals in the correction of female stress urinary incontinence. J Endourol. 1996; 10:207–212. PMID: 8740379.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Assessment of Pelvic Floor Muscle Exercise using Vaginal Cone in Stress Urinary Incontinence of Korea Women
- Comparative Study of the Pelvic Floor Magnetic Stimulation with BIOCON-2000TM in Female Urinary Incontinence Patients
- MR Imaging of Pelvic Floor in Stress Urinary Incontinence
- The Efficacy of Pelvic Floor Muscle Exercise in Patients with Genuine Stress Incontinence
- The Difference of Pelvic Floor with Dynamic MRI before and after Tension Free Vaginal Tape Procedure in Female Stress Urinary Incontinence