J Pathol Transl Med.
2018 May;52(3):179-182. 10.4132/jptm.2017.10.09.
Duodenal Adenocarcinoma of Brunner Gland Origin: A Case Report
- Affiliations
-
- 1Department of Pathology, Seoul National University College of Medicine, Seoul, Korea. woohokim@snu.ac.kr
- 2Department of Surgery, Seoul National University College of Medicine, Seoul, Korea.
- 3Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2412930
- DOI: http://doi.org/10.4132/jptm.2017.10.09
Abstract
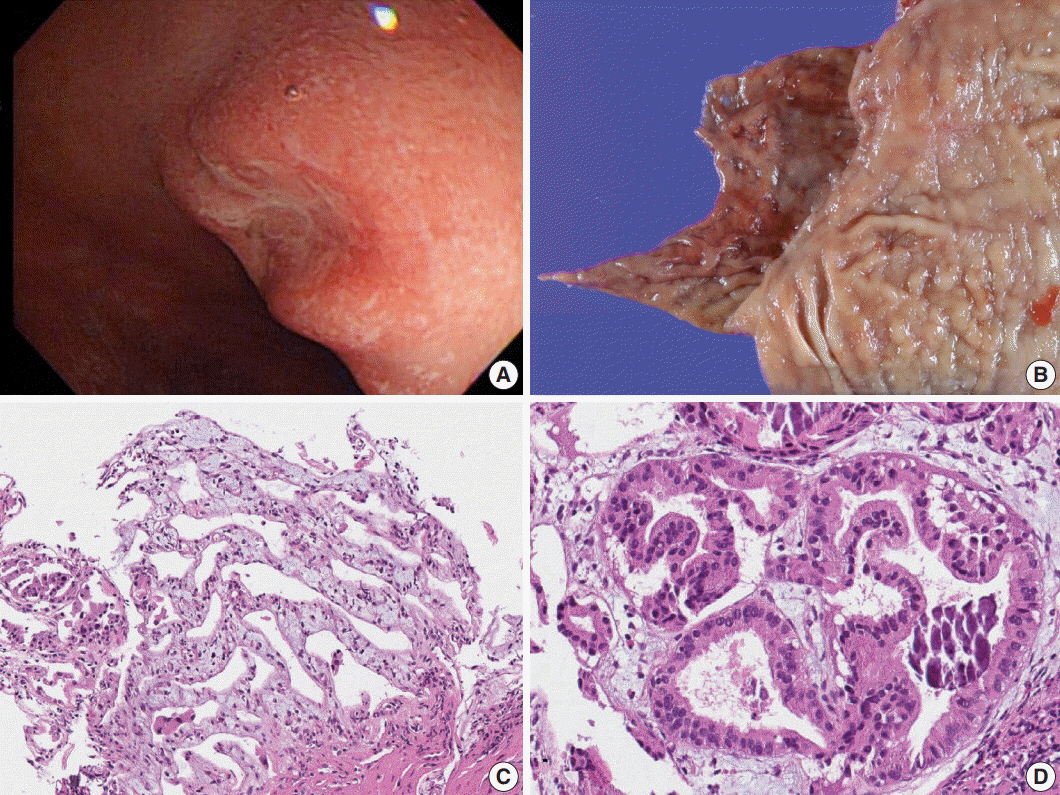
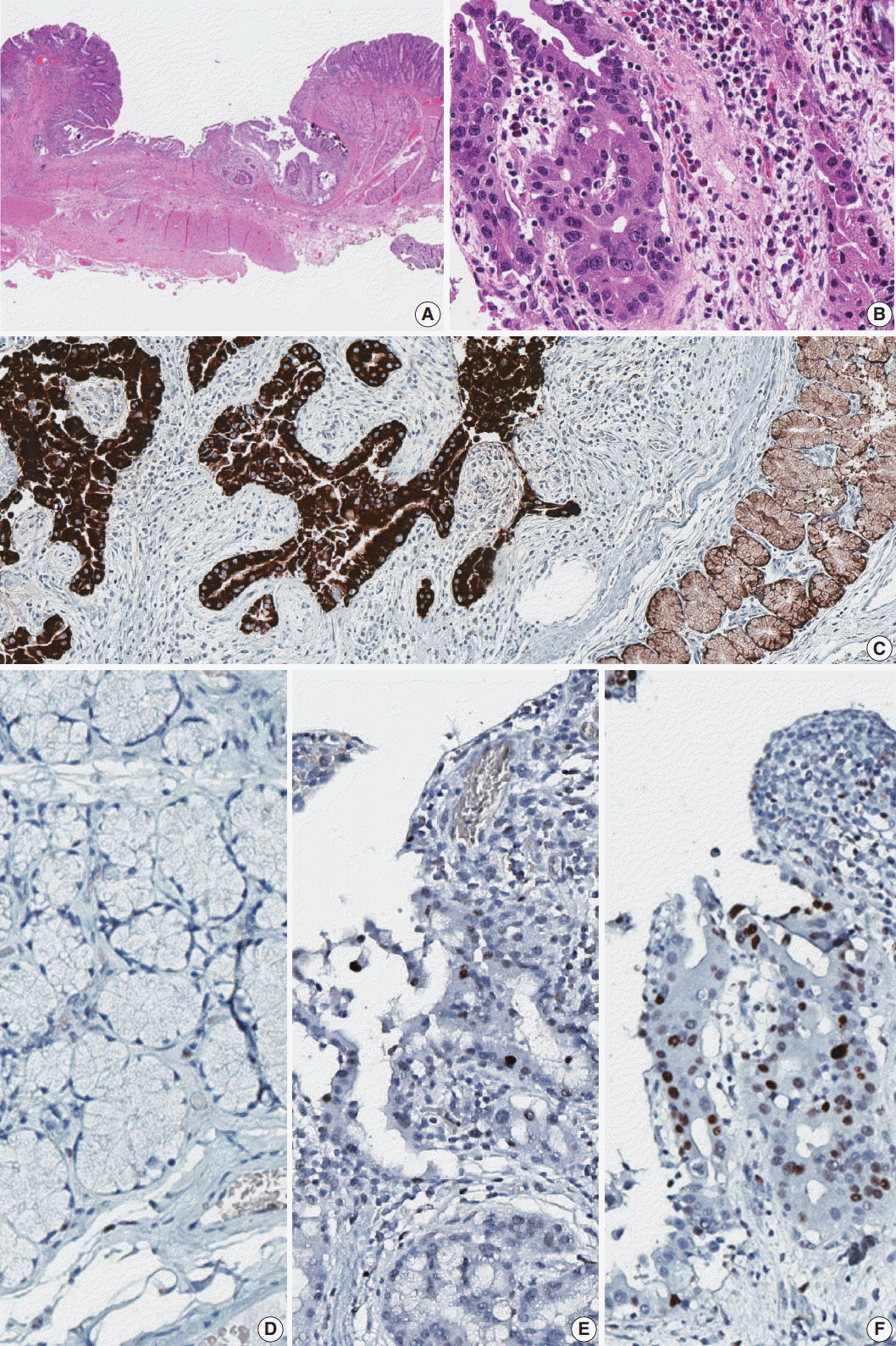
- We report a case of adenocarcinoma originating from the duodenal Brunner glands in a 47-year-old female patient. The lesion was 0.8 cm in extent and located at the posterior wall of the first part of the duodenum. Histologically, the tumor showed transition from non-neoplastic Brunner glands through dysplastic epithelium into adenocarcinoma. The carcinoma cells were strongly positive for MUC6 protein, which is an epithelial marker for the Brunner glands. Tumor protein p53 was overexpressed in the carcinoma cells, but not in the non-neoplastic or dysplastic epithelium. Dystrophic calcification was predominant. This is the first case report of duodenal adenocarcinoma of Brunner gland origin in Korea.
Keyword
Figure
Reference
-
1. Fenoglio-Preiser CM, Noffsinger AE, Stemmermann GN, Lantz PE, Isaacson PG. Gastrointestinal pathology: an atlas and text. Philadelphia: Lippincott Williams & Wilkins;2008. p. 471.2. Kamei K, Yasuda T, Nakai T, Takeyama Y. A case of adenocarcinoma of the duodenum arising from Brunner's gland. Case Rep Gastroenterol. 2013; 7:433–7.
