Gender-related Differences in Management of Nonvalvular Atrial Fibrillation in an Asian Population
- Affiliations
-
- 1Division of Cardiology, Kyung Hee University Medical College, Seoul, Korea. jinbbai@khu.ac.kr
- 2Division of Cardiology, Severance Cardiovascular Hospital Yonsei University College of Medicine, Seoul, Korea. cby6908@yuhs.ac
- 3Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea.
- 4Department of Cardiology, College of Medicine, Ewha Womans University, Seoul, Korea.
- 5Division of Cardiology, Hanyang University Medical Center, Seoul, Korea.
- 6Division of Cardiology, Eulji University Hospital, Daejeon, Korea.
- 7Division of Cardiology, Korea University Anam Hospital, Seoul, Korea.
- 8Department of Internal Medicine, University of Ulsan College of Medicine, Seoul, Korea.
- 9Department of Cardiovascular Medicine, Chonnam National University Medical School, Gwangju, Korea.
- 10Division of Cardiology, Catholic University of Daegu, Daegu, Korea.
- 11Department of Preventive Medicine, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2412545
- DOI: http://doi.org/10.4070/kcj.2017.0389
Abstract
- BACKGROUND AND OBJECTIVES
Gender-related differences in health care utilization for atrial fibrillation (AF) are increasingly recognized. However, large cohort data for examining gender-related differences in AF are lacking in Asian populations.
METHODS
The Registry for Comparison Study of Drugs for Symptom Control and Complication Prevention of AF (CODE-AF Registry) is a prospective observational cohort-study that enrolled participants at 10 tertiary hospitals in South Korea. Baseline characteristics retrieved from the CODE-AF Registry were analyzed.
RESULTS
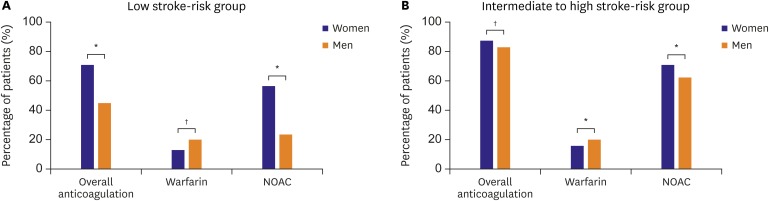
A total of 6,274 patients were recruited (mean age 67±11 years, mean CHA2DS2-VASc score 2.7±1.7, 63% male, 65% paroxysmal AF) from June 2016 to April 2017. Women underwent less electric cardioversion (12.3% vs. 19.6%, p < 0.001), less radiofrequency ablation (12.4% vs. 17.9%, p < 0.001), and less antiarrhythmic drug therapy (44.7% vs. 49.5%, p < 0.001), despite having more severe symptoms (symptom class III or IV, 45.8% vs. 37.5%, p < 0.001). Among patients with a CHA2DS2-VA score of 2 or more, a slightly higher proportion of women were taking oral anticoagulants than men (85.7% vs. 81.9%, p=0.002), and non-vitamin K antagonist oral anticoagulant (NOAC) use was more prevalent in women than men (70.4% vs. 62.3%, p < 0.001). Insufficient NOAC dosing was very common, more so in women than men (61.5% vs. 56.3%, p < 0.001).
CONCLUSIONS
Female patients with AF were treated more conservatively and rhythm control strategies were used less frequently than in males, even though the female patients with AF had more severe symptoms. While insufficient NOAC dosing was common in both sex, it was significantly more frequent in women.
Keyword
MeSH Terms
Figure
Cited by 4 articles
-
Increased Hb Levels Are Associated with the Incidence of Atrial Fibrillation: But Is It Related to the Occurrence of Stroke?
