Ann Hepatobiliary Pancreat Surg.
2018 May;22(2):128-135. 10.14701/ahbps.2018.22.2.128.
Oncologic outcomes after radical surgery for periampullary cancer in octogenarians
- Affiliations
-
- 1Department of Hepatobiliary and Pancreatic Surgery, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. KSKIM88@yuhs.ac
- 2Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2412427
- DOI: http://doi.org/10.14701/ahbps.2018.22.2.128
Abstract
- BACKGROUNDS/AIMS
Interest in treatments for elderly patients has increased with life expectancy, and various studies have reported on the safety and feasibility of radical surgery in elderly patients with cancer. Here, we investigated oncologic outcomes of periampullary cancer in octogenarians.
METHODS
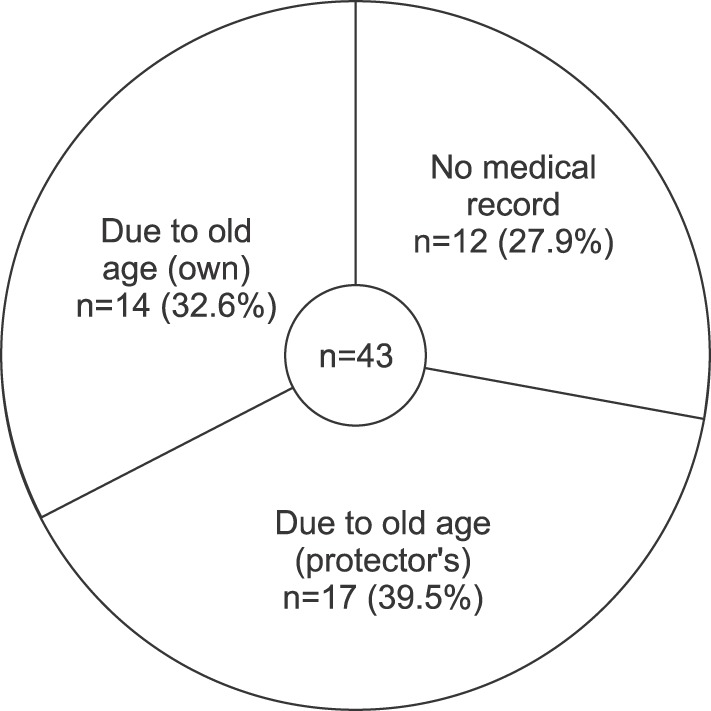
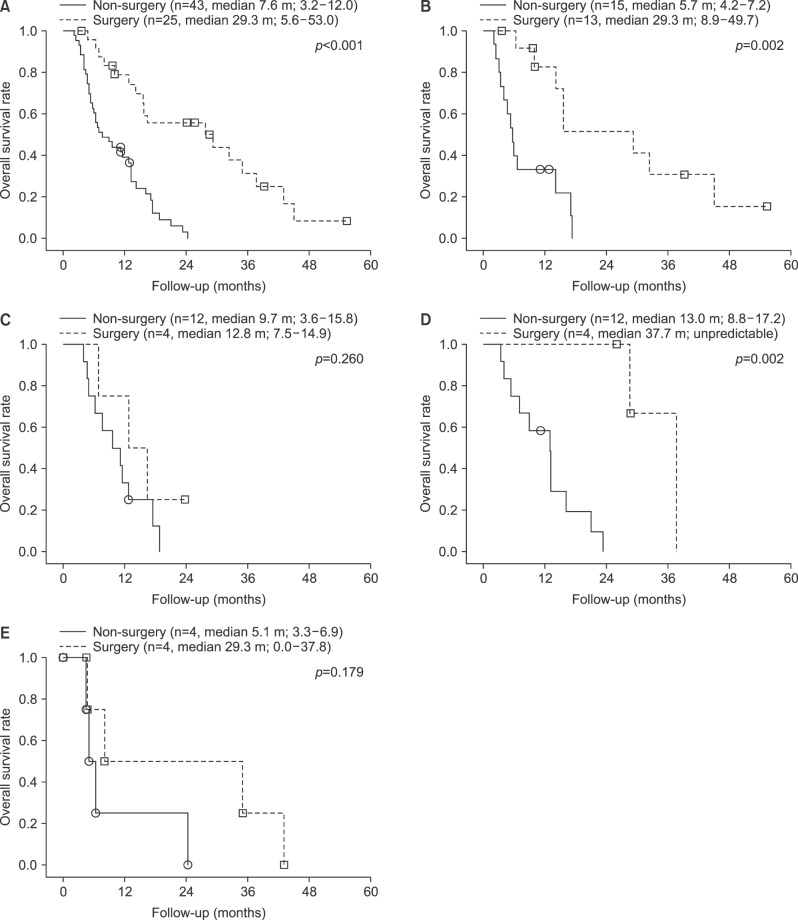
We retrospectively reviewed medical records of 68 patients over 80 years of age who were diagnosed with periampullary cancer and were eligible for surgery; we analyzed overall survival (OS) and immediate postoperative complications and mortality.
RESULTS
There were no significant differences in mean age, disease type, oncologic features, comorbidities, or nutritional status between the patients who had surgery and those who did not. Five patients (20.0%) had major postoperative complications, but there was no immediate postoperative mortality. Patients who had surgery (n=25) had better OS (29.3 months; 95% confidence interval [CI]: 5.6-53.0) than did those who did not (n=43, OS: 7.6 months; 95% CI: 3.2-12.0 months; p<0.001). Similarly, patients with distal common bile duct cancer who underwent surgery had better OS than those who did not (surgery group: n=13, OS: 29.3 months, 95% CI: 8.9-49.7; non-surgery group: n=15, OS: 5.7 months, 95% CI: 4.2-7.2 months; p=0.002).