Article3. Chang HK, Yu E, Kim J, et al. Adenocarcinoma of the small intestine: a multi-institutional study of 197 surgically resected cases. Hum Pathol. 2010; 41:1087–96.
Article4. Koizumi M, Sata N, Yoshizawa K, Kurihara K, Yasuda Y. Carcinoma arising from Brunner's gland in the duodenum after 17 years of observation: a case report and literature review. Case Rep Gastroenterol. 2007; 1:103–9.5. Ohta Y, Saitoh K, Akai T, Uesato M, Ochiai T, Matsubara H. Early primary duodenal carcinoma arising from Brunner's glands synchronously occurring with sigmoid colon carcinoma: report of a case. Surg Today. 2008; 38:756–60.
Article6. Kitagori K, Miyamoto S, Sakurai T. Image of the month: adenocarcinoma derived from Brunner's gland. Clin Gastroenterol Hepatol. 2010; 8:A26.7. Iwamuro M, Kobayashi S, Ohara N, Kawano S, Kawahara Y, Okada H. Adenocarcinoma in situ arising from Brunner's gland treated by endoscopic mucosal resection. Case Rep Gastrointest Med. 2017; 2017:7916976.
Article8. Kim K, Jang SJ, Song HJ, Yu E. Clinicopathologic characteristics and mucin expression in Brunner's gland proliferating lesions. Dig Dis Sci. 2013; 58:194–201.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sporadic Non-ampullary Duodenal Adenoma Overriding the Cystic Dilatation of Brunner's Gland Hyperplasia
- A Case of Brunner's Gland Hyperplasia of the Duodenal Second Portion with Annular Stricture Causing an Induced Obstruction
- A Brunner's Gland Adenoma Removed by Endoscopic Polypectomy
- Adenocarcinoma Arising from Brunner's Gland Hyperplasia
- A Case of Duodenal Brunner's Gland Adenoma Treated by Endoscopic Rescetion