Junbeom Park
Korean Circ J. 2020;50(12):1111-1112. doi: 10.4070/kcj.2020.0495.Gender Issues in Medical Decisions: Implicit Stereotyping and Unconscious Bias
Gi-Byoung Nam
Korean Circ J. 2018;48(6):529-531. doi: 10.4070/kcj.2018.0151.The Role of Novel Oral Anticoagulants and Antiplatelet Therapy after Percutaneous Coronary Intervention: Individualizing Therapy to Optimize Outcomes
Evan Shlofmitz, Richard Shlofmitz, Michael S. Lee
Korean Circ J. 2019;49(8):645-656. doi: 10.4070/kcj.2019.0185.Association of Gender With Clinical Outcomes in a Contemporary Cohort of Patients With Atrial Fibrillation Receiving Oral Anticoagulants
Minjeong Kim, Jun Kim, Jin-Bae Kim, Junbeom Park, Jin-Kyu Park, Ki-Woon Kang, Jaemin Shim, Eue-Keun Choi, Young Soo Lee, Hyung Wook Park, Boyoung Joung
Korean Circ J. 2022;52(8):593-603. doi: 10.4070/kcj.2021.0399.
Reference
-
1. Gillis AM. Atrial fibrillation and ventricular arrhythmias: sex differences in electrophysiology, epidemiology, clinical presentation, and clinical outcomes. Circulation. 2017; 135:593–608. PMID: 28153995.2. Ko D, Rahman F, Martins MA, et al. Atrial fibrillation in women: treatment. Nat Rev Cardiol. 2017; 14:113–124. PMID: 27786235.3. Lip GY, Laroche C, Boriani G, et al. Sex-related differences in presentation, treatment, and outcome of patients with atrial fibrillation in Europe: a report from the Euro Observational Research Programme Pilot survey on Atrial Fibrillation. Europace. 2015; 17:24–31. PMID: 24957921.4. Rienstra M, Van Veldhuisen DJ, Hagens VE, et al. Gender-related differences in rhythm control treatment in persistent atrial fibrillation: data of the Rate Control Versus Electrical Cardioversion (RACE) study. J Am Coll Cardiol. 2005; 46:1298–1306. PMID: 16198847.5. Shantsila E, Wolff A, Lip GY, Lane DA. Gender differences in stroke prevention in atrial fibrillation in general practice: using the GRASP-AF audit tool. Int J Clin Pract. 2015; 69:840–845. PMID: 25752615.6. Piccini JP, Simon DN, Steinberg BA, et al. Differences in clinical and functional outcomes of atrial fibrillation in women and men: two-year results from the ORBIT-AF Registry. JAMA Cardiol. 2016; 1:282–291. PMID: 27438106.7. Vallakati A, Reddy M, Sharma A, et al. Impact of gender on outcomes after atrial fibrillation ablation. Int J Cardiol. 2015; 187:12–16. PMID: 25828301.8. Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991; 22:983–988. PMID: 1866765.9. Andersson T, Magnuson A, Bryngelsson IL, et al. Gender-related differences in risk of cardiovascular morbidity and all-cause mortality in patients hospitalized with incident atrial fibrillation without concomitant diseases: a nationwide cohort study of 9519 patients. Int J Cardiol. 2014; 177:91–99. PMID: 25499348.10. Friberg L, Benson L, Rosenqvist M, Lip GY. Assessment of female sex as a risk factor in atrial fibrillation in Sweden: nationwide retrospective cohort study. BMJ. 2012; 344:e3522. PMID: 22653980.11. Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009; 361:1139–1151. PMID: 19717844.12. Giugliano RP, Ruff CT, Braunwald E, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013; 369:2093–2104. PMID: 24251359.13. Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011; 365:981–992. PMID: 21870978.14. Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011; 365:883–891. PMID: 21830957.15. Kim H, Kim TH, Cha MJ, et al. A prospective survey of atrial fibrillation management for real-world guideline adherence: COmparison study of Drugs for symptom control and complication prEvention of Atrial Fibrillation (CODE-AF) Registry. Korean Circ J. 2017; 47:877–887. PMID: 29171211.16. January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014; 64:e1–e76. PMID: 24685669.17. Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010; 138:1093–1100. PMID: 20299623.18. Friberg L, Rosenqvist M, Lip GY. Evaluation of risk stratification schemes for ischaemic stroke and bleeding in 182 678 patients with atrial fibrillation: the Swedish Atrial Fibrillation cohort study. Eur Heart J. 2012; 33:1500–1510. PMID: 22246443.19. Tomita H, Okumura K, Inoue H, et al. Validation of risk scoring system excluding female sex from CHA2DS2-VASc in Japanese patients with nonvalvular atrial fibrillation - subanalysis of the J-RHYTHM Registry. Circ J. 2015; 79:1719–1726. PMID: 25971525.20. Okumura K, Inoue H, Atarashi H, et al. Validation of CHA(2)DS(2)-VASc and HAS-BLED scores in Japanese patients with nonvalvular atrial fibrillation: an analysis of the J-RHYTHM Registry. Circ J. 2014; 78:1593–1599. PMID: 24759791.21. Suzuki S, Yamashita T, Okumura K, et al. Incidence of ischemic stroke in Japanese patients with atrial fibrillation not receiving anticoagulation therapy--pooled analysis of the Shinken Database, J-RHYTHM Registry, and Fushimi AF Registry. Circ J. 2015; 79:432–438. PMID: 25501800.22. Lee JM, Kim JB, Uhm JS, Pak HN, Lee MH, Joung B. Additional value of left atrial appendage geometry and hemodynamics when considering anticoagulation strategy in patients with atrial fibrillation with low CHA2DS2-VASc scores. Heart Rhythm. 2017; 14:1297–1301. PMID: 28559088.23. Cooke FL. Women’s participation in employment in Asia: a comparative analysis of China, India, Japan and South Korea. Int J Hum Resour Manage. 2010; 21:2249–2270.24. Patterson L, Walcutt B. Korean workplace gender discrimination research analysis: a review of the literature from 1990 to 2010. Asia Pac Bus Rev. 2013; 19:85–101.25. Hsu JC, Maddox TM, Kennedy K, et al. Aspirin instead of oral anticoagulant prescription in atrial fibrillation patients at risk for stroke. J Am Coll Cardiol. 2016; 67:2913–2923. PMID: 27339487.26. Lip GY, Rushton-Smith SK, Goldhaber SZ, et al. Does sex affect anticoagulant use for stroke prevention in nonvalvular atrial fibrillation? The prospective global anticoagulant registry in the FIELD-Atrial Fibrillation. Circ Cardiovasc Qual Outcomes. 2015; 8:S12–S20. PMID: 25714828.27. Perino AC, Fan J, Schmitt SK, et al. Treating specialty and outcomes in newly diagnosed atrial fibrillation: from the TREAT-AF Study. J Am Coll Cardiol. 2017; 70:78–86. PMID: 28662810.28. Steinberg BA, Shrader P, Thomas L, et al. Factors associated with non-vitamin K antagonist oral anticoagulants for stroke prevention in patients with new-onset atrial fibrillation: results from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation II (ORBIT-AF II). Am Heart J. 2017; 189:40–47. PMID: 28625380.29. Avgil Tsadok M, Jackevicius CA, Rahme E, Humphries KH, Pilote L. Sex Differences in dabigatran use, safety, and effectiveness in a population-based cohort of patients with atrial fibrillation. Circ Cardiovasc Qual Outcomes. 2015; 8:593–599. PMID: 26508666.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Application of New Oral Anticoagulants: Prevention of Stroke in Patients with Nonvalvular Atrial Fibrillation
- A Comparative Study on Cerebral Infarction in Patient with Nonvalvular and Valvular Atrial Fibrillation
- Hemoptysis in Quadriplegia with Atrial Fibrillation Who Was Taking Edoxaban: a Case Report
- Pharmacological Treatment of Atrial Fibrillation
- Pathophysiology and Diagnosis in Atrial Fibrillation