CONCLUSIONS
Radical surgery for octogenarian patients with periampullary cancer is safe, feasible, and expected to result in better survival outcomes, especially for patients with common bile duct cancer.
MeSH Terms
Figure
Reference
-
1. Mathers CD, Stevens GA, Boerma T, White RA, Tobias MI. Causes of international increases in older age life expectancy. Lancet. 2015; 385:540–548. PMID: 25468166.
Article2. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015; 65:5–29. PMID: 25559415.
Article3. Seishima R, Okabayashi K, Hasegawa H, Tsuruta M, Shigeta K, Matsui S, et al. Is laparoscopic colorectal surgery beneficial for elderly patients? A systematic review and meta-analysis. J Gastrointest Surg. 2015; 19:756–765. PMID: 25617077.
Article4. Kwon IG, Cho I, Guner A, Kim HI, Noh SH, Hyung WJ. Minimally invasive surgery as a treatment option for gastric cancer in the elderly: comparison with open surgery for patients 80 years and older. Surg Endosc. 2015; 29:2321–2330. PMID: 25480603.5. Kishida N, Hibi T, Itano O, Okabayashi K, Shinoda M, Kitago M, et al. Validation of hepatectomy for elderly patients with hepatocellular carcinoma. Ann Surg Oncol. 2015; 22:3094–3101. PMID: 25582743.
Article6. Lee CR, Lim JH, Kim SH, Ahn SH, Park YN, Choi GH, et al. A comparative analysis of hepatocellular carcinoma after hepatic resection in young versus elderly patients. J Gastrointest Surg. 2012; 16:1736–1743. PMID: 22810298.
Article7. Haigh PI, Bilimoria KY, DiFronzo LA. Early postoperative outcomes after pancreaticoduodenectomy in the elderly. Arch Surg. 2011; 146:715–723. PMID: 21690449.
Article8. Lee DY, Schwartz JA, Wexelman B, Kirchoff D, Yang KC, Attiyeh F. Outcomes of pancreaticoduodenectomy for pancreatic malignancy in octogenarians: an American College of Surgeons National Surgical Quality Improvement Program analysis. Am J Surg. 2014; 207:540–548. PMID: 24560585.
Article9. Turrini O, Paye F, Bachellier P, Sauvanet A, Sa Cunha A, Le Treut YP, et al. Pancreatectomy for adenocarcinoma in elderly patients: postoperative outcomes and long term results: a study of the French Surgical Association. Eur J Surg Oncol. 2013; 39:171–178. PMID: 22999411.10. de la Fuente SG, Bennett KM, Pappas TN, Scarborough JE. Preand intraoperative variables affecting early outcomes in elderly patients undergoing pancreaticoduodenectomy. HPB (Oxford). 2011; 13:887–892. PMID: 22081925.11. Buchbjerg T, Fristrup C, Mortensen MB. The incidence and prognosis of true duodenal carcinomas. Surg Oncol. 2015; 24:110–116. PMID: 25936244.
Article12. Jepsen P, Vilstrup H, Tarone RE, Friis S, Sørensen HT. Incidence rates of intra- and extrahepatic cholangiocarcinomas in Denmark from 1978 through 2002. J Natl Cancer Inst. 2007; 99:895–897. PMID: 17551150.
Article13. Cameron JL, Riall TS, Coleman J, Belcher KA. One thousand consecutive pancreaticoduodenectomies. Ann Surg. 2006; 244:10–15. PMID: 16794383.
Article14. Bilimoria KY, Bentrem DJ, Ko CY, Stewart AK, Winchester DP, Talamonti MS. National failure to operate on early stage pancreatic cancer. Ann Surg. 2007; 246:173–180. PMID: 17667493.
Article15. Fernández-del Castillo C, Rattner DW, Warshaw AL. Standards for pancreatic resection in the 1990s. Arch Surg. 1995; 130:295–299. PMID: 7887797.
Article16. Tempero MA, Malafa MP, Behrman SW, Benson AB 3rd, Casper ES, Chiorean EG, et al. Pancreatic adenocarcinoma, version 2.2014: featured updates to the NCCN guidelines. J Natl Compr Canc Netw. 2014; 12:1083–1093. PMID: 25099441.17. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213. PMID: 15273542.18. Homeier D. Aging: physiology, disease, and abuse. Clin Geriatr Med. 2014; 30:671–686. PMID: 25439635.19. Hoffe S, Balducci L. Cancer and age: general considerations. Clin Geriatr Med. 2012; 28:1–18. PMID: 22326032.
Article20. Balducci L, Ershler WB. Cancer and ageing: a nexus at several levels. Nat Rev Cancer. 2005; 5:655–662. PMID: 16056261.
Article21. Boyd CM, Darer J, Boult C, Fried LP, Boult L, Wu AW. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. JAMA. 2005; 294:716–724. PMID: 16091574.22. Kilari D, Mohile SG. Management of cancer in the older adult. Clin Geriatr Med. 2012; 28:33–49. PMID: 22326034.
Article23. Extermann M, Hurria A. Comprehensive geriatric assessment for older patients with cancer. J Clin Oncol. 2007; 25:1824–1831. PMID: 17488980.
Article24. Corre R, Greillier L, Le Caër H, Audigier-Valette C, Baize N, Bérard H, et al. Use of a comprehensive geriatric assessment for the management of elderly patients with advanced non-small-cell lung cancer: the phase III randomized ESOGIA-GFPC-GECP 08-02 study. J Clin Oncol. 2016; 34:1476–1483. PMID: 26884557.
Article25. Girre V, Falcou MC, Gisselbrecht M, Gridel G, Mosseri V, Bouleuc C, et al. Does a geriatric oncology consultation modify the cancer treatment plan for elderly patients? J Gerontol A Biol Sci Med Sci. 2008; 63:724–730. PMID: 18693227.
Article26. Zbar AP, Gravitz A, Audisio RA. Principles of surgical oncology in the elderly. Clin Geriatr Med. 2012; 28:51–71. PMID: 22326035.
Article27. Kuzu MA, Terzioğlu H, Genç V, Erkek AB, Ozban M, Sonyürek P, et al. Preoperative nutritional risk assessment in predicting postoperative outcome in patients undergoing major surgery. World J Surg. 2006; 30:378–390. PMID: 16479353.
Article28. Casadei R, Zanini N, Morselli-Labate AM, Calculli L, Pezzilli R, Potì O, et al. Prognostic factors in periampullary and pancreatic tumor resection in elderly patients. World J Surg. 2006; 30:1992–2001. PMID: 16957825.
Article29. Abd-El-Gawad WM, Abou-Hashem RM, El Maraghy MO, Amin GE. The validity of Geriatric Nutrition Risk Index: simple tool for prediction of nutritional-related complication of hospitalized elderly patients. Comparison with Mini Nutritional Assessment. Clin Nutr. 2014; 33:1108–1116. PMID: 24418116.
Article30. PACE participants. Audisio RA, Pope D, Ramesh HS, Gennari R, van Leeuwen BL, et al. Shall we operate? Preoperative assessment in elderly cancer patients (PACE) can help. A SIOG surgical task force prospective study. Crit Rev Oncol Hematol. 2008; 65:156–163. PMID: 18082416.31. Prytherch DR, Whiteley MS, Higgins B, Weaver PC, Prout WG, Powell SJ. POSSUM and Portsmouth POSSUM for predicting mortality. Physiological and Operative Severity Score for the enUmeration of Mortality and morbidity. Br J Surg. 1998; 85:1217–1220. PMID: 9752863.32. Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011; 173:676–682. PMID: 21330339.
Article33. Barbas AS, Turley RS, Ceppa EP, Reddy SK, Blazer DG 3rd, Clary BM, et al. Comparison of outcomes and the use of multimodality therapy in young and elderly people undergoing surgical resection of pancreatic cancer. J Am Geriatr Soc. 2012; 60:344–350. PMID: 22211710.
Article34. Oliveira-Cunha M, Malde DJ, Aldouri A, Morris-Stiff G, Menon KV, Smith AM. Results of pancreatic surgery in the elderly: is age a barrier? HPB (Oxford). 2013; 15:24–30. PMID: 23216776.35. de Franco V, Frampas E, Wong M, Meurette G, Charvin M, Leborgne J, et al. Safety and feasibility of pancreaticoduodenectomy in the elderly: a matched study. Pancreas. 2011; 40:920–924. PMID: 21747313.36. Stauffer JA, Grewal MS, Martin JK, Nguyen JH, Asbun HJ. Pancreas surgery is safe for octogenarians. J Am Geriatr Soc. 2011; 59:184–186. PMID: 21226703.
Article37. Khan S, Sclabas G, Lombardo KR, Sarr MG, Nagorney D, Kendrick ML, et al. Pancreatoduodenectomy for ductal adenocarcinoma in the very elderly; is it safe and justified? J Gastrointest Surg. 2010; 14:1826–1831. PMID: 20714937.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pancreatoduodenectomy with uncut-Roux-en-Y reconstruction in patients with previous radical gastrectomy
- Surgical outcomes and prognostic factors of gastric cancer surgery in octogenarians
- Comparison of Surgical Outcomes and Survival between Octogenarians and Younger Patients after Pulmonary Resection for Stage I Lung Cancer
- Safe and feasible outcomes of cholecystectomy in extremely elderly patients (octogenarians vs. nonagenarians)
- Long-term oncologic outcomes of neoadjuvant concurrent chemoradiotherapy with capecitabine and radical surgery in locally advanced rectal cancer: 10-year experiences at a single institution